Resection and Regeneration – A Novel Approach in Treating a Perio-endo Lesion
Vineetha Varughese1, Jaideep Mahendra2, Anchu Rachel Thomas3, N. Ambalavanan4
1 Post Graduate Student, Department of Periodontology, Meenakshi Ammal Dental College, Madurovoyal, Chennai, India.
2 Professor, Department of Periodontology, Meenakshi Ammal Dental College, Madurovoyal, Chennai, India.
3 Post Graduate Student, Department of Conservative Dentistry, Meenakshi Ammal Dental College, Madurovoyal, Chennai, India.
4 Professor and Head, Department of Periodontology, Meenakshi Ammal Dental College, Madurovoyal, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jaideep Mahendra, Department of Periodontology, Meenakshi Ammal Dental College, Alappakam Main Road, Madurovoyal, Chennai- 600095, India.
E-mail: jaideep_m_23@yahoo.co.in
The pulp and the periodontium are invariably anatomically and functionally related to each other. Lesions involving both the periodontium and the pulp complicate diagnosis, treatment planning and prognosis. An emerging approach to periodontal therapy is the concept of regeneration. In this case report, a novel combination therapy of a blend of platelet rich fibrin with bone graft and guided tissue regeneration membrane was used in the treatment of a perio-endo lesion of a multirooted tooth. A successful outcome in alleviating patient’s symptoms and regeneration was seen.
