Case Report
A 20-year-old female dental student reported to the department of Oral Medicine, Diagnosis and Radiology, KVG Dental College and Hospital, Sullia under Rajiv Gandhi University of Health Sciences, India for a detailed intraoral examination; as a private dental practitioner had detected a periapical lesion in her intraoral radiograph that was made for the diagnosis of proximal caries. Patient was asymptomatic during presentation. Her past medical and dental history was unremarkable.
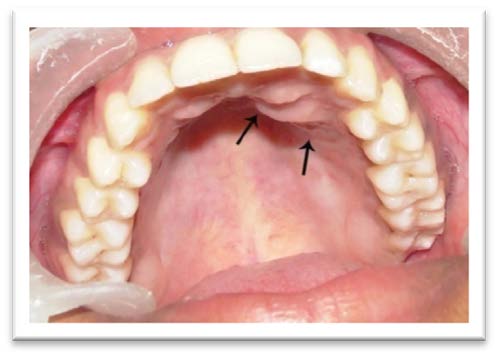
Detailed clinical examination revealed no visible facial swelling. On intraoral examination, an ill defined, solitary swelling of approximately 1x3 cms was observed in the left lateral part of the anterior hard palate in relation to the lateral incisor and canine [Table/Fig-1]. On palpation, it was non-tender and bony hard in consistency with no fluctuation or softening in any part of the swelling. History of trauma was negative. Maxillary anterior teeth were normal and responded positively to electric and thermal pulp vitality tests. This eliminated the possibility of periapical cyst (due to pulpal inflammation) or an odontogenic cyst to be the cause of the swelling. Hence, a preliminary diagnosis of an odontogenic tumour was made, Keratocy stic odontogenic tumour, Adenomatoid odontogenic tumour, Central odontogenic tumour, central hemangioma, Osteoporotic bone marrow defect, Neurofibroma and Neurilemmoma were the specific lesions considered in the differential diagnosis.
Anterior hard palate showing an ill defined swelling in the left lateral incisor – canine region
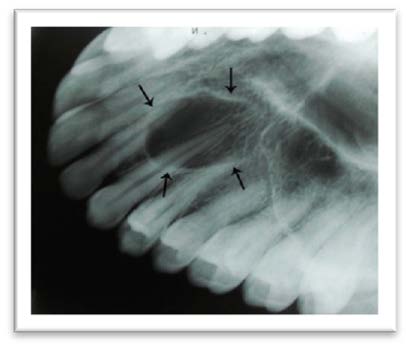
During Intraoral radiographic examinations, periapical radiograph of maxillary left canine region revealed an oval, well defined radiolucent lesion of approximately 2X3 mm with interrupted corticated border superimposing on the root apices of canine and first premolar [Table/Fig-2].
Intraoral periapical radiograph of maxillary left canine region revealing a well circumscribed, unilocular, oval radiolucent lesion with interrupted cortical margins superimposed over the root apices;

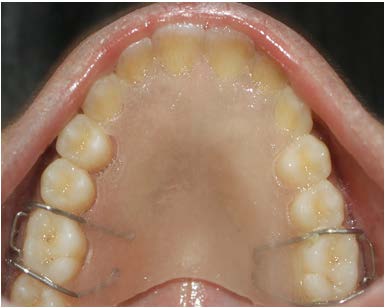
Maxillary lateral occlusal radiograph revealed a well-defined unilocular radiolucent lesion measuring approximately 2x3 mm overlapping the roots of the left lateral incisor, canine and first premolar. It was lined by irregular cortical margins [Table/Fig-3].
Maxillary occlusal radiograph demonstrating unilocular radiolucent lesion extending from left lateral incisor to first premolar; overlapping on their roots
Aspiration biopsy revealed no evidence of any cystic fluid or blood. Negative aspiration highlighted the possibilities of the lesion to be an odontogenic or nonodontogenic intraosseous tumour thus excluding cysts and hemangioma from the list of differential diagnosis. Adenomatoid odontogenic tumour, Central odontogenic tumour, Neurofibroma and Neurilemmoma were the odontogenic and non odontogenic tumours that were further considered in the differential diagnosis.
