Gossypiboma Mimicking as Dermoid Cyst of Ovary: A Case Report
Dalia Rafat1, Seema Hakim2, Noor Afshan Sabzposh3, Nasreen Noor4
1Assistant Professor, Department of Obstetrics & Gynaecology, J N Medical College & Hospital, Faculty of Medicine, Aligarh Muslim University, Aligarh, UP, India.
2Professor, Department of Obstetrics & Gynaecology, J N Medical College & Hospital, Faculty of Medicine, Aligarh Muslim University, Aligarh, UP, India.
3Professor, Department of Obstetrics & Gynaecology, J N Medical College & Hospital, Faculty of Medicine, Aligarh Muslim University, Aligarh, UP, India.
4Assistant Professor, Department of Obstetrics & Gynaecology, J N Medical College & Hospital, Faculty of Medicine, Aligarh Muslim University, Aligarh, UP, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dalia Rafat, Assistant Professor, Department of Obstetrics & Gynaecology, J N Medical College & Hospital, Faculty of Medicine, Aligarh Muslim University, Aligarh, UP -202002, India.
E-mail: drdaliarafat.16@gmail.com
Gossypiboma is a rare condition caused by retained postoperative foreign bodies. The condition is under reported because of diagnostic difficulties and medicolegal implications associated with it. It may mimic a benign or malignant soft-tissue tumour in the abdomen and pelvis. A 22-year-old woman presented with non specific symptoms and was referred to us with radiological diagnosis of dermoid cyst. On laparotomy the mass was proved to be a gossypiboma resulted from gauze which was retained in caesarean section done two years back. Although gossypiboma is rarely seen in daily clinical practice, it should be considered in the differential diagnosis of postoperative patients presenting with non specific complains and lump abdomen. Despite thorough history, physical examination, laboratory, and radiographical findings, usually gossypibomas are not suspected and remain an accidental finding. Employment of all preventive measures during surgical procedures and high index of suspicion in post operative patients are the key stones in its management.
Gossypiboma, Pelvic mass, Retained surgical swab, Textiloma