Bone graft, GTR, Perio endo continuum, PRF, Resection
Case Report
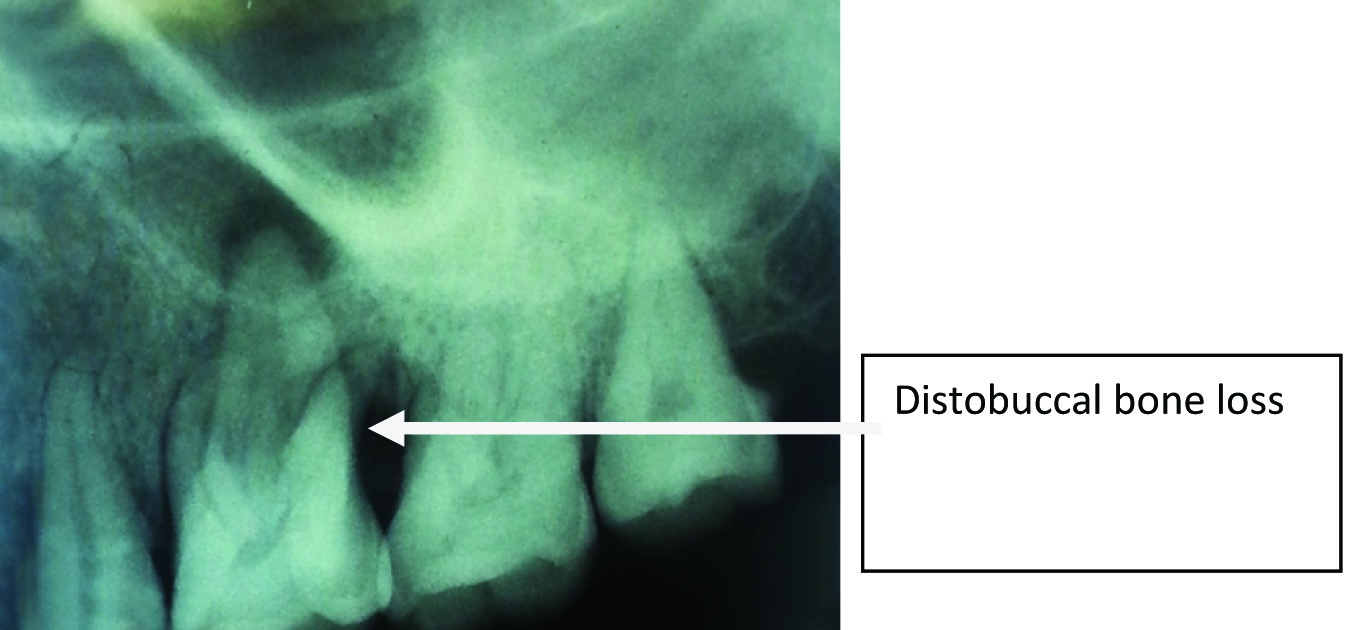
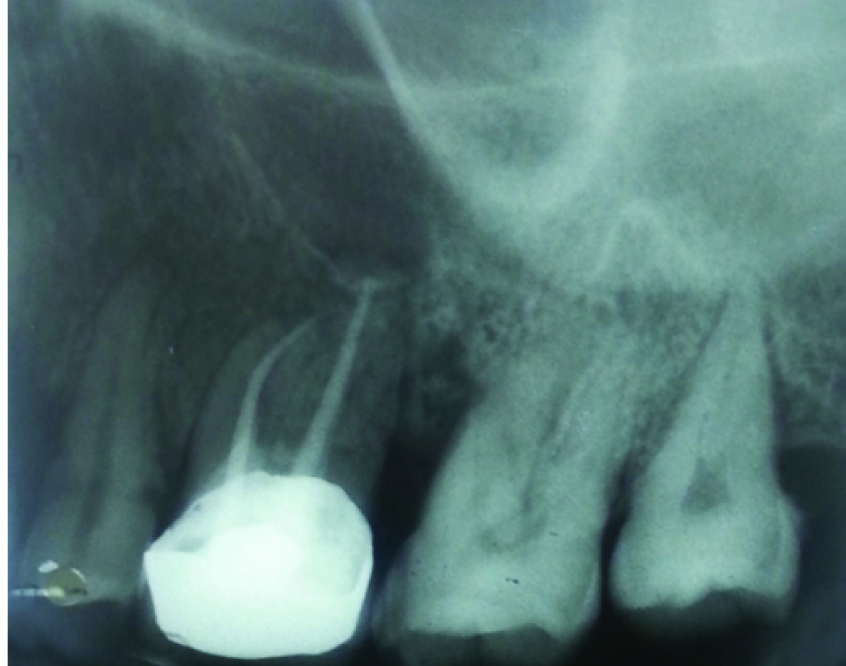
A 40-year-old male patient reported to the Outpatient Department of Periodontology, with a chief complaint of pain and mobility in his right upper back tooth region. On examination of the periodontium, a mild swelling was seen in relation to 16 and17 region. The swelling was diffuse, soft and edematous measuring around 2x2 mm. Probing pocket depth of 5 mm was seen on the mesial aspect of 16 and 9 mm distobuccally. Radiographically, 16 showed widening of periodontal ligament with pronounced radiolucent area surrounding the distobuccal root indicating bone loss [Table/Fig-1]. A radiolucency of 0.5x1mm was also seen at the apical region of the palatal root of 16. The tooth also demonstrated a grade I mobility and tenderness to percussion. Patient was systemically healthy and gave no history of medications or prior hospitalization. Routine blood investigations were done and all the parameters fell within the normal range. The patient was then referred to the Department of Endodontics where vitality testing was done in relation to 16. The vitality test revealed a partially vital pulp. Based on the thorough clinical and radiographic examination, a diagnosis of a primary periodontal lesion with a secondary endodontic involvement in relation to 16 was made.
