Introduction: Renal dysfunction is common in chronic liver disease. The cause of this renal dysfunction is either multi-organ involvement in acute conditions or secondary to advanced liver disease.
Objectives: The study was undertaken to assess the renal function in chronic liver diseases and find out the association of alteration of renal function with gradation of liver disease. (assessed by child-pugh criteria) and to find out the association of alteration of renal function among the cases of chronic liver disease of different aetiology.
Materials and Methods: This cross-sectional, observational study was undertaken in Department of General Medicine, Calcutta National Medical College & Hospital, Kolkata during March 2012 to July 2013 with 50 admitted patients of chronic liver disease after considering the exclusion criteria. The patients were interviewed with a pre-designed and pre-tested schedule, examined clinically, followed by some laboratory investigations relevant to diagnose the aetiology of chronic liver disease, and to assess the severity of liver and renal dysfunction. Data was analysed by standard statistical method.
Results: Eighty six percent of the patients were male and the mean age of study population was 43.58 y, 68% patients suffered from alcoholic liver disease, followed by 14% patients had chronic Hepatitis-B, 10% patients developed acute kidney injury, 20% had hepato renal syndrome and 14% had IgA deposition. The distribution of serum urea and creatinine across the categories of Child Pugh classification tested by Mann-Whitney test and the distribution was statistically significant.
Conclusion: The present study has found significant association between severity of liver dysfunction and certain parameters of renal dysfunction.
Introduction
Chronic liver disease is common clinical problem in our country. Chronic liver disease involves a process of progressive destruction and regeneration of liver parenchyma leading to fibrosis and cirrhosis [1]. Acute kidney injury, chronic kidney disease and the evaluation of numerous exogenous and endogenous measures of kidney function continue to be the focus of much research different patient population [2]. The presence of renal impairment in both groups is a poor prognostic indicator. Hepato-renal syndrome is a unique form of renal failure associated with advanced liver disease or cirrhosis and is characterized by functional renal impairment without significant changes in renal histology [3].
Chronic liver disease and cirrhosis are frequently complicated with renal dysfunction and this combination leads to significant morbidity and mortality [4]. There is considerable evidence that renal failure in patient with cirrhosis primarily related to disturbances in circulatory function-mainly, a reduction in system vascular resistance due to primary arterial vasodilatation in the splanchnic circulation, triggered by portal hypertension [5]. Intrinsic renal diseases may occur in patient with hepatitis B or hepatitis C and alcoholic cirrhosis. Moreover, patients with cirrhosis may develop a specific acute renal failure called type-I hepatorenal syndrome. Independent of event that leads to acute renal failure, patient with cirrhosis may have diseases, such as diabetes mellitus or hypertension and atherosclerosis, which may cause chronic renal injury [6,7].
In clinical practice plasma creatinine level and endogenous creatinine clearance are commonly used as more convenient but less accurate method for glomerular filtration rate assessment [8].
Objectives
The study was undertaken to assess the renal function in chronic liver diseases and find out the association of alteration of renal function with gradation of liver disease (assessed by Child-Pugh criteria) and to find out the association of alteration of renal function among the different aetiologies of chronic liver disease.
Materials and Methods
The present study was done as a descriptive, observational study with a cross-sectional design. The study was undertaken in Department of General Medicine, Calcutta National Medical College & Hospital, Kolkata during March 2012 to July 2013. It included the patients admitted with chronic liver disease of different aetiologies.
Patients included in the study group were diagnosed of chronic liver disease and had a definite aetiology for the chronic liver disease such as: Viral (Hepatitis B, Hepatitis C), Alcoholic chronic liver disease, Non alcoholic steatohepatitis, and Autoimmune (Wilson’s disease, cryptogenic).
Unconscious patients, known patients of kidney disease and patients taking any nephrotoxic drugs and patients of chronic diseases such as tuberculosis, malignancy, diabetes mellitus were excluded from the study.
