Keratoameloblastoma A Rare Entity: A Case Report
Sangeeta J. Palaskar1, Rasika B. Pawar2, Deepakkumar D. Nagpal3, Swati S. Patil4, Pargatsingh T. Kathuriya5
1 Professor and Head, Department of Oral Pathology and Microbiology, Sinhgad Dental College and Hospital, Vadagaon (bk), Pune, Maharashtra, India.
2 Postgraduate Student, Department of Oral Pathology and Microbiology, Sinhgad Dental College and Hospital, Vadagaon (bk), Pune, Maharashtra, India.
3 Reader, Department of Oral Pathology and Microbiology, Sinhgad Dental College and Hospital, Vadagaon (bk), Pune, Maharashtra, India.
4 Postgraduate Student, Department of Oral Pathology and Microbiology, Sinhgad Dental College and Hospital, Vadagaon (bk), Pune, Maharashtra, India.
5 Postgraduate Student, Department of Oral Pathology and Microbiology, Sinhgad Dental College and Hospital, Vadagaon (bk), Pune, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rasika Pawar, Postgraduate Student, Department of Oral Pathology and Microbiology, Sinhgad Dental College and Hospital, Vadagaon (bk), Pune, Maharashtra-411041, India. E-mail : rasikapawar0710@gmail.com
Ameloblastoma is the second most common odontogenic tumour of oral cavity; which has several different histological variants such as follicular, plexiform, acanthomatous, granular cell, desmoplastic, basal cell, clear cell, hemangiomatous, mucous cell differentiation and keratoameloblastoma. It is common in posterior mandible and has high male predilection in the ratio of 3:1. This report presents a case of keratoameloblastoma in 65-year-old female patient in the anterior mandible region with literature review on clinical features, histopathological findings, radiological appearance and treatment options.
Ameloblastoma, Acanthomatous, Histological variants, Mandible
Case Report
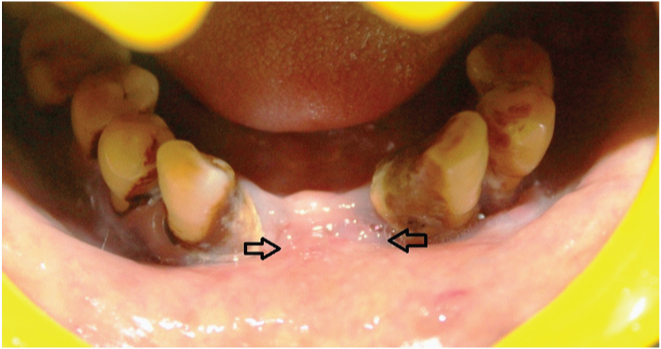
A 65-year-old female presented with a complaint of pain and swelling in the anterior mandible since 2 to 3 months. Patient’s family history and medical history were not contributory. On examination, a single swelling was seen in mandibular labial vestibule extending from left to right canine region, measuring around 7 X 3 cm in its greatest diameter, covered with smooth surface and pale pink in colour [Table/Fig-1]. Teeth in the area of lesion were missing and lesion was obliterating the labial vestibule making cortical expansion obvious. Palpation revealed a firm, non tender swelling with regular borders.
Swelling in the anterior mandible causing obliteration of labial vestibule
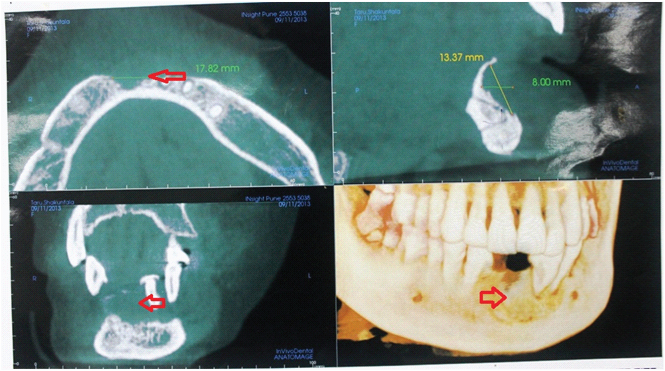
Patient underwent fine needle aspiration cytology, which was suggestive of giant cell lesion. Hence provisional diagnosis was made as central giant cell granuloma. Radiological examination revealed perforation of labial cortical plate in lateral view. Cone beam computed tomography scan revealed erosion of mandible suggesting a neoplastic process [Table/Fig-2]. Taking into consideration the cytological and radiological findings, the lesion was surgically excised and the tissue was sent for histopathological examination.
