Background: There is always a constant search for a new solution to tackle defects in the limbs. The technique has to be simple, easily reproducible and performed within a short duration. The answer is keystone island flap keystone flap is a simple, less time consuming, durable and easily reproducible option to reconstruct most of the limb defects.
Aim: The aim of this article is to study the usefulness of keystone flap in reconstruction of various upper and lower limb defects.
Materials and Methods: This retrospective review involves study of 20 patients undergoing keystone flap reconstruction for various defects from 2012 to 2014. Patient demographic data, medical histories, comorbidities, surgical indications, defect characteristics and locations, hospitalization, complications and follow-up were evaluated and are presented as uncontrolled case series.
Results: Ages of the patients were ranging from 18 to 65 y with an average of 38.75y. Among the defects, 10 were following trauma (50%), 5 were due to tumour resection (25%), 3 followed debridement of abscess (15%) and another 2 defects were due to surgical wound dehiscence (10%). The largest defect covered by this flap in our study measured 45 x 18 cm and the smallest defect was 8 x4 cm. The average intra-operative time was 45.5 min (range 20-90 min). Fourteen flaps were done to cover lower limb defects (70%), 4 for upper limb defects and 2 were for defects in the axilla. Partial flap necrosis was observed in one case. The average duration of hospital stay of patients was 3.45 d. All patients were followed until they achieved stable, healed wound.The overall success rate was 95%.
Conclusion: Keystone flap can be safely used to cover various limb defects with minimal pain, a sensate cover and excellent cosmetic outcome, minimizing the need for microsurgical techniques or prolonged operative time.
Incision, Malignancy, Perforator flap, Reconstruction
Introduction
The keystone island flap was described by Behan in 2003 [1] . Based on fasciocutaneous perforators, the keystone island flap offers both the robust vascularity of perforator flaps and relative ease and speed of local tissue rearrangement [2] . Other advantages of this technique include short operative time, high reproducibility, ease of use and local tissue aesthetic similarities [2]. This technique possibly obviates the need for microsurgical procedures, additional skin grafts, and extensive operative time [3]. The keystone flap derives its name from its similarity to the architectural keystone piece that marks the central portion of the arch. It employs immediately adjacent skin and soft tissue that provides a good colour match in addition to reconstructing the contour of the defect, so providing a far superior cosmetic result [4].
This paper presents our experience with keystone flaps while managing the defects of upper and lower limb due to trauma or after wide local excision of a malignancy. The study aims to determine the feasibility and safety of keystone island flap in managing various limb defects.
Materials and Methods
This retrospective review involves study of 20 patients undergoing keystone flap reconstruction for various limb defects from March 2012 to February 2014. Patient demographic data, medical histories, co morbidities, surgical indications, defect characteristics and locations, hospitalization, complications and follow-up were evaluated and are presented as uncontrolled case series.
Flap Planning and Design
After excision or debridement, the defect is converted to elliptical shape to favour proper closure without standing cutaneous deformity. Janna2The length and width of the defect is measured intraoperatively. The maximum width is also noted. The side of the defect with greater tissue laxity is chosen as the flap donor area. If a single flap is not sufficient to cover the defect, another flap from the opposite side of the ellipse is marked and kept ready. An incision at 90o at either end of the ellipse meets the curvilinear line of the flap outer margin [2]. One side of the elliptical defect serves as the inner arc of the keystone. The width of the flap equals the width of the defect. The flap length depends upon the length of elliptical excision.
Surgical Technique: Incision is made all along the flap boundary as marked before. The incision is deepened until deep facia, which is also divided all along the outer border. Undermining of the flap border should not be done to prevent injury to fasciocutaneous and musculocutaneous perforators. Minimum undermining can be done on the other side of the defect if there is any tension in the suture line. First suture is taken at the centre of the flap where there is maximum tension. The remaining part of the flap is properly sutured to the defect, closure of the ‘Y’ limb and rest of the flap on the outer border is done using standard technique. Keystone flap should be designed on that side of the defect having maximum skin expansibility. Double flaps may be required to cover larger defects or where there is less expansibility of adjacent skin. This flap survives based on perforators emerging from the underlying tissue.Keystone island flap does not require drain routinely. However, if there is extensive dissection for the primary excision of malignancy or debridement, closed drain is kept for few days.