As a twofold intention of diagnosing and treating, the intraosseous lesion was subjected to surgical excision under local anaesthesia. Upon surgical exposure by reflecting the periosteal flap, the lesion was found to be well circumscribed and encapsulated within the dense fibrous connective tissue [Table/Fig-4]. The lesion thus could be easily separated from the surrounding healthy bone in toto. Following complete excision, the surgical defect was closed by open dressing and the specimen was subjected to histopathological examination. An acrylic removal partial denture (stent) was fabricated to cover the dressing area to prevent infection and facilitate wound healing [Table/Fig-5].
Surgical exposure revealing well encapsulated, unilocular lesion situated in the left lateral incisor- canine region

Anterior hard palate with acrylic splint fabricated following the surgical excision
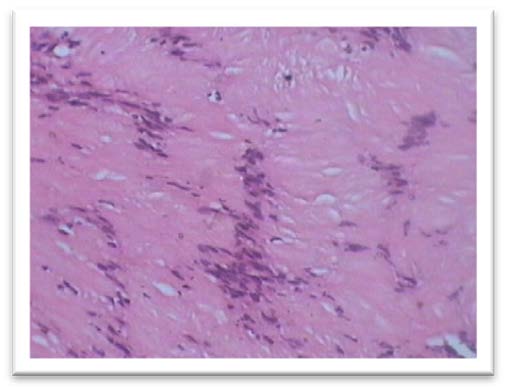
Microscopic examination of the specimen revealed that tumour mass was composed of neural tissue with cells being arranged in typical Antoni type A, seen towards right side exhibiting long spindle shaped nuclei arranged in parallel fashion giving a palisaded appearance forming a homogenous appearing Verocay bodies. While in other areas Antoni B type was haphazardly arranged with microcyst formation [Table/Fig-6]. Pallisaded arrangement of spindle shaped nuclei was well demonstrated in a high power view [Table/Fig-7]. No cellular atypia was evident. Large blood vessels with thrombus formation could be seen interspersed throughout the tumour mass.
Photomicrograph of the lesion showing Antoni B tissue
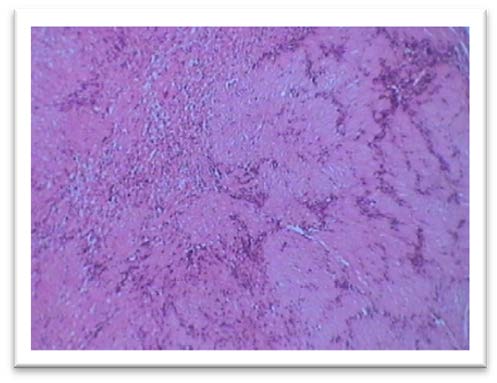
Photomicrograph of the lesion composed of densely cellular and irregularly arranged, elongated spindle cells with palisading nuclei and verocay bodies. Numerous blood vessels are seen interspersed throughout the tumour mass
On the basis of its classic histological features, the diagnosis of benign schwannoma was convincing. The nerve associated with the tumour could not be identified. Immunohistochemistry (IHC) was not required as the histological picture was clearly diagnostic of schwannoma.
Postoperative follow up after two months showed remarkable soft tissue healing [Table/Fig-8] though the underlying bone was soft and yielding because of the bony defect. Radiographic evaluation done two years postoperatively revealed complete bone regeneration by demonstration of internal trabeculations [Table/Fig-9]. There were no signs of recurrence. A general physical examination based on the diagnosis ruled out multiple tumours of neural origin in other sites.
Post operative clinical photograph of the palate showing healed areas

Two year-post operative maxillary occlusal radiograph demonstrating palate with normal trabecular pattern at the operated siteindicating complete bone remineralisation

Discussion
Schwannomas are rare, benign, encapsulated nerve sheath tumours of unknown aetiology. It is believed to originate from proliferation of Schwann cells in the perineurium of the peripheral, cranial or autonomic nerves, resulting in displacement and compression of the adjacent nerve [1,2]. Jose Verocay (in 1908) was the first to describe the microscopic features of this tumour under the term “Neurinoma”. Arthur Purdy Stout in 1935 further detailed on its histopathology and proposed the term “Neurilemmoma” [3]. Presently, the terms schwannoma, Schwann cell tumour, neurinoma, neurilemmoma and perineural fibroblastoma are being used synonymously [1,3].