During the study period 61 patients were admitted with chronic liver disease but among them 11 were not included in the study as they had existing kidney disease or had a positive history of consuming nephrotoxic drug or had other chronic diseases like tuberculosis, malignancy or diabetes mellitus. Therefore, the number of study population was 50.
The study was conducted after obtaining necessary permission from institutional ethics committee. The schedule was designed after discussion with the experts of general medicine and community medicine and pre testing was done in the general medicine outdoor among 10 patients of chronic liver disease, who came for follow up. (These patients were not taken as study population).
Informed written consent in vernacular was obtained from each patient before inclusion in the study. The consent form was also approved by the institutional ethics committee.
Patients were interviewed about duration of the disease, presence of alcoholism, presence of yellowish discoloration of urine, vomiting of blood and passage of black stool. General survey was done to assess presence of anemia, jaundice, clubbing and oedema. The patients were also examined for presence of ascitis, hepato-splenomegaly, distented veins, everted umbilicus, spider naevi, palmar erythema, gynaecomastia, testicular atrophy, and bleeding manifestation to assess the severity of liver dysfunction.
Biochemical examination like blood for hemoglobin, total count, differential count, ESR, and fasting and post prandial sugar was done. Laboratory investigations like total bilirubin with conjugated and un-conjugated fraction, Alanine amino transferase, Aspartate amino transferase S, Alkaline Phosphatase, total protein, albumin ,globulin, prothrombin time, HbSAg, Anti nuclear antibody, Anti-Liver Kidney Microsomal antibodies 1, 2 & 3 were done. Ascitic fluid was examined to assess the aetiology and severity of chronic liver disease. For assessment of kidney function serum urea, creatinine, seum sodium and potassium were examined.
Radiographic examination like ultrasonography of upper abdomen and Kidney, Ureter, Bladder was done. Upper gastrointestinal endoscopy was done for detecting gastro-oesophagial varices, Routine and microscopic examination of urine, 24 h protein excretion and measurement of 24 h urine volume were also done.
Statistical Analysis
Data was collected and tabulated and analysis was done by using standard statistical software like SPSS version 20 with proportion and percentage and statistical test like Mann Whitney and Kruskal Wallis.
Results
In this study most of the patients were in their forties and the mean age was 43.58 years and majority of patients were male. The study revealed most common cause of chronic liver disease was alcohol followed by Hepatitis B and Hepatitis C. All the patients had ascites and anaemia.
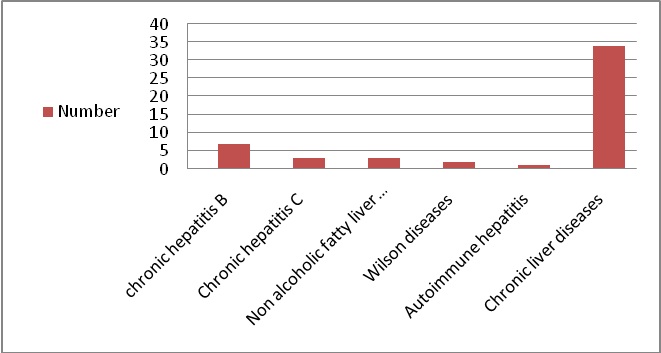
[Table/Fig-1] reveals, among study population, 34 (68%) patients suffered from Alcoholic liver disease,7 (14%) patients had chronic Hepatitis-B, 3 (6%) patients had chronic Hepatitis-C, 3 (6%) patients had Non alcoholic fatty liver disease, 2 (4%) patients had Wilson’s Disease and 1 (2%) patients had autoimmune hepatitis.
[Table/Fig-2]shows, 39 patients (78%) had Serum total protein 6 gm/dl. Forty seven patients (94%) had Serum albumin level <3gmdl. Forty one patients (82%) had serum urea within the range of 15-40 mg/dl. Nine patients (18%) had serum urea > 41 mg/dl. Forty patients (80%) on day 1 had serum creatinine level 1 mg/dl, and 40 patients (80%) had serum creatinine level on day 3 as1 mgdl.
