Idiopathic Leukoplakia- Report of a Rare Case and Review
Shesha Prasad R1, Ramakrishna T2, Anuradha Pai3, Sujatha D4
1 Lecturer, Department of Oral Medicine & Radiology, The Oxford Dental College, Bommanahalli, Hosur Road, Bangalore, Karnataka, India.
2 Professor, department of Oral & Maxillofacial Surgery, The Oxford Dental College, Hospital, Bommanahalli, Hosur Road, Bangalore, Karnataka, India.
3 Professor & Head, Department of Oral Medicine & Radiology, The Oxford Dental College, Hospital & Research Centre, Bommanahalli, Hosur Road, Bangalore, Karnataka, India.
4 Professor, Department of Oral Medicine & Radiology, The Oxford Dental College, Hospital & Research Centre, Bommanahalli, Hosur Road, Bangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shesha Prasad R, The Oxford Dental College Bommanahalli, Hosur Road Bengaluru-560061, Karnataka, India.
E-mail: drsheshaprasad@gmail.com
Idiopathic leukoplakia is a rare potentially malignant lesion, usually found on the tongue with an increased risk of malignant transformation as compared to the tobacco associated form. The risk of malignant transformation increases with age. Diagnosis poses a challenge to the clinician as it is diagnosed by exclusion of other possible causes leading to hyperkeratosis. We present one such rare case in an elderly male patient who was followed up for a year to record the course of the lesion and to report recurrences, if any.
Idiopathic leukoplakia, Keratosis, Potentially malignant, Tongue lesion, White lesion
Case Report
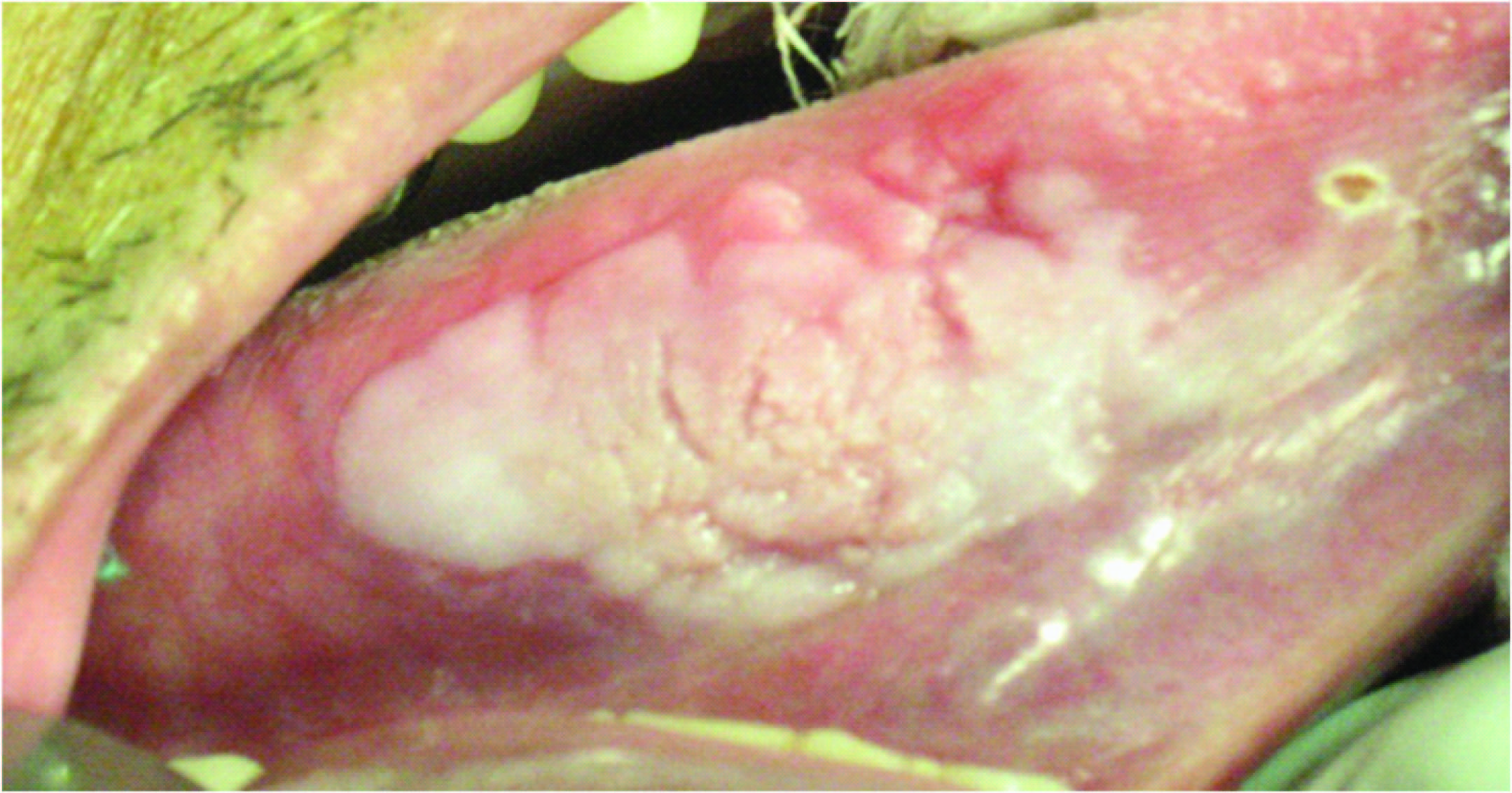
