Introduction: Human infertility is a complex global health problem. It has multiple social consequences which are especially profound for thyroid hormones in infertility with the aim of determining the degree of association of thyroid hormones with hyperprolactinemia in our population.
Materials and Methods: The serum levels of prolactin, T3, T4 and TSH were determined in 90 hyperprolactinemic infertile women, 90 normoprolactinemic infertile women and 50 fertile women. The hormones were assayed using Enzyme Linked Immunosorbent Assay kits.
Statistical Analysis: Analysis of variance and Pearson’s correlation were used to analyze the data, with the significant p-level set at 0.05.
Results: A significantly higher mean serum prolactin and TSH were observed among the infertile groups compared to the fertile controls (p<0.05). The mean serum T3 and T4 were significantly lower in the hyperprolactinemic infertile women compared to the fertile controls (p<0.05). The mean TSH and T3 of normoprolactinemic infertile women and controls were comparable (p>0.05). However, the mean T4 was significantly lower in normoprolactinemic infertile women compared to the fertile controls (p<0.05). In all the groups, TSH correlated inversely with T3 and T4, while T3 correlated positively with T4. It was only in the control group that prolactin correlated positively and significantly with TSH.
Conclusion: It is therefore concluded that hyperprolactinemia with thyroid dysfunction may be a major contributory hormonal factor in infertility among infertile women and as such, estimation of prolactin, T3, T4 and TSH should be included in the workup for infertile women especially those with hyperprolactinaemia.
Introduction
Infertility is defined as the failure of a couple to achieve conception (regardless of cause) after one year of unprotected and adequately timed intercourse [1]. It could be primary i.e. when a couple has never conceived despite cohabitation and exposure to sexual activity over a period of two years or secondary infertility i.e. when a couple have achieved a pregnancy previously but regular unprotected sexual intercourse has not resulted in a second pregnancy [2].
Human infertility is a complex problem, which has numerous consequences depending on the society and cultural background, gender, lifestyle, sexual history, of the people it affects. Infertility is a global public health concern this is partly due to its complexity in aetiology as well as difficulty in preventing, diagnosing and treating it [2]. Although infertility is considered by some as primarily a woman’s problem, men often contribute to and are also affected [3].
It has been estimated by WHO that 8-12% of couples around the world experience problems in conception. The consequences of childlessness in developing countries range from economic hardship, social stigmatization, violence and even denial of proper burial rites [4]. Other consequences include psychological disturbances social stigma and strain on relationships between husbands and wives [5]. Compared to their male counterparts, available evidence suggests that the social consequences of infertility are profound for African women [6]. Regardless of the cause of infertility, they receive major blame for the reproductive delay and suffer personal grief and frustration, social stigma, isolation and serious social and economic deprivation [7]. Nigeria with a population of over 150 million people has a high population growth rate and also a high rate of fertility, 5.53 births per woman in 2011 [8]. Available evidence also suggests that the country has high rates of primary and secondary infertility. About 40% of all cases of infertility are due to problems with the female partner and another 30% are due to problems in the male partner. The rest of the remaining 30% of cases are due either to a cause which affects both the partners or to a cause which cannot be identified [9].
The main causes of female infertility include ovulatory disorders, pelvic inflammatory disease (PID), endometriosis, polycystic ovarian syndrome, advanced age, environmental and occupational exposure to chemicals, congenital abnormalities and hormonal imbalance [1,10].
Prolactin is defined as a pituitary-secreted polypeptide hormone which was named for its stimulatory action on lactation. Its primary function is to enhance breast development during pregnancy and to induce lactation [11]. Measurement of prolactin is usually included in the differential work up for female patients who present with amenorrhea, oligomenorrhoea, galactorrhea, or infertility or for male patients who present with sexual dysfunction. However, its secretion is pulsatile; it increases with sleep, stress, pregnancy, and chest wall stimulation or trauma [11]. Hyperprolactinemia is defined as circulating prolactin levels above normal range, which occurs in conditions other than pregnancy and lactation, when physiological hyperprolactinemia occurs [12]. Even in the absence of hyperprolactinaemia, hypothyroidism can contribute to infertility. This is because thyroid hormones are necessary for maximum production of both progesterone and estradiol [13].
A close interplay between normal steroid action and secretion and thyroid hormones exists. This is necessary for normal ovarian function and consequently, fertility [14]. We hope that our findings will further clarify the role thyroid hormones should play in diagnosing female infertility. The aim of this study is to assess the levels of serum prolactin and thyroid hormones in infertility and determine if there is any association between thyroid hormones levels and hyperprolactinemia in our population.