[Table/Fig-3] shows, 66% patients had serum bilirubin level > 2mg/ 20 patients (40%) had Serum Aspartate amino transferase (AST) within the range of 42-100 u/L. Thirty five patients(70%) had Serum Alanine amino transferase (ALT) < 100 u/L 15 patients(30%) had Serum Alkaline phosphatase (ALP) < 100 u/L. Thirty three patients (66%) had Serum ALP within the range of 100-200 u/L. Two patients(4%) had Serum ALP > 200 u/L. Forty seven (94%) patients had dilated portal vein. Twenty three (46%) patients had grade-II esophageal varices, 24 (48%) had grade-III esophageal varices detected by Upper GI endoscopy.
It was found in the study that distribution of serum urea and creatinine, according to the severities of liver disease as per Child Pugh classification, was statistically significant, as tested by Mann-Whitney test [Table/Fig-4] but serum creatinine level on day 1 and day 3 was not found to be significantly distributed among different aetiologies of chronic liver disease as tested by Kruskal Wallis test [Table/Fig-5].
Discussion
The present study found maximum number of patients in the forties with the mean age 43.58 y. This finding was similar to Fleming KM et al., [9] who also found an increased incidence of chronic liver disease with increase in age. This study showed that the majority of patients were male which is similar to Fleming KM et al., [9]. The study also found that the incidence was over 50% higher in men compared with women. Alcohol, Hepatitis B, Hepatitis C and non alcoholic fatty liver disease (NAFLD) were among the causes of cirrhosis. Present study showed most common cause was alcohol followed by Hepatitis B and Hepatitis C.
Fasalato Silvano et al., [10] found ascites in 233 patients (75.4%). In this current study all patients had ascites. In the present study anaemia complicated most cases of cirrhosis; all patients had anaemia and most had moderate anaemia. In a study done by McHutchison JG et al., [11] it was found that bilirubin level was 3-10 mg/dl in cirrhosis unless other factors like hemolysis, acute viral hepatitis, were present In this study most patients had bilirubin in the range of 3-10 mg/dl.
Liver enzymes e.g. AST and ALT increase modestly in cirrhosis and usually in the range of 300 u/l [12]. In current study there was modest elevation in both enzymes. ALP level usually remains normal in cirrhosis [13]. In our study mean ALP level was 119u/l which is normal. Albumin level was reduced with altered albumin: globulin ratio which is a usual laboratory finding in chronic liver disease [13]. In one study, 30% patients with compensated cirrhosis and 70% patients of uncompensated cirrhosis had varices [14,15]. In this 11current study too majority of the patients (94%) had varices. In a study from Dhaka [16], no statistically significant relation between Child-Pugh score and serum creatinine was found but in our study, change of creatinine with Child-Pugh score was statistically significant (p<0.001). Fornari F et al., [17] showed 30% of patients with cirrhosis had gall stones, risk of developing stones most strongly associated with Child’s grade C & alcoholic cirrhosis with a yearly incidence of about 5%.In our study cholelithiasis in CLD was incidental USG finding. Majority (8%) occurred in ALD and 4% in HEP-C.
In the present study there was no statistically significant change in renal parameters in different aetiologies of liver disease but the result was different in other studies [18-20] like prevalence rate of AKI in cirrhosis was 68% in a study conducted by Fernandez-Seara J [18] but in our study only 10% patients had AKI. In the same study prevalence of hepatorenal syndrome was 25% [18]. Another study showed that among patients with ascites, HRS developed in about 20% and 40% of the patients, at 1 and 5 years, respectively [19]. Ruiz-del-Arbol L et al., [20] in a study done on 23 cirrhotic patients with spontaneous Bacterial peritonitis of which 8 patients developed type-I Hepatorenal syndrome.