Cone beam computed tomography revealed unilocular radiolucent lesion causing erosion of bone
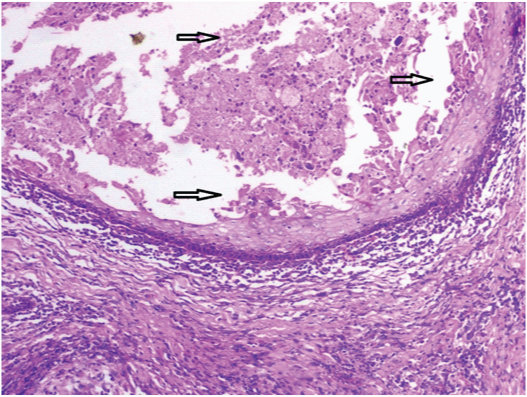
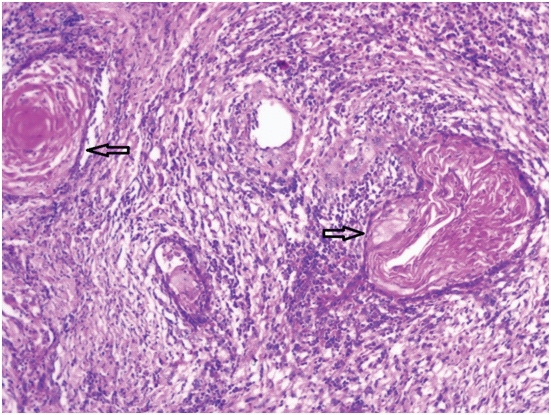
Microscopic examination of excised specimen revealed follicles and plexiform patterns lined by ameloblast like cells with extensive squamous metaplasia and keratin formation in the center [Table/Fig-3]. Connective tissue stroma displayed lamellated stacks of keratin pearls. Dense chronic inflammatory cell infiltrate was found around the large keratin pearls in the connective tissue stroma. Multinucleated reactive giant cells were also found [Table/Fig-4]. These features suggested the diagnosis of keratoameloblastoma. On follow-up after 4 months, patient reported with the same lesion on the same site, keep in mind the lesion has recurred, the surgeons then performed block resection of the anterior mandible. Later patient lost the follow-up.
Photomicrograph showing ameloblastic follicles with squamous metaplasia in the center (10X)
Photomicrograph showing extensive areas of keratin deposition surrounded by chronic inflammatory cells in the connective tissue stroma (10X)
Discussion
Keratoameloblastoma is an extremely rare variant of ameloblastoma [1] with only 17 cases reported in the literature till October 2014. In 1992, the World Health Organization (WHO) defined KA as an ameloblastoma with extensive keratinization, although the recent WHO classification for odontogenic Tumour has not mentioned this term [2,3]. WHO accepted this lesion in histologic spectrum of acanthomatous ameloblastoma due to focal keratinization [4]. According to Norval et al., KA is a variant of acanthomatous ameloblastoma [2,5]. The reported 17 cases of KA are summarized in [Table/Fig-5].
