Giant Serpentine Vertebrobasilar Aneurysm with Vertebral Artery Hypoplasia and Fenestration- A Case Report
Pradeep Choudhary1, Harsh Vardhan Khokhar2, Sangeeta Saxena3
1 Senior Resident, Department of Radiodiagnosis, Government Medical College Kota, Rajasthan, India.
2 Assistant Professor, Department of Radiodiagnosis, Government Medical CollegeKota, Rajasthan, India.
3 Associate Professor, Department of Radiodiagnosis, Government Medical CollegeKota, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pradeep Choudhary, Senior Resident, Mirdha Nagar, Didwana Road, Kuchaman City, Nagaur, Rajasthan-341508, India.
E-mail: pradeep.choudhary04@gmail.com
Intracranial aneurysm in paediatric age group is rare and association of the aneurysm with congenital vertebral artery anomaly is further rarer. We describe such a case in an 11-year-old male patient who consulted a paediatrician about headache and vertigo, and a noncontrast CT (NCCT) head revealed peripherally calcified hyperdense mass in prepontine and basal cisterns. Magnetic resonance imaging (MRI) including contrast enhanced magnetic resonance angiography (MRA) revealed partially thrombosed giant serpentine aneurysm of right vertebrobasilar artery and contralateral hypoplastic vertebral artery with fenestration. The nondominant left vertebral artery gave off the posterior inferior cerebellar artery, then became hypoplastic and joined with its counterpart to form the basilar artery. This pattern is called as type 9. The patient was kept on conservative management. The role of MRI in this congenital anomaly and its association with vertigo and aneurysm of vertebro-basilar artery is discussed.