Two types of schwannomas have been identified: a) Peripheral: located in the soft tissues and b) Central (intraosseous): located within the bone [4]. Being neural in origin, majority of the schwannomas are peripheral tumours; approximately 45% of them affecting the soft tissues of the head and neck [1,4]. Within the oral cavity, tongue is the commonest site followed by buccal mucosa, floor of the mouth, palate, lip and [5]. On the contrary, intraosseous (central) schwannomas are uncommon in head and neck area constituting less than 1%. Mandible is the most favoured site, the reason being attributed to the large caliber of the inferior alveolar nerve and its long course within the jaw [1]. They are presumed to involve bone by one of the three mechanisms: a) arising centrally within bone b) arising within the nutrient canal causing its enlargement c) arising from the periosteum and invading into the bone by secondary erosion [6,7].
Maxillary schwannomas are extremely rare. Over the last 70 y, only 13 cases of intraosseous schwannomas affecting the maxilla have been reported [1,8–19]. The clinical features of all those cases together with the current one has been summarized in the [Table/Fig-10].
Intraosseous Schwannomas of the Maxilla
| Sl. No. | Age/sex | Site/Region | Clinical Manifestations | Investigations carried out | Radiographic Appearance | Observations | Ref # |
|---|
| 1 | 18/F | alveolus /Incisor | Nontender upper lip swelling; vestibular obliteration, vital but mobile teeth | -Vitality test -Radiographs | Ill defined radiolucency; partial sclerotic margin; root resorption; alveolar crestal bone loss | Nonvital incisor at 6 mos post surgery | 8 |
| 2 | 11/F | Premolar | Swelling (6 mos) | NR | NR | | 9 |
| 3 | 21/M | Palate / molar | Incidental clinical finding; Nontender soft swelling with surface ulceration; | -Radiographs -FNAC -Incisional biopsy | Well defined unilocular radiolucency ; corticated margin; missing third molar; buccally displaced second molar | - Odontogenic Cyst (PD) - NAD at1yr post surgery | 10 |
| 4 | 64/F | Palate / Premolar-molar | Swelling (11 mos); mobile teeth; nonvital first molar | -Vitality test -Radiographs -FNAC -Incisional biopsy | Ill defined periapical radiolucency; partial sclerotic margin; | -IHC for S100 protein & neuron specific enolase -NAD at 1yr post surgery | 11 |
| 5 | 9/M | Alveolus /Central incisor | Swelling (10 mos) | -Radiographs | Ill defined periapical radiolucency; alveolar crestal bone loss | - IHC for S100 protein - NAD at 6yrs post surgery | 12 |
| 6 | 14/F | Incisors | Incidental radiographic finding | -Vitality test -Radiographs | Well defined periapical radiolucency | Bone regeneration at 1yr post surgery | 13 |
| 7 | 40/M | Hard palate | Dysphagia, garbled speech; smooth & firm swelling (3mos) | -CT | Nonenhancing soft tissue mass without bony erosion / sinus involvement | - IHC for S100 protein | 14 |
| 8 | 25/M | Gingiva / premolar | Smooth, firm swelling (9yrs) | Incisional biopsy | NR | Fibromatosis gingivae (PD) | 15 |
| 9 | 44/F | Alveolus /lateral incisor to premolar | Swelling (20 yrs) | Incisional biopsy | NR | -minor salivary gland tumour (PD) - NAD at 4yrs post surgery | 1 |
| 10 | 15/ NR | Hard palate/ premolar | Firm, mobile swelling (3mos) | -CT -Incisional biopsy | Well defined, homogenous low density mass without surrounding tissue infiltration | - IHC for S100 protein - NAD at 1yr post surgery | 16 |
| 11 | 64/F | Hard palate / Incisor | Smooth, firm , oval swelling (3yrs) | -Radiographs | Well defined radiolucency; sclerotic lining | Palatal cyst (PD) | 17 |
| 12 | 10/M | hard palate / molar | Dysphagia; smooth, firm, well encapsulated growth (5mos) | NR | NR | NR | 18 |
| 13 | 12/F | Hard and soft palate | Ulcerated growth from hard palate to uvula with yellowish - purple surface discolouration | Incisional biopsy | NR | - IHC for S100 protein | 19 |
| 14 | 20/F (Present case) | Hard palate / canine | Incidental radiographic finding; smooth, firm swelling; | -Radiographs -FNAC | Well defined radiolucency; partial sclerotic margin | - Odontogenic cyst (PD) - complete bone regeneration at 2yrs post surgery | |
mos: months; NR: Not Reported; FNAC: Fine Needle Aspiration Cytology; PD: Provisional Diagnosis; NAD: No Abnormality Detected; IHC: Immunohistochemistry; CT: Computed Tomography
Patients with schwannomas showed a median age of 20 y and 6 mnth (range, 9-64 y), with a peak prevalence in second decade of life. Data pertaining to the gender revealed a slight female predilection with a ratio of 1.6:1. Regarding the site of affectation, the tumours showed slightly increased predilection for the hard palate [Table/Fig-10].
