World Health Organization (WHO) stated rational use of drugs requires that patients receive medication appropriate to their clinical needs, in doses that meet their own individual requirement for an adequate period of time and at the lowest cost to them and their community”[1]. To investigate the rational use of drugs, WHO have established few core indicators, viz. prescribing indicators, patient care indicators and health facility indicators [2]. Prescribing indicators included number of drugs prescribing per encounter, percentage of drugs prescribed by generic name, percentage of encounter by injection and antibiotics prescription and percentage of drugs prescribed from essential medicine list (EML) [2].
Prescription is written medico-legal document by authorized person for the treatment of patient where each prescription should contain all the four elements, superscription, subscription, inscription and signature with registration number issued by medical council [3]. In superscription, information of doctor (qualification, address) and patient (name, age, sex address) as well as date of prescription are included. The subscription should include to the information regarding drug prescribed, like, dosage form, drug name, its dose, number of drugs etc. While directions for the use of drug needs to be mentioned in inscription. Finally, signature of the registered medical practitioner with their registration number at medical council should be written as last element of prescription [4].
All prescription orders should be clearly written by prescriber so it can easily communicate between pharmacist and patient [5]. Prescribing errors can be observed if sufficient and necessary information’s are not mentioned in prescription [5]. These include errors involving omission of needed information; poor hand-writing perhaps leading to errors of drug dose or timing; and prescription of drugs that are inappropriate for the specific situation. Prescribing errors promote the irrational use of drugs and decrease patient compliance [6].
Study by Kuo et al., reported that 70% prescribing errors was observed among United States America (USA) family physicians while study conducted at West England reported that 43.8% prescriptions contain one or more prescribing errors [7,8]. Study carried out at Nasik, India reported that out of 300 prescriptions 279 prescriptions (93%) were irrational based on the use of essential drug WHO and standard treatment guidelines [9].
There is lack of data of study of prescribing analysis at private hospitals in India and also in our city. Hence we carried out this study to know the prescription analysis of outdoor patients’ prescriptions among private hospital at our city.
Materials and Methods
The prospective, observational study carried out at different private hospitals of our city after taking due permission from medical director or head of the hospital for a period of three months (August to October) 2012. We approached 32 private hospitals out of these 10 hospitals gave permission to conduct study. From each hospital 25 prescriptions were taken. They were taken after consent of patient or care taker at hospital pharmacy during predefined day time period between 10 am to 12 pm. The prescriptions were collected irrespective of diagnosis, age, gender, etc across various departments of the hospital. We took photographs of the prescriptions using digital camera. The prescriptions were analysed and appropriate statistical tests were applied.
Results
We collected 250 prescriptions from 10 different hospitals at our city. It was observed that superscription part of the prescription name of the hospital its address, doctor’s name, patient name date of prescription were mentioned in all (100%) prescriptions while they did not mentioned about gender, age and address of the patient in all (100%) the prescriptions. In subscription part of prescription abbreviation for dosage form e.g. ‘T’ for tablet, ‘Inj’ for injection was used in all (100%) the prescription. It was noticed that dose of drug was not completely written in 90% of prescriptions e.g. 100 for 100 mg. Duration of treatment were not mentioned in 80% of prescriptions. In inscription part, direction of use of drug was not properly mentioned in 74% of prescriptions. It was observed that prescriptions were signed by prescribing doctor in all (100%) prescriptions but their medical council registration no. was not mentioned in all (100%) the prescriptions. It was observed that diagnosis was mentioned in 34% of prescription and 86% prescriptions were illegible.
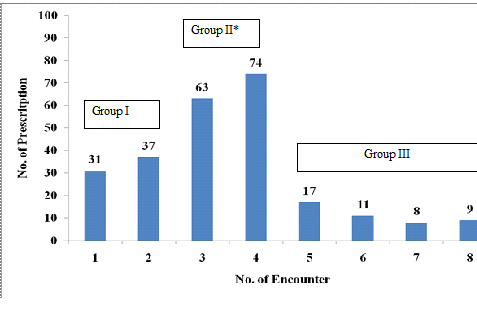
Total 869 drugs were prescribed in 250 prescriptions. It was reported that Group II (3 to 4 encounters) contained 137 (54.8%) prescription which was statistically significant (p<0.05, Z-test) as compared to Group I(less than or equal to 2 encounters) contained 68(27.2%) prescriptions and Group III (more than four encounters) contained 45(18%) prescriptions [Table/Fig-1].
Analysis of prescription per encounter (n=250)
Analysis according to WHO prescribing indicators
* p< 0.05 significantly as compared to group I and group III by Z-test
It was reported that average 3.38±1.79 (Mean±SD) drug were prescribed per encounter. Majority of drugs 811 (93.33%) were prescribed by brand name which was significantly (p<0.05, Z-test) higher as compared to generic name 58 (6.67%) drugs. Percentage encounter with antibiotics and injection form were 53.6% (134 prescriptions) and 20.8% (52 prescriptions) respectively. It was observed that 587(67.54%) drugs were prescribed according to EML of State [Table/Fig-2].