A 78-year-old male patient reported to the outpatient department, with a complaint of white patch on the right lateral border of the tongue for one month. The physical examination was unremarkable. Oral examination revealed a homogenous greyish white plaque on the right ventrolateral border measuring 4 cm x 2.5 cm [Table/Fig-1&2]. The surface showed cracked mud appearance and on palpation the lesion felt as raised and rough. The lesion was non tender and non scrapable. Lips, buccal mucosa, pharynx, and extra oral soft tissues appeared normal. Lymphadenopathy was absent. The patient was neither under any medication nor had any tobacco associated habits. Dental examination revealed crowns i.r.t #11,#12#13,#14,#15,#16,#44,#45,#46,#47,#34, and #35. No sharp margins were evident on palpation of these crowns. A provisional diagnosis of (idiopathic) leukoplakia was considered.
Lateral aspect of the lesion

Ventrolateral aspect of the lesion
Investigations
Routine blood investigations were reported as normal. Toluidine blue stain testing came negative. Incisional biopsy was planned and it included normal and affected mucosa from the site.
Differential diagnosis
Considering the patient’s age, traumatic or frictional keratosis was included. Teeth wear in the elderly can cause frictional keratosis in the lateral aspect of the tongue. This patient had crowns in the right posterior quadrant with no sharp margins or edges ruling out the diagnosis of traumatic or frictional keratosis. Oral hyperplastic candidiasis was the next differential diagnosis that was considered, which is also commonly seen in the elderly vowing to the various medications they consume and diabetes mellitus that commonly causes xerostomia. This patient was neither diabetic nor was under any medication. The mucosa appeared normal and was well hydrated ruling out candidiasis.
Chemical injury leading to a white plaque appearance was also considered. Usually a history of a drug or medication that is applied locally in the area of the lesion is strongly positive. The current case did not reveal any such history.