Angiography, Basilar artery, Paediatric intracranial aneurysm
Case Report
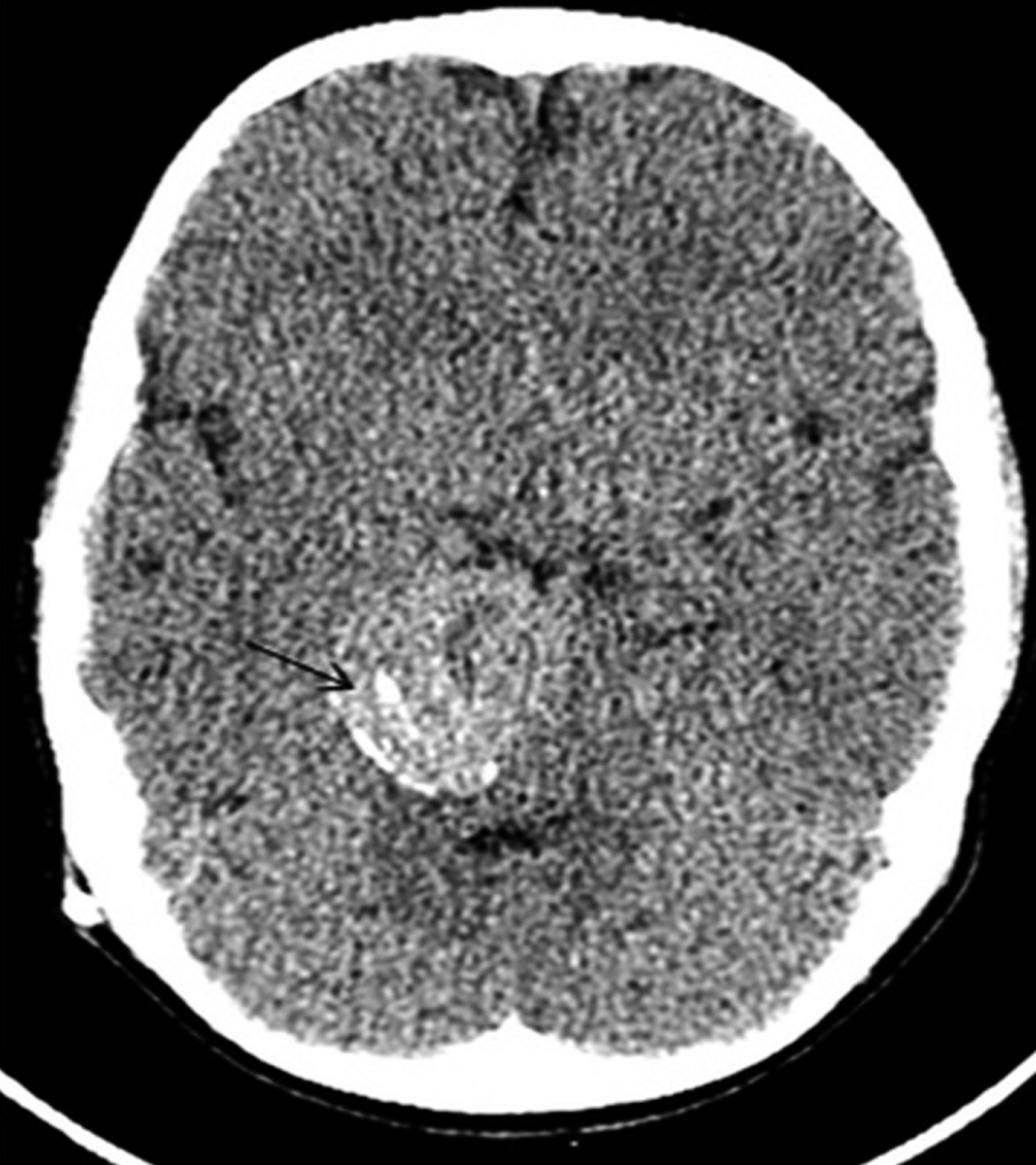
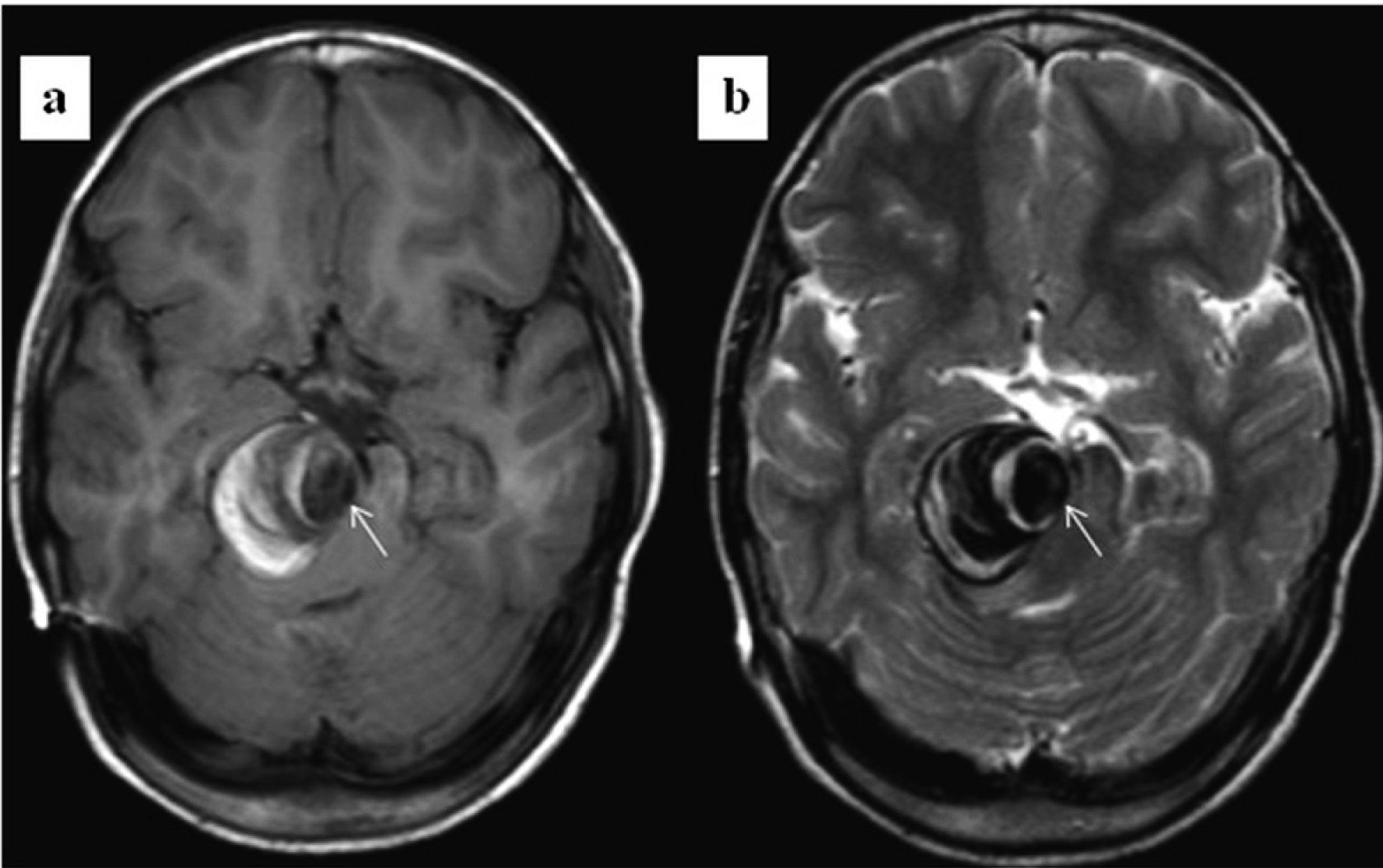
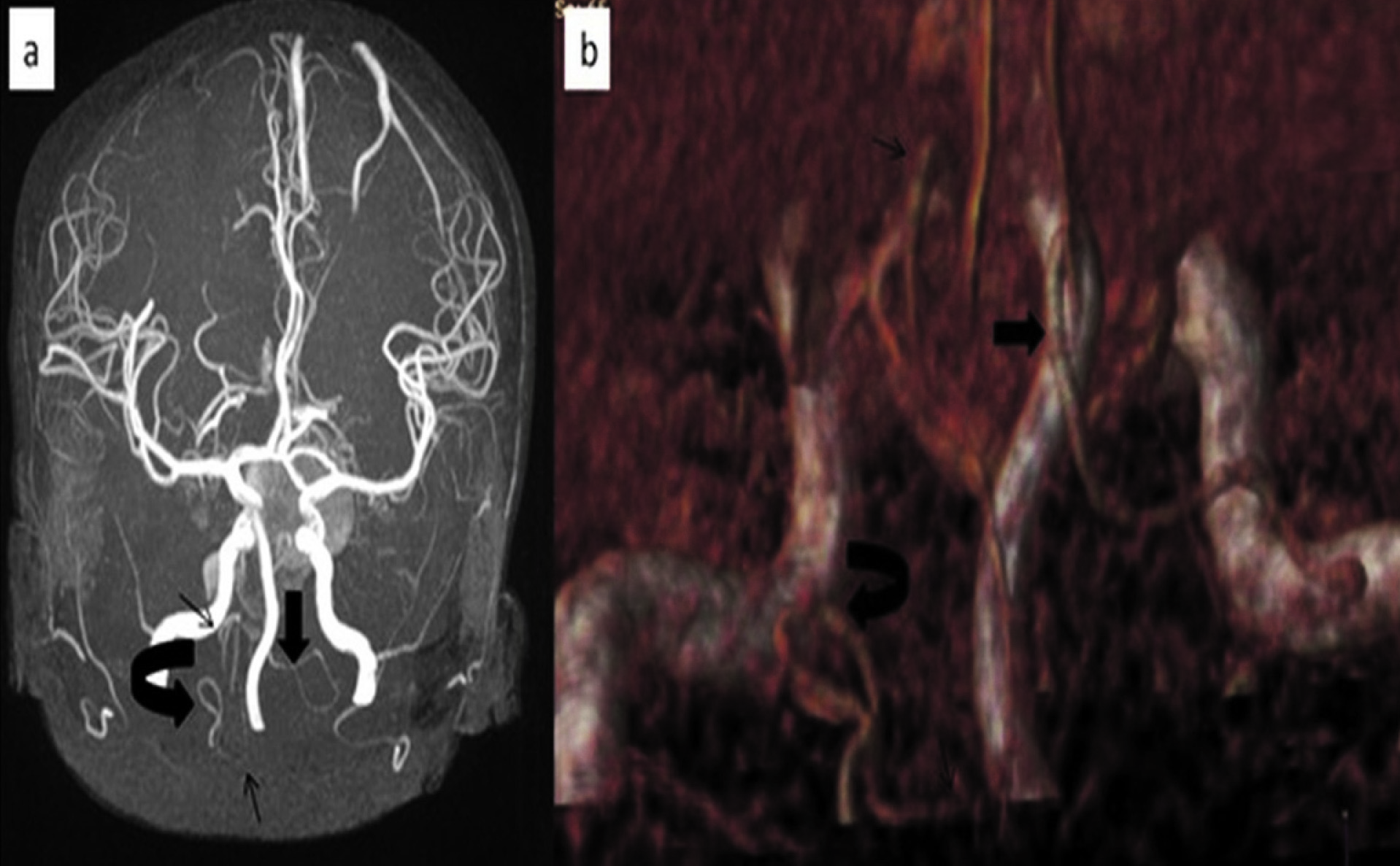
An 11-year-old child presented to the paediatrician in Government Medical College Kota, Rajasthan, India, with complaints of intermittent headache, vertigo and vomiting for last one month. Parents gave the past history of hydrocephalus due to tuberculous meningitis years back, for which ventriculoperitoneal shunt was put, however no documentation was available. Patient had taken complete antitubercular treatment according to the parents. No sensory or motor deficits were noted on examination. Non-contrast CT (NCCT) head revealed large peripherally calcified hyperdense mass anterior to the brainstem with mass effect on the brainstem [Table/Fig-1]. Magnetic resonance imaging on 1.5-T scanner (T1 weighted, T2 weighted, fluid attenuated inversion recovery (FLAIR), diffusion weighted(DWI), apparent diffusion coefficient, gradient echo) revealed a 3.3 cm (Antero-posterior) x 2.6 cm (Transverse) x 3.1 cm (Cranio-caudal) fusiform, tortuous, well-defined, heterogenous mass arising from dominant right vertebro-basilar artery just after origin of right posterior inferior cerebellar artery (PICA) with mass effect on brain stem. The lesion also caused antero-superior displacement of basilar artery and elevation of anterior inferior cerebellar arteries. Multiple areas of blooming corresponding to calcifications in NCCT, were also seen. The lesion showed eccentric area of signal void in spin echo pulse sequences [Table/Fig-2] which became hyperintense on post contrast