Analysis of the symptomatology revealed that swelling was the most common complaint of the patients during their initial visit. However, the tumour was discovered incidentally during their radiographic evaluation [13] or clinical examination [10] [Table/Fig-10]. The duration of the swelling ranged from three mnth to 20 y. Other symptoms like dysphagia and garbled speech were reported by two patients [14,18]. Patients never gave a history of pain or paresthesia. During the clinical examination, eight of the 14 schwannomas produced clinically visible swellings with one of them presenting as alveolar ridge expansion. Surface ulceration [10,19] and tooth mobility [8,11] was observed in two patients. Literature suggested that Provisional (objective) diagnosis was rarely done after the clinical examination. If and when made, it was often diagnosed as cyst [10,17] or fibromatosis gingivae [15].
Radiographic investigations including CT [14,16] have been carried out in most of the cases. In addition, FNAC [10,11] and vitality test [8,11,13] had also been performed. Only in six of the 14 cases, Schwannoma was diagnosed prior to surgical excision by histopathology following incisional biopsy [1,10,11,15,16,19]. IHC for S100 protein was performed in only five cases [Table/Fig-10].
Radiographs demonstrated neoplastic bone destruction in the form of radiolucent lesions surrounded by thin, sclerotic margin. In few cases, margins were ill defined; associated alveolar bone resorption [8,12] and root resorption [8] was observed. In CT, the tumour presented as a well defined, non enhancing, low density soft tissue mass without soft tissue infiltration [14,16] [Table/Fig-10].
Based on our review of the literature, maxillary schwannomas have equal predilection for anterior and posterior segments of the jaw unlike their mandibular counterparts that have greater affliction to the posterior body – ramus. Similar to mandibular schwannomas, maxillary ones have a definite female predilection. Maxillary schwannomas affect younger individuals; often in the second decade of life whereas mandibular tumours are common in older age group.
The clinical features are unremarkable. Unlike peripheral (soft tissue) tumours where patients report with pain [2], long standing swelling is the most frequent complaint reported by the patients of intraosseous schwannomas; pain and paresthesia are rare. Nerve paralysis may develop if the gradually increasing tumour compresses the maternal nerve fibres passing over its capsule [20]. Large palatal schwannomas may exhibit surface ulcerations [10,19]. Associated teeth remain vital inspite of alveolar bone resorption.
Cyst like clinical presentation of maxillary schwannomas as asymptomatic swelling can easily be misdiagnosed as an odontogenic cyst [10,17]. In majority of the cases, diagnosis has been done subsequent to the excision of the tumour mass [8,12–14,17].
Investigations such as FNAC aids in excluding odontigenic cysts. Nevertheless, large tumours necessitate advanced imaging modalities like CT and MRI [14,16]. Being non specific, they only help in assessing the margins of the tumour and its infiltration into the surrounding structures.
Radiographically, mandibular schwannomas exhibit well defined unilocular/multilocular radiolucency with a thin sclerotic border [21]. In all the cases reviewed by us, maxillary schwannomas presented as unilocular radiolucent lesions, often in close proximity to the root apices. Most of them were surrounded by a thin, sclerotic margin. Resorption of the adjacent roots and dystrophic calcifications are likely [2,8]. A definitive diagnosis is difficult to make solely on the basis of clinical presentation and radiographic examination; a biopsy is usually necessary.