Review of previously reported cases of kearatoameloblastoma with clinical, radiographic, and histologic features
| Sr. No. | Author | Age/ Gender | Clinical features | Radiographic features | Histopathologic features | Treatment | Follow ups |
|---|
| 1 | Pindborg [6] | 57/F | Right mandibular body and ramus | Multilocular radiolucency | Papilliferous histology | Unknown | unknown |
| 2 | Altini et al., [7] | 28 /M | Anterior maxilla | Multilocular radiolucency | Simple histology | Wide local excision | unknown |
| 3 | Altini et al., [8] | 76/ M | Right mandible | Multilocular radiolucency | Papilliferous histology | Hemi mandibulectomy | No evidence till 12 months |
| 4 | Siar et al., [9] | 30/ M | Anterior mandible | Multilocular radiolucency | Simple histology with OKC like features | Resection | Unknown |
| 5 | Siar et al., [9] | 35/M | Left mandible | Unknown | Simple histology with OKC like features | Hemi mandibulectomy | Unknown |
| 6 | Siar et al., [9] | 35 /F | Right maxilla | Ground glass with indistinct borders | Simple histology with OKC like features | Unknown | Unknown |
| 7 | Siar et al., [9] | 39/ F | Left anterior mandible | Unilocular radiolucency | Simple histology with OKC like features | Enucleation | Unknown |
| 8 | Norval et al., [5] | 26/ F | Right mandible, erosion of bone | Lobulated radiolucency | Complex histology | Segmental resection | Unknown |
| 9 | Saidal Naief et al., [10] | 26 /M | Right posterior maxilla | Well defined unilocular radiolucency | Simple histology with OKC like features | Curettage and partial maxillectomy | Recurrence after curettege with in 6 month. Unknown after maxillectomy |
| 10 | Kaku T [11] | 35 /M | Right body of mandible | Unilocular radiolucency between roots | Simple histology | Unknown | Unknown |
| 11 | Takeda et al., [12] | 76 /M | Left body of mandible | Multilocular radiolucency | Complex histology | Resection | Unknown |
| 12 | Collini P et al., [13] | 62 /M | Right ramus and condyle of mandible | Irregular radiolucency with calcification | Papilliferous histology | Hemi mandilectomy | Two local recurrences at 36 and 38 months |
| 13 | Whitt et al., [2] | 45/M | Anterior maxilla | Unilocular radiolucency with calcification | Complex histology | Currettage | No evidence at 10 month |
| 14 | Adeyemi et al., [1] | 38/ M | Right posterior mandible | Multilocular radiolucency | Stromal parakeratin deposition with focal cystic change in epithelial islands. Areas of myxoid change | Resection of mandible | unknown |
| 15 | Mohanty N et al., [14] | 46 /M | Right posterior mandible | Multilocular radiolucency | Papilliferous histology | Unkown | Unkown |
| 16 | Ketabi MA et al., [15] | 21 /F | Right anterior Mandible | Unilocular radiolucency | Complex histology | Enucleation | No recurrence upto 12 months followup |
| 17 | Raj V et al., [16] | 22/F | Right Posterior Mandible | Unilocular radiolucency | Simple histology with stroma showing myxoid areas and cystic degeneration | Segmental resection | No recurrence upto 24 months followup |
| 18 | Present Case | 65/ F | Anterior Mandible | Unilocular radiolucency | Complex histology except for hard tissue formation | Excision and block resection of mandible | Recurrence after excision within 4 months, Unkown after block resection of mandible |
It has more male predilection than female in the ratio of 3:1. The present case was diagnosed in a female patient. KA is most commonly diagnosed in the age groups ranging from 3rd to 7th decade of life with the mean age of occurrence is 43.8 years [2]. Posterior mandible is more commonly involved followed by maxilla, 13 out of 17 reported cases showed involvement of the mandible where as four cases were present in maxilla [1,3]. In this case the lesion was present anteriorly in the mid -line of mandible.
Radiographic appearance varied from unilocular to multilocular radiolucency with central calcifications seen in two case reports [1–3]. In the present case, unilocular radiolucency was present with erosion of bony margin and perforation of labial cortical plate.
Whitt et al., [2] summarized the histologic features of KA into 4 subtypes as- (1) Papilliferous histology - in which the odontogenic epithelium is in papillary projections into the cystic spaces, (2) Simple type - in which histology represents epithelial follicles filled with parakeratin or orthokeratin and lined by ameloblast like cells with reversal of polarity; (3) Simple with Keratocystic Odontogenic Tumour (KCOT) like features- showed similar features of simple type in addition it contains features of conventional odontogenic keratocyst, (4) Complex histology-consists of epithelial follicles packed with parakeratin or orthokeratin, extrusion of keratin masses into connective tissue stroma in the form of pacinian like stacks with or without foreign body reaction; also there may be hard tissue formation resembling cementum and woven bone [2,3,5]. Our case showed complex histology except for hard tissue formation.
As there is overlap of histologic features between KA and solid variant of KCOT, it is important to distinguish between these two lesions. Features present in KA are- (1) stellate reticulum or its differentiation to squamous cells, granular cells or basal cells; (2) large amount of keratin pearl deposition in the connective tissue [17]. These features are absent in solid variant of KCOT.
The treatment for KA and conventional ameloblastoma or solid variant of KCOT is same i.e. block resection [18]. However, it is difficult to assess whether the biologic behavior of KA differs from other histologic types of ameloblastomas due to less no of cases reported in the literature. In the present case, the patient reported with recurrence in the same region during the follow up after four months and operated for the same. After that, patient lost the follow-up. Out of 17 cases reported in the literature, two cases had recurred. Therefore, the incidence of recurrence of keratoameloblastoma cannot be mentioned based on scarcity of the cases reported. Although, it is a combination of two benign but aggressive lesions, the rate of recurrence and malignant potential needs to be studied [19].