Results
Twenty patients were included in the study. Ages of the subjects were ranging from 18 to 65 y with an average of 38.75 y. Fourteen cases in our series had distinct risk factors like smoking (30%), diabetes (25%) and radiation therapy (15%). Among the defects, 10 were following trauma (50%), 5 defects were due to tumour resection (25%), 3 were due to debridement of abscess (15%) and the remaining 2 defects were secondary to surgical wound dehiscence (10%).The largest defect covered by keystone flap in our series measured 45 × 18 cm and the smallest defect covered was 8 × 4 cm. The average intra-operative time required to complete the flap was 45.5 min (range 20-90 min). Fourteen key stone flaps were done to cover lower limb defects (70%), 4 flaps were done for upper limb defects (20%) and the remaining 2 were for axillary defects (10%). The average hospital stay was 3.45 d. Oncology patients stayed in the hospital for longer time due to their radiotherapy regimen. All subjects were followed until they achieved stable, healed wound.Regarding complications, partial flap necrosis was observed in one case which required skin grafting (5%). Two other cases had wound infection leading to wound dehiscence, which required secondary suturing. The overall success rate was 95%.
Discussion
Our study of keystone flaps in 20 cases has shown its usefulness for the reconstruction of complex defects with high degree of success. Local transposition flaps done to cover limb defects sometimes result in partial flap necrosis due to lack of vascularity. Transposition flaps can cause contour deformity over the flap and hyperpigmentation of the skin grafted donor area. The keystone flap consists of two V-Y advancement flaps in opposing directions. The movement of these advancement flaps leads to availability of extra tissue adjacent to the defect so as to facilitate primary approximation of skin edges. The flap is designed within various dermatomal precincts, and included in the design are any superficial/deep venous structures or cutaneous nerves which can be incorporated [5]. This technique is simple and easily reproducible by younger surgeons. Microsurgical expertise is usually needed in the vessels’ dissection phase of propeller flap that should be carried out under loupe magnification, in order to follow the chosen nourishing vessels for a short tract into the muscle belly or inside the septa. There is also cosmetic morbidity due to skin graft in the donor area of propeller flaps [6]. Preoperative Doppler flowmetry is usually done to identify perforator vessels in the anatomical area in propeller flaps. This is operator dependent, time consuming and not always accurate in localising the perforating vessels [6]. Keystone flap has minimal donor site morbidity. Small skin graft was used only in one of our cases. In all the remaining cases, the donor areas were closed primarily.
Keystone island flaps can be classified as follows [1] :
Type I: Standard flap design without division of deep fascia.
Type II: The deep fascia on the convex aspect of the flap is divided to enhance mobilization. Further sub categorization (Type II a) secondary defect is closed primarily and (Type II b) secondary defect is closed with a splint skin graft.
Type III: Double keystone flaps are designed to facilitate closure, one on either side of the defect.
Type IV: Up to two- thirds of the flap is undermined. Flap mobilization is maximized.
In our experience, we have observed flap execution is easier over the trunk, gluteal region and thigh, but difficult over knee and distal leg due to deficient skin laxity in the lower leg. It is an excellent option for covering large defects over thigh where there is adequate tissue laxity. Post oncological resection defect (after wide local excision of soft tissue sarcoma) over the anterior aspect of the thigh measuring 35 x 17 cm [Table/Fig-1] was covered using keystone flap from the medial side of thigh [Table/Fig-2]. Another huge defect of 45 x 18 cm over the posterior aspect of the gluteal region and thigh after resection of a recurrent sarcoma [Table/Fig-3] was covered by bilateral keystone flaps on either side of the defect [Table/Fig-4]. Two large defects covered in our study were over the thigh and reconstruction was possible due to skin laxity.
