Introduction: Acute kidney injury is a rare and sometimes fatal complication of pregnancy, the incidence of which has been declining worldwide, though still high in developing countries. There are recent observations of increasing incidence in some developed countries attributed to hypertensive disorders of pregnancy.
Materials and Methods: In this study, we have analysed the records of all patients referred to the dialysis unit of a medical college hospital in Karnataka for acute kidney injury related to pregnancy. AKIN (Acute Kidney Injury Network) criteria for the diagnosis of acute kidney injury were adapted. Age, parity, gestational age, causative factors for acute kidney injury, mode of delivery, access to antenatal care, operative procedures, blood component transfusions, number of haemodialysis, time for initiation of haemodialysis, duration of hospital stay and mortality were analysed by finding mean, standard deviation and standard error.
Results: Fifteen patients out of 21563 who delivered in our hospital developed acute kidney injury. These (n=15) were out of 149 patients of acute kidney injury of various aetiologies who underwent haemodialysis between 2012 and 2014. Of these two were unregistered for antenatal care. Ten were multiparous, Eleven were from rural background, one had home delivery, six had vaginal delivery, seven had caesarean section and two had second trimester abortion. Placental abruption with intrauterine death was the commonest Cause in 9 out of 15 cases. All had severe anaemia. Patients received a mean of 3.9 (SD+/- 2.4) sessions of haemodialysis. Eleven patients recovered completely, two died and two left against medical advice.
Conclusion: Obstetric acute kidney injury is associated with poor access to antenatal care, multiparity and rural background. Placental abruption is the commonest cause of obstetric acute kidney injury. Blood component transfusions, avoidance of nephrotoxic drugs and early initiation of haemodialysis are associated with better outcome.
Introduction
Obstetric Acute Kidney Injury is a rare and sometimes fatal complication of pregnancy, the incidence of which is declining worldwide, yet which is a matter of concern in developing countries [1,2]. Paradoxically the prevalence is increasing in some developed countries, the increase being attributed to hypertensive disorders of pregnancy and their management [3].
Occurrence of obstetric acute kidney injury is traditionally described as bimodal, in early pregnancy due to septic abortions and in late pregnancy due to uterine hemorrhage [4]. When treated in time, complete renal recovery is common [1]. Dialysis dependence occurs in 8.4% to 14.25% of patients and is related to several factors like initial resuscitation and time to dialysis [4-7]. Maternal mortality rates ranging from 12.5% to 24.39% are still prevalent due to obstetric acute kidney injury [4-7]. This study was carried out to assess the clinical and etiological profile of obstetric acute kidney injury and the outcome of hemodialysis.
Materials and Methods
Records of all cases referred to the dialysis unit of our medical college hospital by the Department of Obstetrics from January 2012 to December 2014 were analysed.
AKIN (Acute Kidney Injury Network) Criteria for diagnosis of acute kidney injury were adapted [8]. AKIN stage 3 patients were taken for hemodialysis {serum creatine 3 times baseline, or serum creatine more than 4 mg/dl with rise more than 0.5mg/dl, or oliguria with urine output less than 0.3ml/kg/h for 24 h or anuria for 12 h}. Age, parity, gestational age, causative factors for acute kidney injury, mode of delivery, access to antenatal care, number of blood / blood component transfusions, operative procedures, time from the 8onset of azotemia and/or oliguria to the initiation of hemodialysis, hematologic parameters, liver function tests, urine analysis and other laboratory tests as recorded in the case records, type of anticoagulation for hemodialysis, number of hemodialysis and outcome were analysed.
Complete recovery meant dialysis independence after six weeks of initiation. Partial recovery meant dependence on hemodialysis after six weeks of initiation. All cause mortality was also recorded.
Statistical Analysis
Mean values of hemoglobin, platelet count, leukocyte count, duration of hospital stay, number of hemodialysis, blood transfusions were calculated. Standard deviation (SD) was calculated using the formula for n<30. Chisquare test was done to assess the significance of difference between different proportions. Comparison of duration of hospital stay ( ≤ 14 days or ≥ 14 days) with mean scores of different parameters by Mann-Whitney U test.