Conclusion
KA is a rare tumour. It differs from acanthomatous ameloblastoma having keratin deposition in the connective tissue. Our case showed complex histology without any hard tissue formation which also showed clinical recurrence after four months. It is therefore mandatory to keep follow up of such cases for longer duration to know the biological behaviour of the lesion.
[1]. Adeyemi BF, Adisa AO, Fasola AO1, Akang EE, Keratoameloblastoma of the mandibleJ Oral Maxillofac Pathol 2010 14(2):77-79. [Google Scholar]
[2]. Whitt JC, Dunlap CL, Sheets JL, Thompson ML, Keratoameloblastoma: a Tumour sui generis or a chimera?Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007 104:368-76. [Google Scholar]
[3]. Sisto JM, Olsen GG, Keratoameloblastoma: complex histologic variant of AmeloblastomaJ Oral Maxillofac Surg 2012 70:860-64. [Google Scholar]
[4]. Gardner DG, Heikinheima K, Shear M, World Health Organization Classification of Tumours: Pathology of Head and Neck Tumours 2005 1st edLyon, FranceIARC Press:296 [Google Scholar]
[5]. Norval EJ, Thompson IL, VanWyk CW, An unusual variant of keratoameloblastomaJ Oral Pathol Med 1994 23:465 [Google Scholar]
[6]. Pindborg JJ, Pathology of the dental hard tissues 1970 Philadelphia(PA)W. B. Saunders:381-82. [Google Scholar]
[7]. Altini M, Lurie R, Shear M, A case report of keratoameloblastomaInt J Oral Surg 1976 5(5):245-49. [Google Scholar]
[8]. Altini M, Slabbert HD, Johnston T, Papilliferous keratoameloblastomaJ Oral Pathol Med 1991 20(1):46-48. [Google Scholar]
[9]. Sair CH, Ng KH, “Combined ameloblastoma and odontogenic keratocyst” or “keratinizing ameloblastoma”Br J Oral Maxillofac Surg 1993 31(3):183-86. [Google Scholar]
[10]. Said-al- Naief NA, Lumerman H, Ramer M, keratoameloblastoma of maxilla. A case report and review of literatureOral Surg Oral Med Oral Pathol Oral Radiol Endod 1997 84(5):535-39. [Google Scholar]
[11]. Kaku T, Keratoameloblastoma of the mandibleJ Oral Pathol Med 2000 29:350 [Google Scholar]
[12]. Takeda Y, Satoh M, Nakamura S, Keratoameloblastoma with unique histological architecture: An undescribed variation of ameloblastomaVirchows Arch 2001 439:593 [Google Scholar]
[13]. Collini P, Zucchini N, Vessellhia G, Papilliferous keratoameloblastoma of mandible: A papillary ameloblastic carcinoma: Report of a case with a 6 year follow-up and review of the literatureInt J Surg Pathol 2002 10:149 [Google Scholar]
[14]. Mohanty N, Rastogi V, Misra SR, Mohanty S, Papilliferous keratoameloblastoma: an extremely rare case reportCase Rep Dent 2013 2013:706128doi: 10.1155/2013/706128. Epub 2013 Jun 3 [Google Scholar]
[15]. Ketabi MA, Keratoameloblastoma, a very rare variant of ameloblastomaJ Craniofac Surg 2013 24(6):2182-86. [Google Scholar]
[16]. Raj V, Chandra S, Bedi RS, Dwivedi R, Keratoameloblastoma: Report of a rare variant with review of literatureDent Res J 2014 11:610-14. [Google Scholar]
[17]. Shuster A, Shlomi B, Reiser V, Kaplan I, Solid keratocystic odontogenic Tumour – report of a nonaggressive caseJ Oral Maxillofac Surg 2012 70(4):865-70. [Google Scholar]
[18]. Marx R, Stern D, Oral and Maxillofacial Pathology 2003 Hanover Park, ILQuintessence Publishing:646 [Google Scholar]
[19]. Netto R, Cortezzi W, Merly F, Fróes R, Abrahão A, Keratoameloblastoma: a rare case of recidivation of a rare lesionInt J Oral Maxillofac Surg 2013 42(10):1174 [Google Scholar]