imaging. The entry and exit points of parent vessel in the aneurysm were separate. These findings were consistent with partially thrombosed giant serpentine vertebrobasilar aneurysm. Contrast enhanced MRA also showed hypoplastic left vertebral artery (diameter 2.8 mm) with fenestration and continuation of the artery as left PICA. A very thin calibre (1mm) vessel was connecting the hypoplastic vertebral artery with contralateral vertebral artery to form basilar artery at higher level. Left PICA arose at the level of the foramen magnum and remained lateral and posterior to the brainstem with caudal loop located well below the lower pole of the tonsil. Right PICA arose at higher level than its counterpart and had oblique course [Table/Fig-3].
NCCT head axial view shows peripherally calcified hyperdense mass in basal cistern region with mass effect on brainstem
MRI brain shows well-circumscribed mass distorting the brainstem and containing mixed signal intensities on both T1W (a) and T2W (b) Images representing various stages of clot in the thrombosed portion of the lumen and evidence of eccentric signal void within the patent portion of the residual lumen (arrows)
MIP image (a) and volume rendered image (b) of post gadolinium scan shows fenestration (curved arrow) and hypoplastic left vertebral artery continuing as left PICA (thin straight arrows). Right vertebral artery is of normal calibre and situated in midline with higher origin and altered (oblique) course of right PICA (thick straight arrows)
Based on imaging finding of unruptured, partially thrombosed and calcified giant serpentine posterior fossa aneurysm, patient was kept on conservative management. However, patient lost on follow up so outcome was not decided.