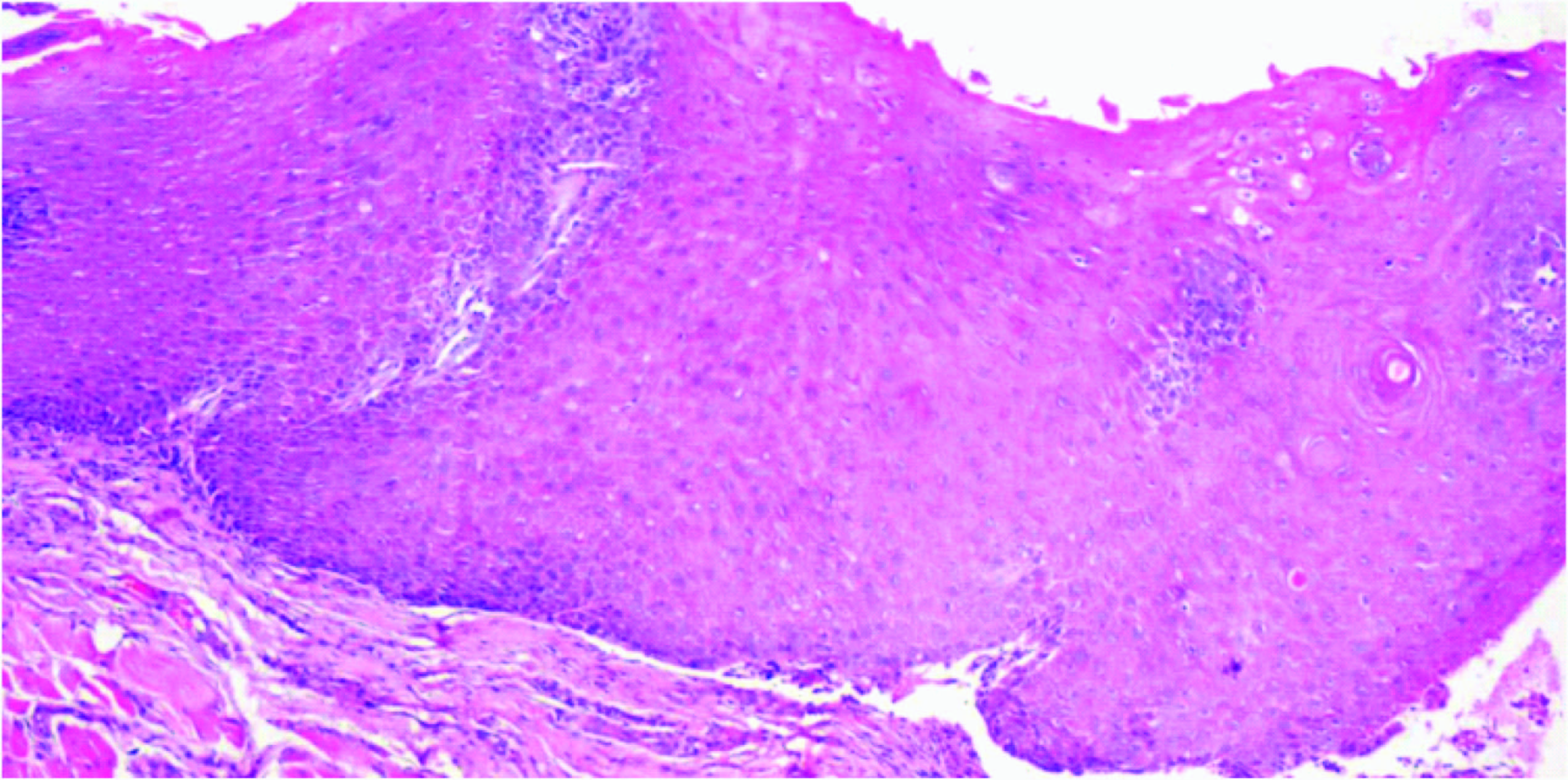
Incisional biopsy revealed histological features that were consistent with hyperplastic stratified squamous epithelium with intraepithelial inflammatory cell infiltration consistent with leukoplakia [Table/Fig-3]. Diagnosis of idiopathic leukoplakia was derived based on the history and clinical examination.
10X view: Hyperplastic epithelium showing keratin pearl formation and individual cell keratinisation
Treatment
Complete excision of the lesion was performed and the histological report was again consistent with leukoplakia.
Follow-up
The patient was followed up once in four months to check recurrence. The patient did not reveal any signs of recurrence even after one year following excision [Table/Fig-4].