Results
During the three years from 2012 to 2014, a total of 149 patients underwent hemodialysis. Of these, 15(n) were due to obstetric acute kidney injury. Six obstetric acute kidney injuries occurred out of 7956 deliveries (0.075%) in 2012, 6 again out of 7424 deliveries (0.080%) in 2013 and 3 out of 6183 (0.049%) in 2014. Ten were multipara, 11 were from rural areas and two were not registered anywhere for antenatal care. Ten patients out of fifteen were referred from peripheral hospitals. One patient had home delivery while 14 delivered in hospitals. The demographic profile of patients is shown in [Table/Fig-1]. Referral from other peripheral health care facilities was found to have statistical significance (p<0.05).
Of these patients; two had second trimester abortions, seven had caesarian sections and six had vaginal deliveries. Three patients underwent postpartum hysterectomy after caesarian section and one, after vaginal delivery to control bleeding. Two patients of caesarian section underwent B-Lynch. One patient had a second laparotomy followed by bilateral internal iliac artery ligation [Table/Fig-2].
The commonest cause 9 of acute kidney injury in our study was abruptio placenta (c2=25.65, p<0.01). Eleven patients had multiple factors causing acute kidney injury. The main etiologies contributing to acute kidney injury are shown in [Table/Fig-3].
Eight patients had received amikacin after surgery, five had received diclofenac sodium and two had received both (before referral from peripheral hospital). One had received frusemide when oliguric with ecclampsia. This patient previously had also received amikacin.
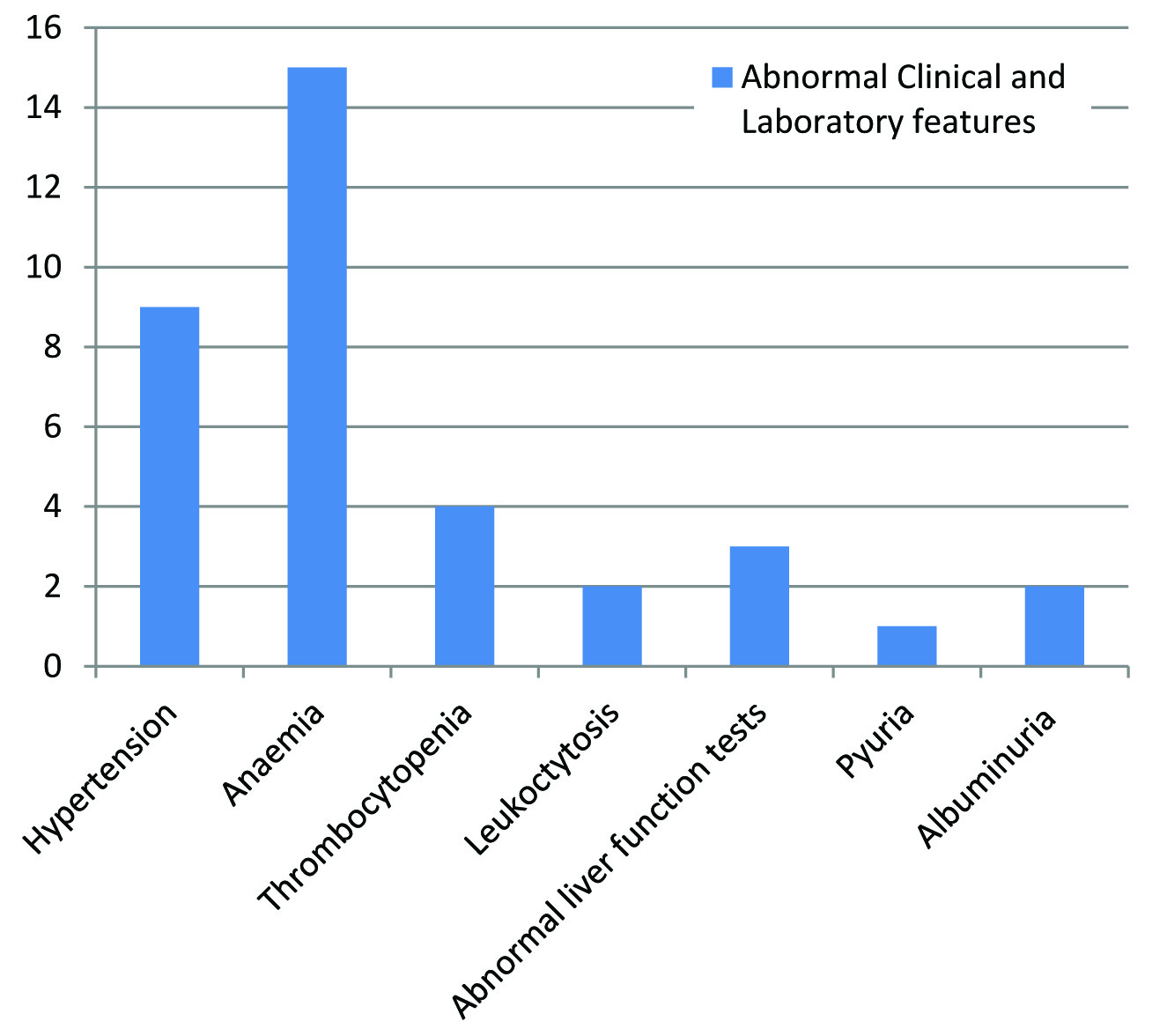
Abnormalities in BP and laboratory parameters are depicted in [Table/Fig-4]. Nine patients had pregnancy induced hypertension (including one who had ecclampsia). All patients were anemic {Mean hemoglobin 5.8 gm%, SD ± 1.3, SE 0.3}. All patients received blood component transfusions {Mean 3.5 units of packed cells, SD ± 2.6, SE 0.7}. Mean Values of these parameters are depicted in [Table/Fig-5].