Case Report
A 22-year-old lady presented to her primary care physician complaining of progressive discomfort and heaviness in lower abdomen. Her work-up included an ultrasonograph of the abdomen and pelvis, which showed an intra-abdominal mass. The patient was therefore referred to Jawahar Lal Nehru Medical College, for further management. The patient thus presented in our outpatient department with complains of discomfort and heaviness in lower abdomen since two months. The patient used to have slight discomfort in lower abdomen since six months but from past two months the discomfort has increased and she has started feeling heaviness and swelling in lower abdomen also. There was no history of fever, chill, nausea, vomiting, constipation, dysuria or body weight loss. Her past medical and surgical history was insignificant except for history of a caesarean section two years back. Her surgical records showed that it was an emergency caesarean section and blood transfusion was done for increased per operative blood loss, however postoperative period was uneventful and she was discharged on eighth day in good health.
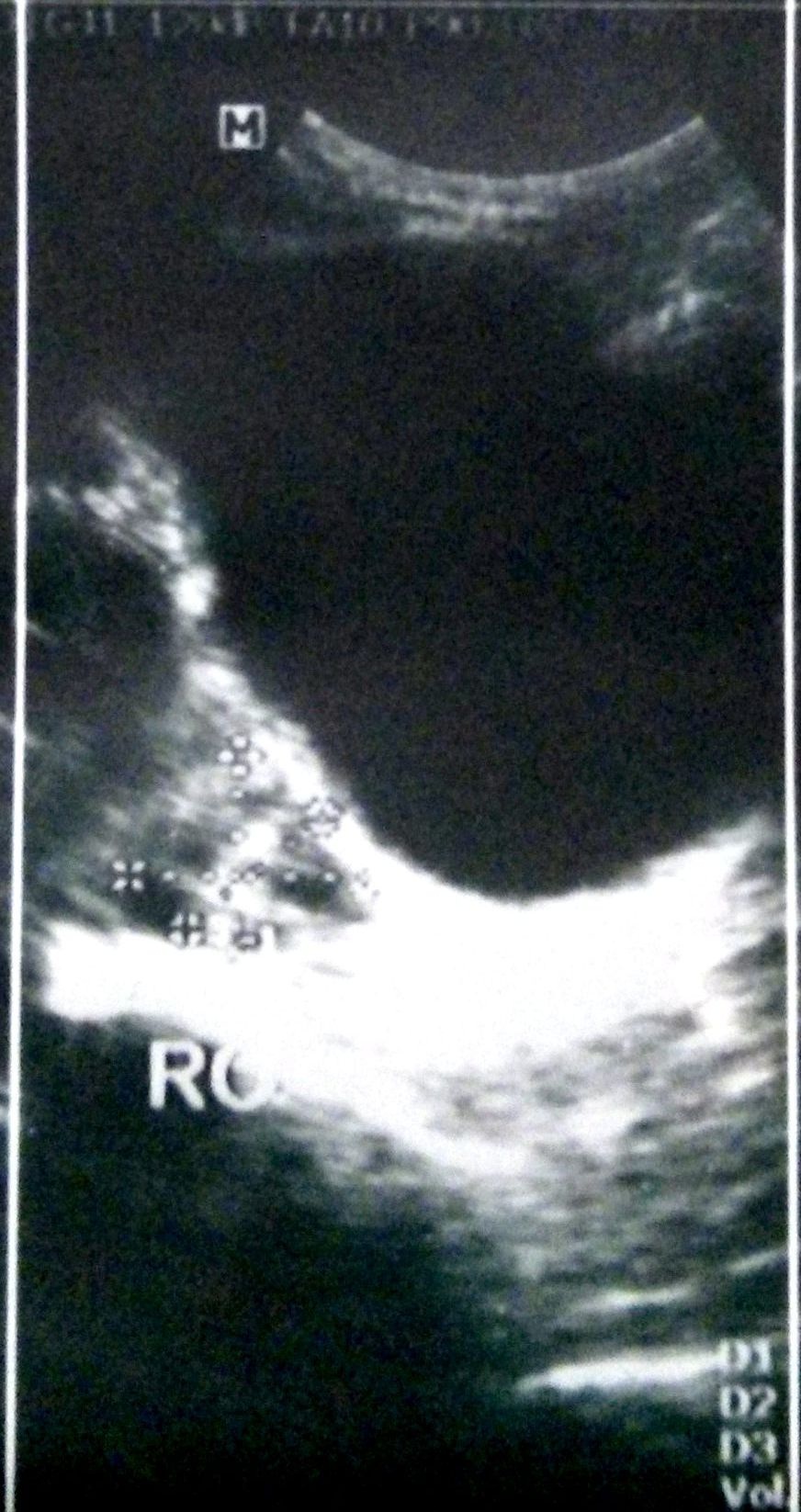
On physical examination vital signs were normal. On abdominal examination, a smooth, round, mobile, non tender mass was palpable in right lower quadrant. On bimanual pelvic examination uterus was normal in size and anteverted and a round, mobile, non tender mass of about 7cm × 8 cm was felt in right adnexa separate from and anterior to the uterus. The blood cell count, blood chemistries, and urinalysis were all within the normal range. The ultrasound ordered by the referring facility revealed a heterogenous lesion of 6 cm×7 Reportcm in the right adnexa. The lesion showed echogenic foci and multiple linear reticular echogenic structures within it with anechoic area at the base of lesion, suggesting dermoid cyst of right ovary [Table/Fig-1]. The left ovary was normal and the right ovary was not visualized. Patient refused for further confirmatory investigations due to non affordability so decision for exploratory laparotomy was taken.