Analysis of prescription according to WHO prescribing indicators (n=250)
| WHO prescribing indicators | Prescription analysis |
|---|
| Average number of drugs per encounter (Mean±SD) | 3.38±1.79 |
| Percentage of drugs prescribed by generic name | 6.67% |
| Percentage of drugs prescribed by brand name | 93.33%* |
| Percentage of encounters with an antibiotic prescribed | 53.6% |
| Percentage of encounters with an injection prescribed | 20.8% |
| Percentage of drugs prescribed from essential medicines list | 67.54% |
* p< 0.05 significantly as compared to generic name by Z-test
Analysis of drugs
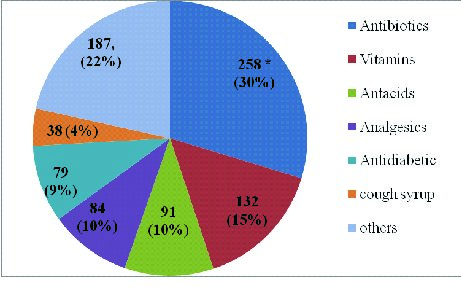
Analysis of drug revealed that antibiotics, analgesics, antacids and vitamins were consumed 65% of prescribed drugs. Cough syrup and anti diabetic drugs were prescribed 4% and 13% of prescribed drugs respectively. Other 22% of prescription contained skin cream, anti-anginal, antihypertensive, lipid lowering agents, diuretics etc [Table/Fig-3].
Analysis of prescribed drugs (n=869)
* p< 0.05 significantly as compared to other drugs by Z-test
Discussion
Our study revealed that there was not fully complete prescription was found. Hospital details like address, patient name date of prescription were mention in 100% prescriptions. Similar to report by Siddarth et al., where it was 99.3% [10]. Gender, age and address of patient were missing in all (100%) the prescriptions similar to study conducted at Maharashtra [11] while Siddarth et al., [10] reported that in 33% and 0.7% prescriptions address and gender were missing. Study conducted at Ethopia [12] and Dubai [13] reported that age, gender were not mentioned in 36.6%, 18.6% and 9.7%, 12% respectively which was lower as compared to our study. In our study age and gender were mentioned in outdoor patient record file of hospital while we observed only prescription part from file. Patient details like age, gender can helpful in certain drug precautions among child and elderly patients as well as contraindicated in pregnant women.
Abbreviations were used in all (100%) prescriptions for dosage form similar to reported by Hazra et al., [14] where it was 95.5%. Study conducted at Nepal and USA reported that 0.65% and 4.7% prescribing errors was due to use of abbreviations respectively [15,16]. An abbreviation used by prescriber may misinterpreting the prescription. Use of abbreviations may save time for prescriber but does not promote patient safety due to prescribing error. Strict guideline must be followed or electronic prescription should be promoted.
In our study duration of treatment, dose, dosage schedule were not properly written in above 70% of prescription while study conducted at Maharashtra [11] and Jammu [17] it was not properly written approximately 35% and 25% respectively. Study conducted at Brazil [18] where 18.2 % prescriptions dose of drug was missing and 6.6% of prescriptions higher dose was mentioned while study conducted at Nigeria [19] duration of treatment, dose, dosage schedule duration of treatment, dose, dosage schedule was missing in 1.6% 5.8% and 6.4% of prescriptions respectively which was lower compared to our study. It might be due to verbal explanation by doctor to patient but patient may forget the instructions and increase chance of medication error. Another reason may be due to lack of time, excessive work for prescribers [18].
It was observed in our study was that all (100%) prescriptions contained doctor’s name with its signature similar to reported by Siddarth et al., [10] where 96.7% of prescription had doctor’s signature but 7.3% of prescription had doctor’s name. We and Siddarth et al both reported that 0% prescription contained medical registration number [10]. Study conducted at Dubai [13] reported that doctor’s name, signature and medical registration number were missing in 10.3%, 12.2 and 54.9% of prescription respectively. Prescription without medical registration number is cause of concerned because it is required for medico-legal case.
It was observed diagnosis was mentioned in 34% of prescription which was higher as compared to reported by Rishi et al., [19] where it was 22.25% but lower compared to reported by Siddarth et al., [10] where it was 97%. It was observed that 86% prescriptions were illegible which was higher as compared to Siddarth et al., [10] and Phalke et al., [11] where it was 6.3% and 17.6% respectively. Study conducted at Shrilanka [20] reported 25.6% illegible prescription which lower as compared to our study. Illegible prescriptions were difficult to read and may increase chance of medication error. So, training to prescribe for legible prescribing should be promoted.
In our study average 3.38±1.79 drugs per encounter were prescribed which was similar to study carried out by Potharaju et al., [21] and Mirza et al., [22] and where it was 3.1 and 3.72 medicines prescribed per patient respectively. Our study report of average drugs per encounter was higher as compared to study conducted at Spain and Sweden where it was 2.3 and 1.4 respectively [23]. Our study report was lower as compared to Ansari et al., [24] where it was 5.05 medicines per prescription in private sector. In our study 119 (47.6%) of prescription four or more drugs were prescribed. It was indicated that the polypharmacy was common in private sector at Western India. It may be due to lack of time for doctor to diagnosing and treating common disease conditions; patient demand of quick and speedy relief from symptoms, availability of irrational fixed drug combinations and unethical marketing practices by pharmaceutical companies [24].