No recurrence after one year follow up

Discussion
Idiopathic leukoplakia (IL) being rare, must be differentiated from tobacco associated leukoplakia [1]. Van der Waal et al., in a study reported idiopathic leukoplakia to have an incidence of 36% [2]. Clinical manifestations more commonly appear on the tongue [3] but can develop on the gingiva [4]. Sapna et al., reported idiopathic leukoplakia on the gingiva in a 40-year-old male prevalent for four months [4]. These lesions are commonly observed in female patients, invariably with epithelial dysplasia [2]. They can recur and have tendency towards malignant transformation. Vechio et al., [5] reported a case where idiopathic leukoplakia was persistent for 1.2 y on the dorsal surface of tongue in a 76-year-old female, which transformed into verrucus proliferative leukoplakia and ultimately squamous cell carcinoma. Oral leukoplakia in general is a potentially malignant disorder with an overall malignant transformation of 1% worldwide. 0.3% malignant transformation is seen in the Indian population [6]. IL shows greater tendency for malignant transformation and studies have shown that the malignant transformation ranges from 0.13% to 36.4% [7]. Vaander Waal and Arduino have reported that the lesions on the lateral border of the tongue in elderly, especially Indian men are considered at a greater risk for carcinogenesis [6,7]. Arduino also reported that the lesions on the ventrolateral surface of the tongue have shown greater risk of aneuploidy and loss of heterozygosity [7] which are the earliest changes towards malignant transformation.
The present lesion in this patient was considered as idiopathic as patient did not have any tobacco associated habits. Other causes like friction, trauma from sharp teeth, chemical injury, candidiasis were ruled out. The case discussed by Vechio et al., [5], showed signs of metamorphosis to verrucus form whereas the present case showed no such signs of metamorphosis. As described in numerous studies by Vaander Waal and Arduino, the present case had all the risk factors which warranted complete excision of the lesion. The duration of the lesion was approximately seven weeks before excision and had showed no signs of regression. The incisional biopsy revealed histopathological findings of hyperplastic parakeratotic epithelium with no signs of dysplasia. However, mild signs of dysplasia were noted in the second specimen following complete excision. This case was followed up for one year and no recurrence has been noted till date.
Points to be noted
IL is considered as a pre-malignant or a potentially malignant lesion more aggressive than oral leukoplakias. As it is less prevalent, its diagnosis poses a major challenge for practitioners. The diagnosis of IL is mainly based on exclusion.
Accurate diagnosis can be established only by detailed contributing history such as tobacco related habits, systemic diseases, medications and conclusively by histological studies correlating with history.
Conclusion
Cases of ILs are scantily reported in literature. Further research elaborating the cause of IL, its genetic predisposition, reason for tongue as the common site involved, rationale behind increased malignant transformation when compared with tobacco associated form, and as to why the elderly population are affected more though there is no continuous exposure to any tobacco associated habit needs to be addressed. Extensive reporting and analysis is required for possible answers.
[1]. van der Waal Isaäc, Axell T, Oral leukoplakia: a proposal for uniform reportingOral Oncol 2002 (38):521-26. [Google Scholar]
[2]. Freitas MD, Carrión AB, Vila PG, López JA, García AG, Rey JMG, Clinicopathologic aspects of oral leukoplakia in smokers and non-smokersOral Surg Oral Med Oral Pathol Oral Radiol Endod 2006 102:199-203. [Google Scholar]
[3]. Faecher RS, Thomas JE, Idiopathic leukoplakia lingualisGen Dent 1993 41(6):547-49. [Google Scholar]
[4]. Sapna L, Vandana KL, Idiopathic linear leukoplakia of gingiva: A rare case reportJournal of Indian Society of Periodontology 2010 14:198-200. [Google Scholar]
[5]. Vechio AD, Nakagima E, Azevedo LH, Alves FA, Migliari DA, Rapid progression of a idiopathic leukoplakia to aproliferative verrucous leukoplakia lesion and then squamous cell carcinomaQuintessence Int 2012 43:583-85. [Google Scholar]
[6]. van der Waal Isaäc, Potentially malignant disorders of the oral and oropharyngeal mucosa; terminology, classification and present concepts of managementOral Oncol 2009 (45):317-23. [Google Scholar]
[7]. Arduino PG, Bagan J, El-Naggar AK, Carrozzo M, Urban Legends Series: Oral LeukoplakiaOral Dis 2013 19(7):642-59. [Google Scholar]