Discussion
Intracranial aneurysms are rarely seen in the paediatric population with a reported prevalence of 0.5% to 4.6% [1]. Compared to adult intracranial aneurysm they tend to be larger and occur with greater frequency in the posterior fossa with a male preponderance [1].
In paediatric intracranial vascular pathologies catheter angiography is less favoured imaging technique and computed tomography remains the initial imaging method of choice in acute presentations [2]. MR imaging with MR angiography is particularly useful in non emergent setting and provides information equivalent to CT and MDCT angiography without drawback of radiation [2]. In both MRA and CTA, for measurements (e.g., largest aneurysm dimension, neck size) source images are most useful, whereas MIP (maximum intensity projection) or 3D renditions are best suited for assessment of direction of the aneurysm projection [3].
Prevalence of vascular anomalies such as a duplication or a fenestration are more common in the vertebrobasilar system (posterior circulation) compared to the carotid circulation (anterior circulation) [4]. Hypoplastic vertebral artery (lumen diameter smaller than 3 mm) is seen in 10–40% of normal angiograms mainly on right side and in about 1% of cases; vertebral artery terminates as the posterior inferior cerebellar artery (PICA) [5]. In our case hypoplastic left vertebral artery (VA) had fenestration and it was continuing as PICA. Embryologic basis for such a variation probably appears duplication of the distal VA of the LSA (Lateral spinal artery) type as proposed by Siclari at al., [6].