In our study only 6.67% drugs were prescribed by generic name which was higher as compared to reported by Ansari et al., [24] and Mohanty et al., [25] where it was 1.41 and 2% respectively. Kumari et al., [26] reported that 27.1% drugs prescribed by generic name respectively which was higher as compared to our study.
In our study, the prescriptions with generic name prescriptions were lower which is contradict to our pharmaceutical sector as it is one of the biggest supplier of generic drugs in the world
The common reasons for prescribing by brand name by prescriber were
Doubt about efficacy and bioavailability of generic formulations.
Prescribers’ adherence to hospital formulary and drugs prescribed from hospital formulary and pharmacy.
Pharmaceutical companies’ claim about higher efficacy and suitability of brand name and fixed drug combinations.
Percentage of encounters with an antibiotic prescribed was 53.6% in our study which was similar to study conducted at Southern India [25] and Pakistan [27] where it was 57.24% and 52% respectively. Study conducted at Bhopal (India) [28], Iran [29] and Jordan [30] reported that antibiotic percentage of encounter was. 63.5%, 61.9 % and 60.9% which was higher as compared to our study. Antibiotics were most commonly prescribed in our study. Inappropriate and irrational use of antibiotics may lead to increase antibiotic resistant bacteria, increase morbidity and increase health expenditure. Rational use of antibiotics is recommended by WHO and it is more necessary for developing countries like us.
Prescription by injection was observed in 20.8% of prescription which was similar to report by Potharaju et al., [21] where it was 25%. Various other studies from India by Bharity et al., [31], Kumari et al., [26] reported that 13.5%, 1.7% encounter by injection route respectively which was lower compared to our study. Studies conducted at Iran [29] injections were prescribed in 58% of encounters which was higher as compared to our study. Percentage of encounters with an injection prescribed should be as low as possible because of the risk of communicating diseases and the increased use of healthcare resources.
In our study 67.54% drugs were prescribed according to State EML similar to study conducted at Madhya Pradesh [31] where it was 66.9% and previous report from our state where it was 77.61% but lower to study conducted at West Bengal [32] where it was 90.3%. In Nigeria [18] 94% drugs prescribed from EML which was higher as compared to our study while from Shri lanka [20] 39.6% drugs prescribed from EML which was lower as compared to our study. Prescribing from the EML is good clinical practice and improves the rational use of medicines.
Antibiotics was prescribed 30% of drugs which was similar to Mohanty et al., [26] and Dutta et al., [32] where it was 26% and 29.20% of drugs respectively. Study conducted at Madhya Pradesh [31], Lucknow [26] antibiotics was 22.5%, 20.6% of prescribed drugs respectively. Analgesics (10%), antacids(10%) and vitamins (15%)constituted one third of prescribed drugs in our study which was lower to study by Siddharth et al., [10] where analgesics, antacid and vitamins were 23.3.%, 26.33% and 24% respectively. Study conducted at Northern India [19] reported that non-steroidal anti-inflammatory drugs analgesics, antibiotics and vitamins were prescribed 89.75%, 77.25%, and 59.74% respectively which was higher as compared to our study. Study conducted at Dubai [13] reported that antibiotics and vitamins were 21.4% and 5.9% of prescriptions respectively which was lower as compared to our study. Study conducted at Nigeria [18] analgesic and vitamins were 36.2% and 9.7% of prescriptions which was higher and similar to our study respectively. Probable reason for most commonly prescribed of analgesics, antibiotics and multivitamins was that physicians may overestimate the severity of illness and justify its prescribing. Physicians might also under stress due to patient demand of rapid symptomatic relief of symptoms. It was chance to dissatisfaction in patients if the doctor is not prescribed drug [31].
Our study revealed that prescription errors were common in private hospitals. Therefore, educate prescribers to reduce prescribing errors through seminar, conference, workshop are required. There should be also pharmacist and doctor’s joint training for decrease prescription errors. Some errors can be improved by using computerized prescription in hospital. Antibiotics were commonly prescribed drugs in our study and it may lead to drug resistant organisms and increase health burden. So, strict regulation of antibiotic policy in outdoor patients in private hospital is required with availability of antibiotic policy to each prescriber for better management of patients and increase rational use of antibiotics
Limitations
The analysis of prescriptions was not based on diagnosis pattern, which system is involved. Prescriptions from specific groups like pregnant women, children and geriatric patients not analyse and cost of the drugs was not calculated. We could not analysed on rationality of drugs prescribed and WHO core indicators like patient and health facility core indicators. Also we could not get the permission to analyse the prescriptions from some of the well-known private hospital of our city.
Conclusion
Prescribing errors were commonly observed in private hospitals. Antibiotics were commonly prescribed in outdoor patients compared to other group of drugs. Therefore educated to prescriber with good prescribing practice and strict regulation antibiotic policy in outdoor patients in private hospitals are required.
* p< 0.05 significantly as compared to generic name by Z-test