Distribution of study population according to different aetiologies
Renal function profile in chronic liver disease
| Parameter | Frequency (%) |
|---|
| Serum Urea (mg / dl) |
| 15-40 | 41(82%) |
| >41 | 9(18%) |
| Creatinine (mg / dl)on day 1 |
| 1 | 40(80%) |
| 2 | 10(20%) |
| Creatinine (mg / dl) on day3 |
| 1 | 40(80%) |
| 2 | 4(8%) |
| 3 | 4(8%) |
| 4 | 2(4%) |
| Serum albumin(gm/dl) |
| <3 | 47(94%) |
| 3-3.5 | 2(4%) |
| >3.5 | 1(2%) |
| Serum globulin(gm/dl) |
| <2.5 | 1(2%) |
| >2.5-4 | 41(82%) |
| >4 | 8(16) |
| Renal biopsy |
| Mesangial proliferation,Ig A deposition | 7(14%) |
| Normal | 43(86%) |
Liver function profile in chronic liver disease
| Liver function profile | Number(%) |
|---|
| Total bilirubin |
| <2 | 17(34%) |
| 2-3 | 25(50%) |
| >3 | 8(16%) |
| Serum ALT(U/L) |
| 42-100 | 20(40%) |
| 101-200 | 27(54%) |
| >200 | 3(6%) |
| Serum AST(U/L) |
| <100 | 35(70%) |
| 100-200 | 12(24%) |
| >200 | 3(6%) |
| Serum ALP(U/L) |
| <100 | 15(30%) |
| 100-200 | 33(66%) |
| >200 | 2(4%) |
| Portal vein diameter |
| 12 | 3(6%) |
| 13 | 15(30%) |
| 14 | 28(56%) |
| 15 | 4(8%) |
| Upper GI endoscopy-esophageal varices |
| Abs | 3(6%) |
| G-II | 23(46%) |
| G-III | 24(48%) |
Distribution of study population according to alternation of renal function with gradation of liver disease (n=50)
| Renal complication | Child pugh classification of liver diseases | Statistical test on distribution of categories according to child Pugh classification |
|---|
| B | C |
|---|
| Serum Urea | 32 | 9 | Man whitney test,p=0.003 |
| Normal |
| Abnormal | 0 | 9 |
| Serum creatinine | 32 | 9 | Man whitney test,p=<0.0001 |
| Normal |
| Abnormal | 0 | 9 |
Association in relation to alternation of renal function with aetiologies of liver disease
| Renal function test in chronic liver diseases | Statistical test on distribution of aetiologies Independent sample Kruskal Wallis test |
|---|
| Serum Creatinine on Day 1 | p=0.762 |
| Serum creatinine on Day 3 | p=0.789 |
Conclusion and Limitation of the Study
The present study has found significant association between severity of liver dysfunction and some parameters of renal dysfunction. However no such significant association was found between distribution of different renal parameters among different aetiologies of chronic liver disease.
This study emphasizes the fact that we should be more vigilant when treating CLD patients, regarding their renal function, as proper screening, prevention and treatment of renal dysfunction can decrease morbidity and mortality
The study was done with limited patients admitted in a hospital so for generalization derivation from of the results, a further study with larger sample and in different settings would be required.