Preoperative radiograph of 16 showing extensive bone loss distally and periapicallesion in relation to palatal root
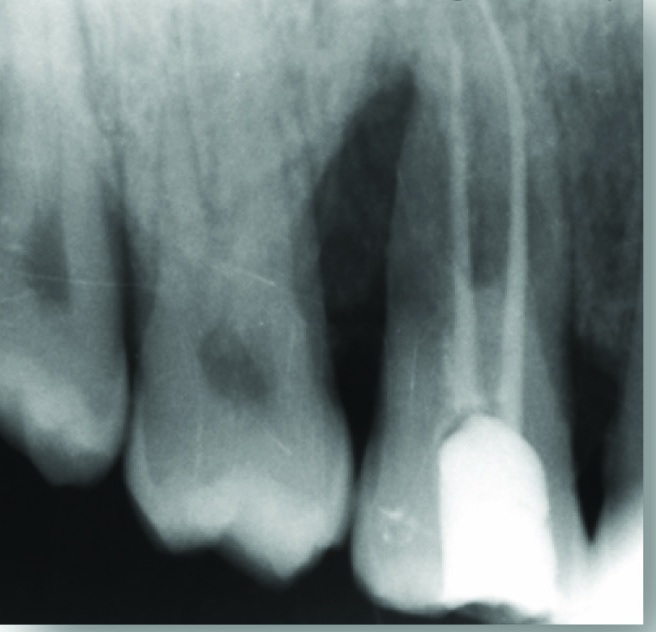
The formulated treatment plan involved Phase I therapy: scaling and root planing followed by systemic antibiotic regimen (Amoxicillin/500 mg/thrice daily/5 d). Root canal treatment (RCT) was planned for 16. It was completed in three sittings [Table/Fig-2]. The canals were cleaned and shaped using stainless steel files and Nickel Titanium rotary instruments and irrigation with 5.25% sodium hypochlorite. The canals were obturated with guttapercha and calcium hydroxide was used as an intracanal medicament. Resection of the affected distobucal root was planned due to the extensive bone loss surrounding the distal root and mobility of the tooth. Phase II of the treatment plan scheduled three months after RCT, involved root resection and periodontal regenerative surgery using a blend of platelet rich fibrin (PRF) and bone graft along with GTR membrane. The treatment was explained to the patient and an informed consent was obtained.
RVG after endodontic treatment in 16
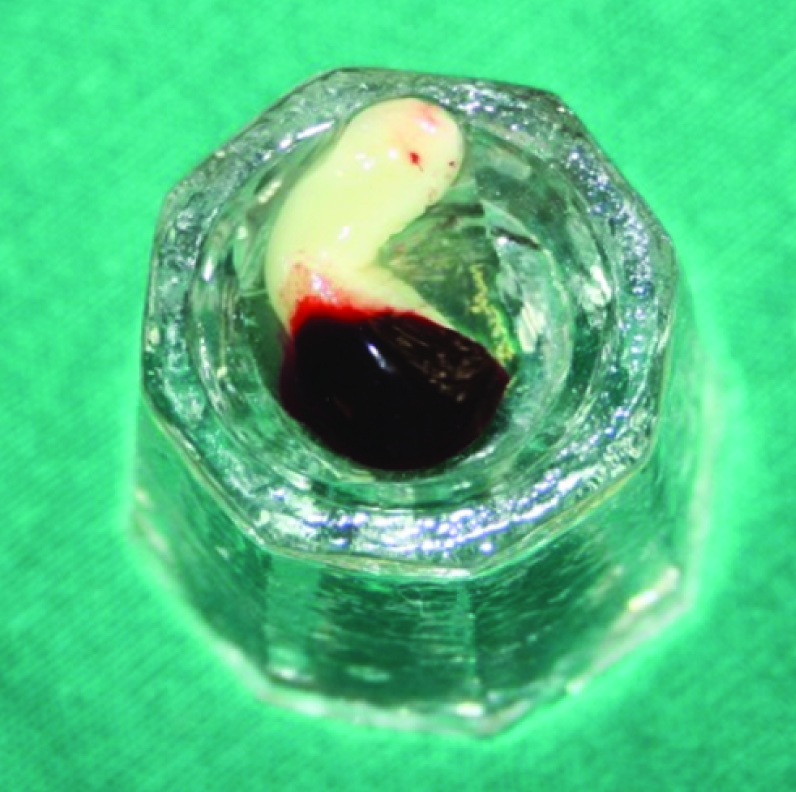
Prior to the surgery, PRF was prepared in accordance with the protocol developed by Freymiller and Aghaloo [1]. Intravenous blood from the antecubital vein was collected in a 10 ml sterile tube without anticoagulant and immediately centrifuged at 3000 rpm for 10 min. PRF was easily separated from red corpuscles base (preserving a small RBC layer) using sterile tweezers just after removal of PPP (platelet-poor plasma) and then transferred into a sterile dappen dish [Table/Fig-3].