It is well-established that great differences in the diameter of the vertebral arteries at a level superior to the first cervical vertebra, has an important role in the etiology of the vertebrobasilar insufficiency and basilar deviation [7]. In the MR angiographic study by Paksoy et al., significant association was found between congenital morphologic anomaly of distal vertebral artery (CMADVA) and vertigo as seen in our case [8]. When we consider hypoplastic artery criteria of 1 mm than in our case left vertebral artery gave left PICA branch after fenestration then became hypoplastic (so partial hypoplasia) to join contralateral normal vertebral artery so constituting type 9 pattern according to Paksoy classification [9].
Aneurysms on the vertebrobasilar junction are rare, with an incidence of 0.5% of all treated aneurysms in a study, however it is one of the site of predilection for serpentine aneurysms [9,10]. Vertebrobasilar aneurysms are often associated with fenestration of the proximal basilar artery and vice versa [9]. To the best of our knowledge no case has been reported previously in literature, of giant serpentine vertebrobasilar junction aneurysm with contralateral vertebral artery hypoplasia and fenestration. Our case is first case of this type. By definition, a serpentine aneurysm is usually giant (2.5 cm) having separate entry and exit points of residual aneurysmal lumen which are separated by a variable distance. Lumen of the aneurysm is almost completely clotted except for a residual irregular eccentric lumen [10]. Progression of calcification within the aneurysm is often associated with a regression of mass effect and edema in adjacent brain tissue [10].
In our present case we postulate that presenting clinical features of the child were due to both, mass effect by the partially thrombosed aneurysm and congenital vascular variance. Furthermore altered hemodynamics due to hypoplastic and fenestrated vertebral artery may be the cause of aneurysm formation. Management of basilar or vertebrobasilar aneurysms is complicated and still evolving [10].
Conclusion
Although vertebrobasilar aneurysms are rare; they are often associated with fenestration, duplication, hypoplasia or combination of them in the posterior circulation. Such associated vascular variations has role in etiology of the aneurysm and help in proper presurgical planning so they worth reporting.
[1]. Huang J, McGirt MJ, Gailloud P, Tamargo RJ, Intracranial aneurysms in the paediatric population:case series and literature reviewSurgical Neurology 2005 63:424-33. [Google Scholar]
[2]. Gatscher S, Brew S, Banks T, Simcock C, Sullivan Y, Crockett J, Multislice spiral computed tomography for paediatric intracranial vascular pathophysiologiesJ Neurosurg 2007 107(3 Suppl Paediatrics):203-08. [Google Scholar]
[3]. Hacein-Bey L, Provenzale JM, Current Imaging Assessment and Treatment of Intracranial AneurysmsAJR 2011 196:32-44. [Google Scholar]
[4]. Kovaxč JD, Stanković A, Stanković D, Kovač B, Šaranović D, Intracranial arterial variations: A comprehensive evaluation using CT angiographyMed Sci Monit 2014 20:420-27. [Google Scholar]
[5]. Tay KY, U-King-Im JM, Trivedi RA, Higgins NJ, Cross JJ, Davies JR, Imaging the vertebral arteryEur Radiol 2005 15:1329-43. [Google Scholar]
[6]. Siclari F, Burger IM, Fasel JHD, Gailloud P, Developmental anatomy of the distal vertebralartery in relationship to variants of the posterior and lateral spinal arterial systemsAm J Neuroradiol 2007 28:1185-90. [Google Scholar]
[7]. Uzmansel D, Kurtoglu Z, Bagdatoglu C, Kara A, Altan Yildiz A, Unilateral variant vertebral artery with an aneurysm of the basilar tip: a case reportInternational Journal of Anatomical Variations 2009 2:96-98. [Google Scholar]
[8]. Paksoy Y, Vatansev H, Seker M, Ustun ME, Buyukmumcu M, Akpinar Z, Congenital morphological abnormalities of the distal vertebral arteries (CMADVA) and their relationship with vertigo and dizzinessMed Sci Monit 2004 10:CR316-23. [Google Scholar]
[9]. Peluso JPP, Rooij WJV, Sluzewski M, Beute GN, Aneurysms of the vertebrobasilar junction: incidence, clinical presentation, and outcome of endovascular treatmentAJNR Am J Neuroradiol 2007 28:1747-51. [Google Scholar]
[10]. Mawad ME, Klucznik RP, Giant serpentine aneurysms: radiographic features and endovascular treatmentAJNR Am J Neuroradiol 1995 16:1053-60. [Google Scholar]