Materials and Methods
Selection of subjects
A total of 230 women of Nigerian origin participated in the study. Out of this number, 180 were attending the Gynaecology clinic of University of Calabar Teaching Hospital were used as subjects. Ninety of them had confirmed hyperprolactinenia with infertility while the other 90 were normoprolactinemic but infertile. Fifty apparently healthy women with proven fertility (who have had at least one child in the last 2 y) and normoprolactinemic were used as controls. Ethical approval was obtained from the ethics committee of the University of Calabar Teaching Hospital, Calabar. A standard questionnaire was administered to them and their consent to participate in the study obtained.
Sample size calculation
The number of sample in this research was determined using the formular of Ejemot-Nwadiaro [15]

where N = desired sample size
Zα = the α level of the coefficient interval at 95% (1.96)
p = proportion of non-occurrence
q = (1-p) proportion of non occurencence
d= precision
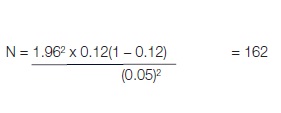
Substituting the expected occurrence of p= 12% i.e. 0.12 from WHO [4] we have
Sample collection: Venous blood (5ml) was aseptically collected from the infertile and fertile women by venepunture and dispensed into clean plain bottles, allowed to clot, retracted and centrifuged at 5000 revolution per minute (rpm) for 5 min. The serum obtained was separated and frozen till used for prolactin and thyroid function assay (TSH, T3 and T4 assay).
Assays: The assays used in the study were Prolactin, TSH, T3 and T4, these were analyzed using ELISA kits obtained from DRG International Incorporated, East Mountain Side, USA. Prolactin and TSH assays were based on solid phase enzyme-linked immunosorbent assay; T3 on sandwich enzyme-linked immunosorbent assay; and T4 on competitive binding enzyme-linked immunosorbent assay. A microwell reader was used for the measurement of absorbance of the samples at 450nm. No significant variations in results was observed when samples were analyzed immediately and after storage with this method. Expected normal values for T3 were 60 -210.0ng/ml; T4 were 5 – 13 μg/ml, TSH were 0.5 – 4.1 μlu/ml for adults and prolactin were 8.39 – 20.15ng/ml for adult females.
Statistical Analysis
Analysis of variance and Pearson’s correlation were used to analyze the data, with the significant p-level set at 0.05. This was done using the PAWstatistic 18, a statistical package from SPSS Inc, California, USA.
Results
A comparison of mean values of age, prolactin, TSH, T3 and T4 of hyperprolactinaemic infertile women, normoprolactinaemic infertile women and controls, showed that was no significant 14variations in mean value of age (p>0.05). However, there were significant variations in the mean values of prolactin TSH, T3 and T4 among the groups. The mean values of prolactin and TSH of the hyperprolactinaemic infertile women were significantly higher (p<0.05) than those of the controls. However, the mean values of T3 and T4 of the hyperprolactinaemic infertile women were significantly lower (p<0.05) than those of controls. Similar observations were made when values for the hyperprolactinaemic infertile women were compared with those of normoprolactinaemic infertile women. There were no significant differences (p>0.05) in the mean values of TSH and T3 between the normoprolactinaemic infertile women and controls. The mean levels of T4, however, was significantly lower (p<0.05) in the normoprolactinaemic infertile women compared to the controls. The mean prolactin levels was significantly higher (p<0.05) in normoprolactinemic infertile women compared to the controls [Table/Fig-1].
Among the controls, prolactin correlated significantly with TSH (r=0.3045, p=0.031), there was no significant correlation between prolactin and T3 and T4 [Table/Fig-2]. However, there was no correlation between prolactin on one hand and TSH, T3 and T4 on the other in both of the infertile groups.
Discussion
The mean serum levels of T3 and T4 of the hyperprolactinemic infertile women were significantly lower than those of the controls (p<0.05). Similar findings were reported by Poppe and Velkeniers [16]. They observed that in hyperprolactinemic patients without any sign of pituitary dysfunction, there are normally reduced levels of thyroid hormones. Tasneem et al., [17] also observed in their study, that some of the women with high prolactin levels had subclinical hypothyroidism. Although the values of these hormones (T3, T4, and TSH) are within the normal range in this study, there is a wide variation in the range of blood levels of these hormones in the subjects used. These subjects (infertile women) may be in a compensated state with normal T4 levels achieved by increased TSH secretion.