The time from diagnosis of acute kidney injury to initiation of hemodialysis was an average of 2.93 d with SD ± 2.81. All patients received a mean of 3.9 sessions of hemodialysis with SD ± 2.4. Eight patients received hemodialysis without heparin, two received hemodialysis with heparin and five with reduced dose of heparin.
The average duration of hospital stay was 16.1 days {SD ± 10.81 SE 2.8}. Range of hospital stay was 4 d to 34 d. Longer duration of hospital stay was significantly associated with increased number of hemodialysis [Table/Fig-6].
Eleven out of fifteen patients recovered completely, 2/15 died {1 due to septicemia and multiorgan failure and the other due to fulminant hepatic failure} and 2/15 left against medical advice.
Discussion
Our study reports 15 out of 21,563 deliveries that developed obstetric acute kidney injury requiring hemodialysis through three years {6(0.075%) in 2012, 6 (0.080%) in 2013, 3(0.049%) in 2014}. Whether this trend carries significance is unclear. A study conducted in Canada by Mehrabadi A, et al., [3] reported that there was increasing incidence of obstetric acute kidney injury attributed to hypertensive disorders of pregnancy {1.66 per 10,000 deliveries (0.0166%) in the year 2003-2004 to 2.68 per 10,000 deliveries (0.0268%) in the year 2009-2010}. Incidence in our centre, though decreasing, is higher than their study. Several demographic factors might have influenced the occurrence of obstetric acute kidney injury in our study. In our study, two patients had not received any antenatal care, 10 were referred from other establishments and only three received antenatal clinic services more than twice. One reason for irregular antenatal consultation may be the traditional practice of returning to maternal hometown during late second trimester for delivery causing difficulty in tracking the patients by primary health care service providers {inferred from difference in residential address provided at the time of admission and that of the referral card from the medical establishment last visited in eight patients}.
In our study only one patient had home delivery and all others were at hospital. Patel ML et al., [5] reported 32 (53.3%) who had not received any antenatal care at any stage of their pregnancy and had undergone traditional birth attendant assisted home delivery, 20(33.4%) who had delivered in the hospitals but without prior antenatal care and eight (13.3%) patients who received some sort of antenatal care. In comparison Goplani KR et al., [7] reported 45 (64.28%) hospital deliveries and 11 (15.71%) deliveries at home. Findings of Munib S and Khan SJ [4] were different in that 73(80.25%) did not receive antenatal care and 74 (84%) had home delivery/abortion.
In our study 11/15 (73.3%) were from rural areas. Goplani KR [7] also reported that 30% of patients were urban and 70% were rural. Residence in rural areas would have delayed quick access during the emergency. In our study 10 (66.6%) were multipara. Others reported 46.7% (Patel ML et al.,) [5], 76.55% (Munib S and Khan SJ) [4], 68.57% (Goplani KR et al.,) [7], multiparity in their patients.