Keystone flap should be attempted with caution in areas of least skin expansibility – around the knee joint,ankle joint, around the elbow joint, plantar aspect of foot and palmar aspect of hand. In one of our cases, to cover a defect below the knee, we had to elevate the distal end of the flap to cover the defect as there was reduced skin laxity. Alternative option should be thought of if there is degloving or avulsion of the soft tissue adjacent to the defect. We routinely incised the margins of the flap through deep fascia. This will facilitate the mobility of the flap to fill the defect. Mobility of the flap can be comparable to a treetop mobility, and possible only after incising the deep fascia all around the convex border of the flap. We have noticed shearing of the flap and increased tension in the suture line in cases where deep fascia was not incised. However, while closing smaller defects and in the presence of sufficient laxity, we have not incised the skin over the central part of the convex surface of the flap to retain more vascularity in the flap, but the deep fascia was incised underneath the skin [Table/Fig-5,6].
Splints were applied routinely to help soft-tissue healing in upper and lower limbs for 3-4 d. Physiotherapy would be required in cases when skin grafting has been done. No long term splinting was followed in any of the patients. Hence bilateral limb procedures can be done in a single sitting.Conventional skin grafts with or without a local flap would involve significant scarring, post operative immobilization, extensive physiotherapy, graft pressure therapy, etc. We have operated on a case of bilateral axillary hidradenitis suppurativa by excision and primary keystone flap for both sides in a single sitting without using any uncomfortable splints [Table/Fig-7,8]. The patient was advised to move his upper limb three days after surgery [Table/Fig-9]. The wound healed well within 7 d.
However, key stone flaps have minor drawbacks like long scars beyond the limits of the defect and its arc of rotation is limited unlike a free flap. It is important to make sure that the blood supply of the keystone flap has not been disrupted by either surgical ablation of cancer or by radiation therapy [7]. In spite of these, keystone flaps bring about primary wound healing for a wide variety of defects with minimal pain, a sensate cover and excellent cosmetic outcome. It has been used for defects in head and neck and parotid defects and defects over the trunk [2,8,9]. This technique can reduce the need to perform microsurgical flaps. Keystone flap requires shorter learning curve when compared to perforator flaps and micro vascular free flaps. This flap could be a useful tool of a Plastic surgeon.
Defect measuring 35 × 17 cm after excision of a recurrent soft tissue tumour over lateral aspect of thigh (Case 11)

Keystone flap done from the medial aspect of the thigh defect to cover it

Huge defect measuring 45 × 18cm over the posterior aspect of the right gluteal region and thigh after wide local excision of a recurrent soft tissue sarcoma (Case 10)
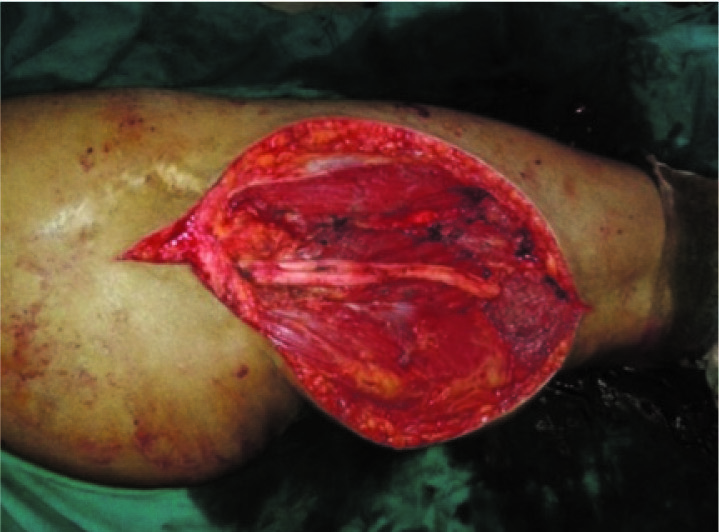
Bilateral keystone flap to cover the defect without any secondary donor area