The mean serum TSH concentration of the hyperprolactinemic infertile women was significantly higher (p<0.05) than those of the controls and normoprolactinemic infertile women. This is similar to observations made in a study by Sharma et al., [18] and Turankar et al., [19]. A significant positive correlation between TSH and prolactin levels in subjects enrolled in the study (r = 0.285, p<0.05) was observed. This finding is also consistent with the findings of Goswami et al., [13]. Thyroid hypofunction is characterized by low serum levels of T4, because of this low level there is an increase in secretion of thyrotropin releasing hormone (TRH). In some individuals, TRH increases the levels of both prolactin and TSH by stimulating the thyrotrophs and lactotrophs [20]. The relatively higher occurrence of deranged TSH values in the hyperprolactinaemic infertile women when compared to the normoprolactinemic infertile women and control group in this study reflects the tendency of hyperprolactinaemic infertile women towards thyroid insufficiency or the vice versa.
In this study, TSH levels were found to have correlated negatively and significantly with both T3 and T4 levels in all the study groups. This significant inverse relationship is not surprising since it is in good agreement with the concept that T4 plays the dominant role in the regulation of TSH secretion because T4 is rapidly converted to T3 within the pituitary cells. This negative feedback on the hypothalamopituitary axis results in increased secretion of TRH which inturn stimulates thyrotrophs and lactotrophs thereby increasing the levels of both TSH and prolactin.
Studies have shown that for normal sexual function, thyroid secretion of T3, T4 needs to be approximately normal [21]. Evidence from experimental and clinical studies have suggested a close relationship between the hypothalamic – pituitary – ovarian axis (HPO) and the hypothalamic – pituitary – thyroid axis (HPT) [19]. This is because, the specific thyroid hormone receptors at the ovarian level may regulate the influence of estrogens as well as reproductive function the at higher levels of the HPT axis thereby integrating the reciprocal relationship between these two major endocrine axes [22].
In hypothyroidism, increased TRH production leads to hyperprolactinemia and altered GnRH pulsatile secretion. This leads to a delay in LH response and inadequate corpus luteum leading to abnormal follicular development and ovulation. Thyroid hormone receptors are expressed on human oocytes and granulosa cells. At the cellular level, thyroid hormones synergize with FSH mediated LH/HCG receptor to exert direct stimulatory effects on granulose cell function e.g. progesterone production [14]. Altering the peripheral metabolism of estrogen and decreasing SHBG production is another pathway by which hypothyroidism may impact on fertility. These pathways may result in an abnormal feedback at the pituitary level [14] and consequently infertility.
Comparison of physical and biochemical parameters of hyperprolactinaemic infertile, normoprolactinaemic infertile women and controls
| Parameter | Hyperprolactinemic infertile women | Normoprolactinemic infertile women | Controls | Range Low High | Calc. F | Crit F | p-value |
|---|
| Age (yrs) | 30.2±3.57 | 30.5±3.93 | 29.8±2.62 | 20.0 – 40.0 | 1.817 | 3.036 | p>0.05 |
| Prolactin (ng/ml) | 63.09±61.78 | 12.58±5.17 | 8.21±3.71 | 1.00 – 368.6 | 49.379 | 3.036 | p<0.05 |
| TSH(μlu/ml) | 2.5±3.15 | 1.3±0.63 | 1.4±0.73 | 0.3 – 29.8 | 8.285 | 3.036 | p<0.05 |
| T3(ng/dl) | 103.3±22.30 | 117.8±18.61* | 117.0±17.30* | 40.0 – 180.0 | 10.442 | 3.036 | p<0.05 |
| T4(μg/ml) | 6.0±1.35 | 6.7±1.07* | 7.3±1.61* | 2.9 – 12.8 | 17.526 | 3.036 | p<0.05 |
| n | 90 | 90 | 50 | | | | |
Mean ± SD, S - Significant NS – Not significant *= higher than that of hyperprolactinemic infertile women
Correlation plot of thyroid stimulating hormone against prolactin in the controls

Conclusion
It is therefore concluded that hyperprolactinemia with thyroid dysfunction may be a major contributory hormonal factor in infertility among infertile women and as such, estimation of prolactin, T3, T4 and TSH should be included in the workup for infertile women especially those with hyperprolactinaemia.