Goplani KR et al., [7] observed that post-abortal sepsis was declining in incidence due to legalization of abortion. We noticed two patients out of 15 (13.3%) had abortions and one of them had sepsis. Abruptio placenta with intrauterine death was the commonest cause of acute kidney injury (9 out of 15) in our study. This is in contrast with Patel ML et al., [5] (41.7%), Kilari SK et al., [6] (39.02%) and Goplani KR et al., [7] (61.42%) where septicemia was the commonest cause. The reason may be better access to antibiotics in our place and a tendency to miss placental abruption by the referring hospitals due to lack of ultrasound scan facility. Munib S and Khan SJ [4] noticed that pregnancy induced hypertension was the commonest cause (54.54%) of obstetric acute kidney injury in their study. Our study also had 9 patients with hypertension when referred for dialysis. Whether the hypertension was pregnancy induced or a complication of renal failure was unclear.
Fifteen out of 149 (10.14%) patients who received hemodialysis at our dialysis unit for acute kidney injury had obstetric acute kidney injury. Comparison with other studies is mentioned below in [Table/Fig-7]. In our study 2 (13.3%) died. Various other studies also reported high mortality rates. Kilari SK et al., [6] reported 24.39% mortality, Goplani KR et al., [7] (18.57%), Patel ML et al., (15%) and Munib S [4] (12.5%). Among our patients, 73.3% had complete recovery of renal functions. Others reported 8.4% to 14.28% of irreversible renal dysfunction [4-7].
Some patients had received aminoglycosides or non-steroidal anti-inflammatory drugs or both before the diagnosis of acute kidney injury. Whether changing to other antibiotics and pain control measures post-operatively can reduce obstetric acute kidney injury needs to be studied in the future.
Demographic characteristics
| Sl No | No of patients( n=15) | % of patients |
|---|
| Parity |
| Primi gravida | 5 | 33.33 |
| Multi gravida | 10 | 66.67 |
| Age groups |
| <=22yrs | 8 | 53.33 |
| >=23yrs | 7 | 46.67 |
| Mean ± SD | 23.4 ± 3.6 | |
| Antenatal care |
| Registered at our hospital | 3 | 20.00 |
| At least one antenatal visit at Primary Health Centre or Peripheral hospital | 10 | 66.67 |
| Unregistered | 2 | 13.33 |
| Location/residence |
| Urban | 4 | 26.67 |
| Urban | 11 | 73.33 |
Mode of delivery and operative procedures
| Mode of delivery | No of patients (n=15) | % of patients |
|---|
| Abortion | 2 | 13.33 |
| Lower Segment Caesarian Section (LSCS) | 2 | 13.33 |
| LSCS+B-Lynch | 2 | 13.33 |
| LSCS + Postpartum Hysterectomy | 3 | 20 |
| Vaginal delivery +Postpartum Hysterectomy | 1 | 6.67 |
| Vaginal delivery | 5 | 33.33 |
Causes of acute kidney injury related to pregnancy.
| Abruptio Placentae | 09 |
|---|
| Postpartum Haemorrhage | 01 |
| Septic Abortion | 01 |
| Puerperal sepsis | 01 |
| Ecclampsia | 01 |
| Acute Fatty Liver of Pregnancy | 01 |
| Disseminated Intravascular Coagulation | 01 |
(n=15) (Please note: many patients had more than 1 contributory factor)
Abnormal Clinical and Laboratory Features (apart from azotemia) in patients who had obstetric acute kidney injury.
Mean and SD for different laboratory parameters
| Variables | Mean±SD |
|---|
| Hemoglobin(g/dl) | 5.81±1.33 |
| Platelet count(cells/mm3) | 174800±109753 |
| White Blood Count (cells/mm3) | 12726.67±4215.53 |
| Total protein(mg/dl) | 4.80±0.74 |
| Serum albumin(mg/dl) | 2.66±0.32 |
| Time from ARF to dialysis (days) | 2.93±2.81 |
| Number of dialyses | 3.93±2.37 |
| Duration of hospital stay (days) | 16.13±10.76 |
Comparison of duration of hospital stay (≤14d and >14d) with mean scores of different laboratory parameters by Mann-Whitney U-test.