PRF transferred to dappen dish
Procedure
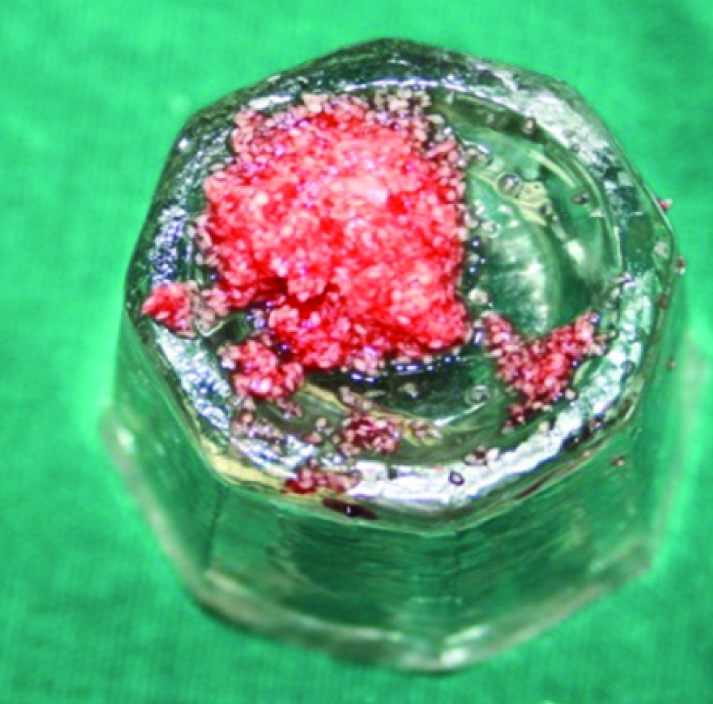
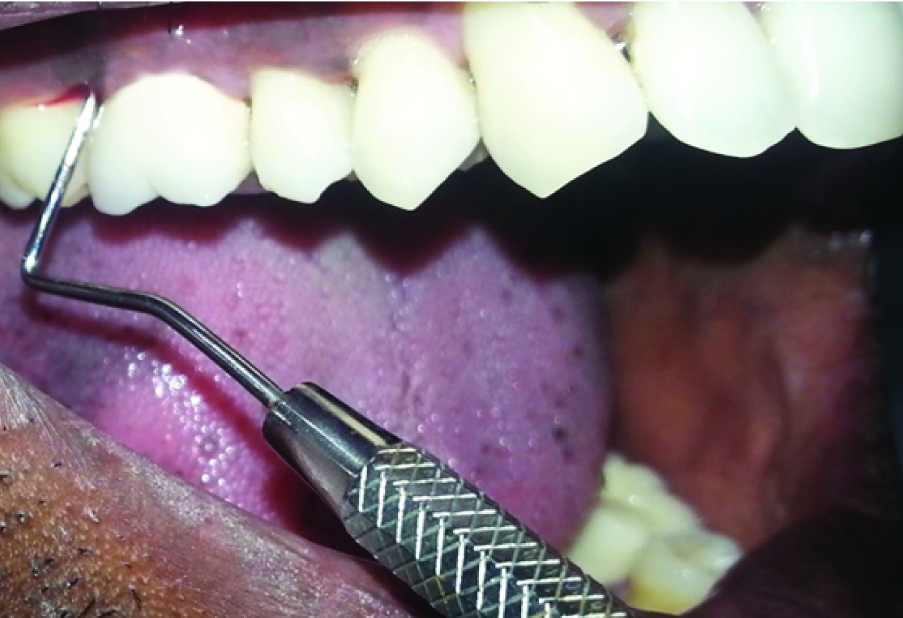
Standard sterilization protocol and proper asepsis was maintained. The area selected for surgery was anaesthetized with lignocaine with adrenaline (1: 80,000 concentration) [Table/Fig-4]. Sulcular incision was given in relation to 16 and 17. A single vertical releasing incision distal to 15 was given preserving the mesial papilla of 16 extending upto the mucogingival junction and a full thickness mucoperiosteal flap was elevated [Table/Fig-5]. The defect was thoroughly debrided using gracey’s curettes. Resection of distobuccal root was done obliquely at the furcation level using a tapered fissure bur [Table/Fig-6]. The resected root was removed with an artery forceps [Table/Fig-7] and a resection seal with type II glass ionomer cement was used. The remaining ledges and bony defects were removed using a file and bur [Table/Fig-8]. The PRF was mixed with bone graft (osseograft; Advanced Biotech Products Ltd, India) to attain a gel like consistency [Table/Fig-9]. This gel formation was then packed into the defect. A resorbable GTR membrane (Healiguide; Advanced Biotech Products Ltd, India) was trimmed and adapted to the defect area so that entire defect was completely covered [Table/Fig-10]. The flap was advanced coronally and sutured with 3-0 black silk using simple interrupted technique. A periodontal dressing was given to avoid any trauma to the surgical site. Amoxicillin (500 mg/thrice daily/5 d) for the patient was started two days prior to the procedure and was continued three days thereafter. Aceclofenac (100 mg/thrice daily/3 d) was prescribed to ward off infection and for pain management after surgery. Postoperative instructions were given.
Preoperative clinical photograph

Full thickness mucoperiosteal flap elevated

Resection of distobuccal root was done obliquely at the furcation level


16 after removal of distobuccal root and bone contouring

Blend of PRF and bone graft
Pre-suturing of flap, placement of blend and GTR membrane

Patient reported after 10 d for suture removal and healing was found to be satisfactory. Reviews were scheduled after one month, six months and 12 months. One month following surgery, the tooth was restored with a metal ceramic crown. Radiographs at six months [Table/Fig-11] and 12 months [Table/Fig-12] showed a significant bone fill at the treated site. Periodontal examination