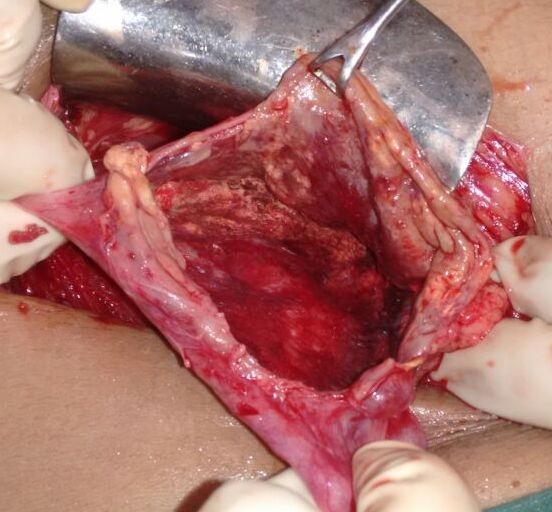
At laparotomy, a 6 cm×7 cm well-encapsulated mass was seen in the pelvic cavity at the right broad ligament with moderate adhesions to peritoneum, the adjacent small bowel and omentum [Table/Fig-2]. Uterus and bilateral ovaries were normal. To remove the mass as a whole, the adhesions were sharply dissected but in doing so the wall opened up and about 40 ml of yellowish, amorphous material was drained and a piece of gauze was removed from the cystic lesion [Table/Fig-3&4]. The postoperative course was uneventful and the patient was discharged home on the eighth postoperative day.
Discussion
Gossypiboma (also called textiloma or retained surgical sponge) is a rare condition caused by retained postoperative foreign bodies. The term gossypiboma is derived from the Latin word gossypium, meaning cotton, and the Kiswahili word boma, meaning place of concealment.
The incidence of gossypiboma is difficult to estimate because of diagnostic difficulties associated with it and lack of documentation secondary to the possible legal ramifications. However, the incidence varies between 1/100 and 1/5000 laparotomies [1-4]. Despite of all the precautions being taken before, during, and after surgical procedures, foreign bodies are still occasionally left behind in the peritoneal cavity. As the symptoms of gossypiboma are usually nonspecific and may appear years after surgery, the diagnosis of gossypiboma may be difficult, and it may mimic a benign or malignant soft-tissue tumour in the abdomen and pelvis, as is the case with our patient.
Operative loss of surgical objects usually result from circumstances where either initial counts are often hurried or omitted like in surgical emergencies, haemorrhagic procedures or change in operating theatre staff; or in time-consuming operations and in operations in anatomical regions difficult to reach [2,5]. The time interval between the original operation and the diagnosis of retained foreign body is variable and vary from a few weeks after surgery to several years later. Also, their clinical presentation is protean and depends on the location and the type of reaction they can evoke. Retained foreign bodies can lead to two different types of body responses [6]. One is an exudative type which usually occurs early in the postoperative period and may lead to abscess formation with or without bacterial super-infection. The other is the aseptic fibrinous response which usually presents late in the postoperative period and results in adhesion or encapsulation leading to granuloma formation. Mostly patient presents with latter type of response and accordingly, the diagnosis is usually difficult because of less severe symptoms and the delay in onset from previous surgery. Patients usually remain asymptomatic and the diagnosis is either incidental, or they present with pseudo tumour syndrome [3,7,8]. On the other hand, patients with former type of response usually presents much earlier with resultant abscess and chronic external or internal fistula into an adjacent adherent hollow organ such as the stomach, intestine, bladder, sigmoid colon or vagina [9-11], leading to varied complications.
The differential diagnosis of gossypiboma is proposed depending on the form of its presentation and commonly includes tumour or tumour recurrence, tuberculosis, postoperative adhesions, invagination, and intraabdominal abscess [12]. The diagnosis is often not easy based on history and physical examination, so familiarity with the imaging features of gossypiboma is important. Many radiologic findings are characteristically used to diagnose gossypiboma. The retained sponge containing a radiopaque marker can be easily diagnosed by conventional radiography except when it breaks into pieces or if the radiopaque marker becomes bound or folded in which case the retained sponge might not be identified at conventional radiography [5]. On sonography, a retained sponge is seen as a well-defined hypoehoic mass with a wavy hyperechoic area and dense acoustic shadowing [12] while CT scans typically reveals it as a well-defined soft-tissue mass and may show a whorled texture or a spongiform pattern with contained gas bubbles [13]. On MRI, gossypiboma manifest as a well-defined mass that showed a peripheral wall of low signal intensity at T1- and T2-weighted imaging and enhancement at contrast-enhanced T1-weighted imaging. The serrated contour in the inner border of the peripheral wall was shown at contrast-enhanced T1-weighted imaging and on T2-weighted imaging; the whorled stripes within the central portion were characteristically shown as low signal [14,15].