[1]. http://www.ner.vse.cz//wiki/index.php/Chronic liver disease last accessed on 13.5.2012 [Google Scholar]
[2]. Andy Slack, Andrew Yeoman, Julia Wendon, Renal Dysfunction in Chronic liver diseaseCritical Care 2010 14:214 [Google Scholar]
[3]. AP Betrosiun, B Agarwal, EE Douzinas, Acute renal dysfunction in liver diseaseWorld J Gastroenterol 2007 13(42):5552-59. [Google Scholar]
[4]. Zehra Eren, Gulein Kantaru, Assessment of renal functions in patients with liver disease: which one is correct?BANTAO Journal 2010 8(1):9-12. [Google Scholar]
[5]. Perez Gines, Robert Schrier W, Renal failure in cirrhosisN Engi J Med 2009 361:1279-90. [Google Scholar]
[6]. S Caronia, K Taylor, L Pagliaro, Further evidence for an association between non-insulin-dependent-diabetes mellitus and chronic hepatitis C virus infectionHepatology 1990 30:1059-63. [Google Scholar]
[7]. E Kalaitzakis, S Rosengren, T Skommevik , Björnsson ecoronary artery disease in patients with liver cirrhosisDig Dis Sci 2010 55(2):467-75. [Google Scholar]
[8]. Chantler C, Haycock GB, Estimation of glomerular filtration rate from height/plasma creatinine ratio Arch Dis Child 1983 58(9):754-55. [Google Scholar]
[9]. KM Fleming, GP Aithal, M Solaymani-Dodaran , TR Card, J West, Incidence and prevalence of cirrhosis in the United Kingdom, 1992-2001: a general population-based studyJ Hepatol 2008 49(5):732-38. [Google Scholar]
[10]. S Fasolato, P Angeli, L Dallagnese, G Maresio, E Zola, E Mazza, Renal failure and bacterial infections in patients with cirrhosis: epidemiology and clinical featuresHepatology 2007 45:223-29. [Google Scholar]
[11]. JG Mc Hutchison, MP Manns, DL Longo, Definition and management of anemia in patients infected with hepatitis C virusLiver Int 2006 26:389-98. [Google Scholar]
[12]. Johnston David E, Special Considerations in Interpreting Liver Function TestsAm Fam Physician 1999 59(8):2223-30. [Google Scholar]
[13]. Dienstag Jules L, (1955) Chronic Hepatitis. In: Fauci, Braunwald, Kasper, Hauser, Longo, Jameson, Loscalzo, (Eds)Harrison's Principles of Internal Medicine 2008 17th EditionNew York, NYMcGraw Hill [Google Scholar]
[14]. G Garcia-Tsao, AJ Sanyal, ND Grace, WD Carey, The Practice Guidelines Committee of the American Association for the Study of Liver Diseases, the Practice Parameters Committee of the American College of Gastroenterology Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosisAm J Gastroenterol 2007 102(9):2086-102. [Google Scholar]
[15]. P Dite, KL Goh, F Guarmer, D Liberman, R Eliakim, M Fried, for the World Gastroenterology Organisation (WGO). World Gastroenterology Organisation practice guideline: esophageal varices. Munich, Germany: World Gastroenterology Organisation 2008 [Google Scholar]
[16]. A Al-Mamun, G Mashud, F Karim, M Al-Mahtab, AJ Tarafdar, MF Hossain, serum creatinine levels unrelated to Child-Pugh status in uncomplicated cirrhosis of liver with ascitesEuroasian J Hepato-Gastroenterol 2013 3(1):36-38. [Google Scholar]
[17]. F Fornari, S Imberti, MM Squillante, L Squassante, G Civardi, E Buscarini, Incidence of gall stones in a population of patients with cirrhosisJ Hepatol 1994 20:797-09. [Google Scholar]
[18]. J Fernandez-Seara, J Prieto, J Quiroga, JM Zozaya, MA Cobos, JL Rodriguez- Eire, Systemic and regional hemodynamics in patients with liver cirrhosis and ascites with and without functional renal failureGastroenterology 1989 97(5):1304-12. [Google Scholar]
[19]. L Ruiz-del-Arbol, A Monescillo, C Arocena, P Vater, P Gines, V Moreira, Circulatory function and hepatorenal syndrome in cirrhosisHepatology 2005 42(2):439-47. [Google Scholar]
[20]. L Ruiz-del-Arbol, J Urman, J Fernanda, M Gonzalez, M Navasa, A Monescillo, Systemic, renal, and hepatic hemodynamic derangement in cirfhotic patients with spontaneous bacterial peritonitisHepatology 2003 38(1):1210-121. [Google Scholar]