Mean ± SD, S - Significant NS – Not significant *= higher than that of hyperprolactinemic infertile women
[1]. MC Evers, The infertile coupleAm Fam Physician 2002 54(3):1001-10. [Google Scholar]
[2]. KL Wright, Defining infertility: what infertility means for clinicians and clientsNetwork 2003 23(2):4-6. [Google Scholar]
[3]. DT Audu, TA Ojua, C Edem, RI Aernyi, Infertility and gender difference in reaction among couples and family and community treatment: a study of patients attending N.K.S.T. hospital Mkar in Benue state, NigeriaESJ 2013 9(32):96-106. [Google Scholar]
[4]. NJ Wiersema, AJ Drukker, MT Dung, GH Nhu, NT Nhu, CB Lambalk, Consequences of infertility in developing countries: Results of a questionnaire and interview. Survey in the South of VietnamJ Transl Med 2006 4:54 [Google Scholar]
[5]. N Ameh, TS Kene, SO Onuh, JE Okohue, DU Umeorah, OB Anozie, Burden of domestic violence amongst infertile women attending infertility clinics in NigeriaNiger J Med 2007 16:375-77. [Google Scholar]
[6]. A Alhassan, AR Ziblim, S Muntaka, A survey on depression among infertile women in GhanaBMC Womens Health 2014 14:42 [Google Scholar]
[7]. PT Tabong, PB Adongo, Infertility and childlessness: a qualitative study of the experiences of infertile couples in Northern GhanaBMC Pregnancy Childbirth 2013 13:72 [Google Scholar]
[8]. World Bank. World bank database. [Internet]. 2011 [cited 2014 Aug 22] Available from http://data.worldbank.org/indicator [Google Scholar]
[9]. MA Fritz, L Speroff, Clinical Gynaecologic Endocrinology and infertility 2010 12th EditionNew YorkBlackwell [Google Scholar]
[10]. FE Okonofua, Female and male infertility in Nigeria: studies on epidemiology of infertility in Nigeria with special reference to the role of genital tract infections and sexual and reproductive risk factors. Sweden: Department of Public Health Sciences Division of International Health (IHCAR) Karolinska Institutet 2005 [Google Scholar]
[11]. LA Nilsson, C Roepstorff, B Kiens, H Billig, C Ling, Prolactin suppresses malonyl-CoA concentration in human adipose tissueHorm Metab Res 2009 41(10):747-51. [Google Scholar]
[12]. S Bernichtein, P Touraine, V Goffin, New concepts in prolactin biologyJ Endocrinol 2010 206:1-11. [Google Scholar]
[13]. B Goswami, S Patel, M Chatterjee, BC Koner, A Saxena, Correlation of prolactin and thyroid hormone concentration with menstrual patterns in infertile womenJ Reprod Infertil 2009 10(3):207-12. [Google Scholar]
[14]. K Poppe, B Velkeniers, D Glinoer, Review: Thyroid disease and female reproductionClin Endocrinol (Oxf) 2007 66(3):309-21. [Google Scholar]
[15]. RI Ejemot-Nwadiaro, Biostatistics and health research methods 2009 Calabar: Datapro Publishers [Google Scholar]
[16]. K Poppe, B Velkeniers, Thyroid and infertilityVerh K Academy Geneeskd Belg 2002 64(6):389-99. [Google Scholar]
[17]. A Tasneem, I Fatima, A Ali, N Mehmood, MK Amin, The incidence of hyperprolactinaemia and associated hypothyroidism: local experience from LahorePak J Nuclear Med 2011 1:49-55. [Google Scholar]
[18]. P Sharma, P Suvama, T Nitin, Female infertility and its correlation with serum prolactin and TSH concentration- an unmatched case control studyJ Pharm Biomed Sci 2013 30(30):902-07. [Google Scholar]
[19]. S Turankar, K Sonone, A Turankar, Hyperprolactinaemia and its Comparision with Hypothyroidism in Primary Infertile WomenJ Clin Diagn Res 2013 7(5):794-96. [Google Scholar]
[20]. MA Emokpae, HB Osadolor, A Omole-Ohonsi, Sub-clinical hypothyroidism in infertile Nigerian women with hyperprolactinaemiaNig J Physiol Sci 2011 26:35-38. [Google Scholar]
[21]. AG Doufas, G Mastorakos, The hypothalamic-pituitary-thyroid axis and the female reproductive systemAnn N Y Acad Sci 2000 900:65-76. [Google Scholar]
[22]. S Saha, The female reproductive system and the hypothalamic-pituitarythyroid axis[Internet]. 2012. [cited 2014 Aug 21]. Available from http://www.pharmaceuticalintelligence.com/2012/12/11/the-female-reproductive-systemand-the-hypothalamic-pituitary-thyroid-axis [Google Scholar]