at six months and 12 months revealed a reduction in probing pocket depth and normal soft tissue contour. At 12 months, probing pocket depth was reduced to 4 mm with respect to the distal aspect of 16 and to 3 mm in relation to the mesial aspect [Table/Fig-13]. In terms of mobility, at 12 months, it was observed that there was no mobility in relation to 16. The patient was comfortable and satisfied with the outcome of the treatment, as his complain of pain and mobility was dealt with.
Postoperative radiograph at 6 months showing defect fill

Post operative radiograph at 12 months showing defect fill
Clinical post op at 12 months showing reduced probing pocket depth
Discussion
In this report, the patient had reported with a complaint of recurrent pain, a mild swelling and mobility in relation to 16. A diagnosis of a primary periodontal lesion with secondary endodontic involvement was made, as the tooth presented the classic signs of periodontitis (probing depth, bone loss) and was partially vital. Partial pulp necrosis, particularly in the cases of multi rooted teeth is common [2], hence the tooth showed a positive response during pulp testing. The pulp can maintain its vitality if the microvasculature at the apical foramen remains intact [3].
Primary periodontal disease with secondary endodontic involvement, require both endodontic and periodontal therapies.The prognosis in these cases depends upon the stage of periodontal disease and the efficacy of periodontal treatment. In molar teeth the prognosis may be better. Since not all the roots may suffer the same loss of supporting tissues, root resection can be considered as a treatment option. In the present case, the distobuccal root showed loss of supporting structures and hence resection of the root was planned.
Osseograft was chosen as the osteoconductive graft as it is a readily available bovine bone which is processed to yield natural bone mineral minus the organic component. Once the osseograft is placed in the osseous defect, a sequential differentiation of mesenchymal type cell occurs to form cartilage and bone [4].
On the other hand, the use of PRF in periodontal therapy is an upcoming trend showing optimistic and promising results. PRF, introduced by Dohan et al., [5], is a second-generation platelet concentrate enriched with platelets and growth factors which promote tissue regeneration and healing. PRF being an autologous material, the risk of disease transmission is less.