As with many other medical problems prevention is better than cure for gossypibomas. Implementation and strict adherence to following measures is of utmost importance. Meticulous preoperative and postoperative counting of all surgical materials, routine use of sponges impregnated with a radio-opaque marker and thorough exploration of the abdominal cavity at the conclusion of the surgery even in the face of correct counts.
Despite thorough history, physical examination, laboratory, and radiographical findings, usually gossypibomas are not suspected and remain an accidental finding. Often the presumptive diagnosis is that of a tumour. This is especially true in situations like in our case, where extensive preoperative workup is not feasible either due to non affordability or non compliance of the patient.
Sonographic appearance of retained gauze, mimicking as dermoid cyst of ovary
Intraoperative appearance of gossypiboma

Thick walled cavity after removal of gauze
Retained surgical gauze, 6 × 3 cm in size

Conclusion
In conclusion the situation is double pronged. On one hand there is diagnostic dilemma, and on other hand it carries medico-legal implications. Wide awareness is mandatory to avoid unnecessary psychological and physical morbidity, associated with misdiagnosis of the condition and employment of unnecessary aggressive surgical approach. Also, a high index of suspicion is required in postoperative patients presenting with non specific complains.
[1]. AF Rehmat Ullah, S Shuja, S Gazozai, Intra-Abdominal Surgical Gauze Pseudotumour (Gossypiboma) Mimicking A Dermoid CystInt J Pathol 2012 10(2):85-87. [Google Scholar]
[2]. I Taçyildiz, M Aldemiry, The Mistakes of Surgeons: “Gossypiboma”Acta chir belg 2003 103:71-75. [Google Scholar]
[3]. J Serra, X Matias-Guiu, R Calabuig, P Garcia, FJ Sancho, JP La Calle, Surgical gauze pseudotumourAm J Surg 1988 155:235-37. [Google Scholar]
[4]. K Slim, T Ben Slimane, C Dziri, R Mzabi, Textile foreign bodies left in the abdomenAnn Radiol (Paris) 1990 33:280-83. [Google Scholar]
[5]. W Rappaport, K Haynes, The retained surgical sponge following intra-abdominal surgery: a continuing problemArch Surg 1990 125:405 [Google Scholar]
[6]. T Mochizuki, Y Takehara, K Ichijo, T Nishimura, M Takahashi, M Kaneko, Case Report: MR Appearance of a retained surgical spongeClin Radiol 1992 46:66-67. [Google Scholar]
[7]. JW Hyslop, KI Maull, Natural history of the retained surgical spongeSouth Med J 1982 75:657-60. [Google Scholar]
[8]. NM Gupta, A Chaudhary, V Nanda, Retained surgical sponge after laparotomy. Unusual presentationDis Colon Rectum 1985 28:451-53. [Google Scholar]
[9]. BB Mentes, E Yilmaz, M Sen, Transgastric migration of a surgical spongeJ Clin Gastroenterol 1997 24:55-57. [Google Scholar]
[10]. K Kato, T Kawai, K Suzuki, Migration of surgical sponge retained at transvaginal hysterectomy into the bladder: a case reportHinyokika Kiyo 1998 44:183-85. [Google Scholar]
[11]. T Manabe, H Goto, S Mizuno, A case of retained surgical sponge penetrated into the sigmoid colonNippon Igaku Hoshasen Gakkai Zasshi 1997 57:279-80. [Google Scholar]
[12]. PR Lauwers, RH Van Heey, Intraperitoneal gossypibomas: the need to count spongesWorld J Surg 2000 24:521-27. [Google Scholar]
[13]. S Sugano, T Suzuki, M Iinuma, Gossypiboma: diagnosis with ultrasonographyJ Clin Ultrasound 1993 21:289-92. [Google Scholar]
[14]. A Kalovidouris, D Kehagias, L Moulopoulos, A Gouliamos, S Pentea, L Vlahos, Abdominal retained surgical sponges: CT appearanceEur Radiol 1999 9:1407-10. [Google Scholar]
[15]. CK Kim, CK Park, H Ha, Gossypiboma in Abdomen and Pelvis: MRI Findings in Four PatientsAJR 2007 189:814-17. [Google Scholar]