Post abscess debridement defect in lateral aspect of thigh (Case 12),


Post excision hydradenitis suppurativa, left axilla (Case 5),

Post excision hydradenitis suppurativa, left axilla (Case 5)

| S. No. | Age | Size | Etiology | Site |
|---|
| 1 | 18 | 8 x 4 cm | Cutaneous malignancy | Ankle |
| 2 | 26 | 9.5 x 6 | Post abscess debridement | Knee |
| 3 | 45 | 9.5 x 5.5 | Tumour excision | Axilla |
| 4 | 38 | 18.5 x 12.5 | Post trauma | Thigh |
| 5 | 65 | 11 x 7 | Abscess (hidradenitis suppurativa) | Axilla |
| 6 | 34 | 6 x 9 | Post trauma | Fore arm |
| 7 | 28 | 8 x 4 | Post trauma | Elbow |
| 8 | 45 | 12 x 8 | Post trauma | Arm |
| 9 | 50 | 25 x 12 | Post trauma | Thigh |
| 10 | 40 | 45 x 18 | Tumour resection | Gluteal region |
| 11 | 52 | 35 x 17 | Tumour resection | Thigh |
| 12 | 18 | 10 x 8 | Post abscess debridement | Thigh |
| 13 | 24 | 14 x 8 | Post trauma | Gluteal region |
| 14 | 27 | 8 x 6 | Wound dehiscence | Leg |
| 15 | 38 | 8 x 6 | Post trauma | Knee |
| 16 | 46 | 8.5 x 4.5 | Post trauma | Arm |
| 17 | 60 | 12.5 x 6.5 | Post trauma | Thigh |
| 18 | 56 | 16.5 x 6.5 | Wound dehiscence | Leg |
| 19 | 41 | 12 x 8 | Post trauma | Knee |
| 20 | 24 | 9 x 5.5 | Tumour resection | Leg |
Conclusion
Keystone flap is an easy and safe option for covering various limb defects with least morbidity, provides a sensate cover and minimizes the need for microsurgical techniques and long operative time.
Acknowledgement
The authors are grateful to Dr.Satish Bhat, Senior consultant Plastic Surgeon, Yenepoya medical college, Mangalore, India for his guidance and inputs towards refining the technique of keystone flap.
[1]. FC Behan, The keystone design perforator island flap in Reconstructive surgeryANZ J surg 2003 73:112-20. [Google Scholar]
[2]. JS Khouri, BM Egeland, SD Daily, MS Harake, S Kwon, PC Neligan, The Keystone Island flap: Use in Large Defects of the Trunk and Extremities in Soft tissue ReconstructionPlastic & Reconstructive Surgery 2011 127(3):1212-21. [Google Scholar]
[3]. SP Bhat, Keystone flaps in coloured skin: Flap technology for the masses?Indian J Plast Surg 2013 46(1):36-47. [Google Scholar]
[4]. MD Moncrieff, JF Thompson, JR Stretch, Extended experience and modifications in the design and concepts of the keystone design island flapJ Plast Reconstr Aeshtet Surg 2010 63(8):1359-63. [Google Scholar]
[5]. P Pelissier, H Gardet, V Pinsolle, M Santoul, FC Behan, The keystone design perforator island flap. Part II: clinical applicationsJ Plast Reconstr Aesthet Surg 2007 60(8):888-91. [Google Scholar]
[6]. M Pignatti, M Pasqualini, M Governa, M Bruti, G Rigotti, Propeller flaps for leg reconstructionJ Plast Reconstr Aesthet Surg 2008 61(1):777-83. [Google Scholar]
[7]. HC Chen, Precautions in using keystone flapJ Plast Reconstr Aesthet Surg 2010 63:720 [Google Scholar]
[8]. FC Behan, WM Rozen, J Wilson, S Kapila, A Sizeland, MW Findlay, The cervico –submental island flap for locoregional head and neck reconstructionJ Plast Reconstr Aesthet Surg 2013 66(1):23-28. [Google Scholar]
[9]. FC Behan, CH Lo, A Sizeland, T Pham, M Findlay, Keystone Island Flap Reconstruction of Parotid DefectsPlast Reconstr Surg 2012 130(1):36e-41e. [Google Scholar]