In this case report, we utilized a combination therapy of a blend of PRF and bone graft (osseograft) and a GTR membrane (Healiguide). In similar studies by Guillemin and Mellonig [6], a combination of barrier materials and bone graft was used and they concluded that combination therapy attained a greater attachment gain and bone fill. The use of PRF along with bone grafts accelerates the healing and regenerative processes [6,7].
After the placement of the blend of PRF and bone graft, the membrane was placed as a barrier between the gingival flap and the defect before flap repositioning and suturing. Similar surgical techniques using PRF, hydroxyapatite and PRF membrane were done by Shivashankar et al.,[8]. The goal of membrane barrier procedures is to guide proliferation of the different tissues during healing after therapy (selective cell repopulation). Overall, the blend of PRF and bone graft and GTR membrane showed tremendous progress and outcome in the management of perio-endo lesion with improvement in clinical parameters.
Clinical and radiographic examination at six and 12 months revealed bone fill indicating regeneration. Radiographic assesement of the tooth revealed an obturation, 1mm short of the apex. Michelle et al., (1979) evaluated 501 RC treated tooth and found that in vital teeth, when the roots were obturated greater than 1mm short of the apex, a higher success rate (96%) was seen [9]. No pathological findings or mobility were seen and patient was completely asymptomatic and pleased with the treatment outcome. The management of endoperio lesions without regenerative therapy showed a success rate of 27-37%, whereas the use of regenerative therapies showed a success rate to improve to 77.5% [10]. The use of a blend of PRF and bone graft to form a gel consistency gives enhanced graft stability, retention and lesser chances of displacement. This being an important pre requisite for successful regeneration lead to improved treatment outcome and bone fill in this case.
Conclusion
The following conclusion is drawn from this case report. The combination therapy of a blend of PRF and bone graft and GTR shows successful results with elimination of pain and mobility, improvement in periodontal parameters and patient satisfaction.
[1]. Freymiller EG, Aghaloo TL, Platelet-rich plasma: ready or not?J Oral MaxillofacSurg 2004 62(4):484-88. [Google Scholar]
[2]. Peters DD, Baumgartner JC, Lorton L, Adult pulpal diagnosis: evaluation of the positive and negative responses to cold and electrical pulp testsJ Endod 1994 20:506-11. [Google Scholar]
[3]. Langeland K, Rodrigues H, Dowden W, Periodontal disease, bacteria, and pulpal histopathologyOral Surg Oral Med Oral Pathol 1974 37:257-70. [Google Scholar]
[4]. Harakas NK, Demineralized bone matrix-induced osteogenesisClin Orthop Rel Res 1984 188:239-51. [Google Scholar]
[5]. Dohan DM, Choukroun J, Diss A, Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolutionOral Surg Oral Med Oral Pathol Oral RadiolEndod 2006 101(3):E37-44. [Google Scholar]
[6]. Guillemin M, Mellonig J, Healing in periodontal defects treated with decalcified freeze dried bone allograft in combination with e-PTFE membranesJ ClinPeriodontol 1993 20:528-36. [Google Scholar]
[7]. Sakka S, Coulthard P, Bone quality: a reality for the process of osseointegrationImplant Dent 2009 18:480-85. [Google Scholar]
[8]. Shivashankar VY, Johns DA, Vidyanath S, Sam G, Combination of platelet rich fibrin, hydroxyapatite and PRF membrane in the management of large inflammatory periapical lesionJ Conserv Dent 2013 16:261-64. [Google Scholar]
[9]. Michelle AS, Robert RW, Richard EW, Determining the Optimal Obturation Length: A Meta-Analysis of LiteratureJ Endod 2005 31:271-74. [Google Scholar]
[10]. Se-Lim O, Ashraf F, Sang HP, Treatment strategy for guided tissue regeneration in the combined endodontic periodontal lesions: case report and reviewJ Endod 2009 35:1331-36. [Google Scholar]