| Parameters | Summary | <=14days | >=15days | Total | Z-value | p-value |
|---|
| Hb(g/dl) | Mean | 6.3 | 5.3 | 5.8 | -1.2280 | 0.2190 |
| SD | 1.5 | 1.0 | 1.3 | |
| SE | 0.6 | 0.3 | 0.3 |
| Platelet Count (cells/mm3) | Mean | 136571.4 | 208250.0 | 174800.0 | -0.9290 | 0.3530 |
| SD | 82740.3 | 124433.3 | 109753.8 | |
| SE | 31272.9 | 43993.8 | 28338.3 |
| WBC (cells/mm3) | Mean | 12385.7 | 13025.0 | 12726.7 | -0.4680 | 0.6400 |
| SD | 4902.2 | 3837.3 | 4215.5 | |
| SE | 1852.9 | 1356.7 | 1088.4 |
| RBC transfusions In units | Mean | 2.6 | 4.3 | 3.5 | -1.1090 | 0.2670 |
| SD | 1.9 | 3.1 | 2.6 | |
| SE | 0.7 | 1.1 | 0.7 |
| Time from ARF to dialysis (days) | Mean | 2.7 | 3.1 | 2.9 | -0.6720 | 0.5010 |
| SD | 1.3 | 3.8 | 2.8 | |
| SE | 0.5 | 1.3 | 0.7 |
| No of dialysis | Mean | 2.1 | 5.5 | 3.9 | -3.0900 | 0.0020* |
| SD | 1.1 | 2.1 | 2.4 | |
| SE | 0.4 | 0.7 | 0.6 |
*p<0.05
Comparision of the frequency of occurrence of obstetric acute kidney injury with other studies
| Author | Number of cases of obstetric acute kidney injury out of total number of acute kidney injuries. | As a percentage of total number of acute kidney injuries. | Duration of study | Calculated Average per year |
|---|
| Munna Lal Patel [5] (2013) | 60/520 | 11.5% | 1 year | 11.5% |
| Kilari Sunil Kumar [6] (2005) | 41/966 | 04.24% | From July 1999- Dec 2004. | 0.94% |
| K.R. Goplani [7] (2014) | 70/772 | 9.06% | From January 2004 to May 2006. | 2.58% |
| Present Study (2014) | 15/149 | 10.14% | From January 2012 to December 2014 | 3.38% |
Conclusion
Obstetric acute Kidney Injury was associated with high morbidity and mortality. It was more common in multipara and in women who had received inadequate antenatal care, than in primipara and in women who had received adequate antenatal care. Severe anemia was associated with this condition. Abruptio placenta was the commonest cause for obstetric acute kidney injury. Blood component transfusions and early initiation of dialysis were associated with quick recovery and better renal outcome. Changing anti-biotic policy and pain control needs to be studied for reducing the incidence of obstetric acute kidney injury.
*p<0.05
[1]. N Khanal, Ejaz Ahmed , F Akhtar, Epidemiology, Causes and Outcome of Obstetric Acute Kidney Injury. Novel Insights on Chronic Kidney DiseaseAcute Kidney Injury and Polycystic Kidney Disease 2012 :67-84. [Google Scholar]
[2]. J Prakash, R Vohra, IA Wani, AS Murthy, PK Srivastva, K Tripathi, Decreasing incidence of renal cortical necrosis in patients with acute renal failure in developing countries: a single centre experience of 22 years from Eastern IndiaNephrology Dialysis Transplantation 2007 22(4):1213-17. [Google Scholar]
[3]. A Mehrabadi, S Liu, S Bartholomew, JA Hutcheon, LA Magee, MS Kramer, Hypertensive disorders of pregnancy and the recent increase in obstetric acute renal failure in Canada: population based retrospective cohort studyBMJ 2014 4731:1-12. [Google Scholar]
[4]. S Munib, SJ Khan, Outcomes of pregnancy related acute renal failureRMJ 2008 33(2):189-92. [Google Scholar]
[5]. ML Patel, R Sachan, Radheshyam P Sachan, Acute renal failure in pregnancy: Tertiary centre experience from North Indian PopulationNigerian Medical Journal 2013 54(3):191-95. [Google Scholar]
[6]. SK Kilari, RK Chinta, SK Vishnubhotla, Pregnancy related acute renal failureJ Obstet Gynecol India 2006 56(4):308-10. [Google Scholar]
[7]. KR Goplani, PR Shah, DN Gera, M Gumber, M Dabhi, A Feroz, Pregnancy – related acute renal failure: A single center experienceIndian Journal of Nephrology 2008 18(1):17-21. [Google Scholar]
[8]. RL Mehta, JA Kellum, SV Shah, BA Molitoris, C Ronco, DG Warnock, Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injuryCritical Care 2007 11(2):1-8. [Google Scholar]