Characteristic Histopathological features of schwannoma include encapsulation and presence of Antoni type A and Antoni type B tissues. Antoni A are well differentiated cells with nuclear palisading and Verocay bodies. Antoni B tissue, the predominant tissue type in central schwannomas is comprised of poorly organized cells with prominent, thickened blood vessels [2]. Histopathological features of schwannoma are conclusive. Hence, IHC if and when performed is only for academic completion. In IHC, Antoni type B tissue cells show intense staining for S-100 protein. Perineural cell derived tumour capsule are immunoreactive to EMA (Epithelial Membrane Antigen) and collagen IV. Capsular and Antoni B cells are positive for CD34 and CD68 lysosome associated antigens also. But, S-100 protein is probably the single best antigen for confirmation of this neural tumour as it is expressed exclusively by Schwann cells [17].
Either maxilla or mandible, surgical enucleation has remained the mainstay of treatment for schwannomas. Patients have remained asymptomatic with no clinical evidence of disease in a follow up examination of cases over a period of two to six y [12,16]. The presence of capsule possibly will facilitate its complete removal, reducing the rate of recurrence. Bone regeneration is noticeable as early as one year following surgery [13].
In the current case, the tumour presented as a well defined radiolucent lesion superimposing over the roots of the anterior teeth that was incidentally discovered during the radiographic examination. Comparable to a periapical lesion, it would have been mistaken for pathology of odontogenic origin but for the presence of vital teeth. Meticulous clinical examination revealed a palatal swelling that was negligibly small as compared to the size of the radiographic bone resorption. This would have gone unnoticed until grown to larger dimensions. Being situated in the vicinity of odontogenic apparatus, a clinician would primarily consider odontogenic cysts and tumours in the list of their differential diagnosis. Further, results of vitality test and FNAC assisted in inclusion of non odontogenic lesions. Author wish to highlight the role played by the chairside investigations in the diagnosis of this case; emphasising the need for performing such simple tests that furnish instant results and improves diagnosis. Intraosseous schwannoma affecting the maxilla is rare; manifesting as periapical radiolucency is rarer hence likely to receive back seat in the diagnostic chart. Yet, our literature search revealed two of the 13 reported cases of central schwannomas presenting as periapical lesions. This substantiates that whenever an oral physician encounters a painless maxillary swelling with a lesion in the periapical region of vital teeth, non odontogenic lesions should be borne in mind; furthermore intraosseous schwannoma must be considered in their list of diagnosis.
Conclusion
Intraosseous lesions located in the periapical region with nonspecific clinical and radiographic features often lead to diagnostic confusion. Most of the lesions located in the vicinity of the teeth are odontogenic in origin. Yet, other possibilities like intraosseous schwannomas must be included in the differential diagnosis, especially when the clinical and radiographic presentations are inconclusive.
mos: months; NR: Not Reported; FNAC: Fine Needle Aspiration Cytology; PD: Provisional Diagnosis; NAD: No Abnormality Detected; IHC: Immunohistochemistry; CT: Computed Tomography
[1]. Martins MD, de Jesus LA, Fernandes KPS, Bussadori SK, Taghloubi SA, Martins MAT, Intra-oral schwannoma: Case report and literature reviewIndian J Dent Res 2009 20:121-25. [Google Scholar]
[2]. Nevilli BW, Damm DD, Allen CM, Bouquot JE, Oral & Maxillofacial Pathology 2009 3rd EdPhiladelphiaWB Saunders Company:526-28.Chapter:12: Soft tissue tumours [Google Scholar]
[3]. Chi CA, Carey J, Muller S, Intraosseousschwannoma of the mandible: A case report and review of literatureOral Surg Oral Med Oral Pathol Oral RadiolEndod 2003 96:54-65. [Google Scholar]
[4]. Friedman M, Intraosseous schwannomaOral Surg Oral Med Oral Pathol 1964 18:90-96. [Google Scholar]
[5]. Martins MD, Taghloubi SA, Bussadori SK, Fernandes KPS, Paolo RM, Martins MAT, Intraosseous schwannoma mimicking a periapical lesion on the adjacent tooth: case reportIntendod J 2007 40:72-78. [Google Scholar]
[6]. Musgrove BT, Moody GH, Central neurilemmoma of the mandibleBr Dent J 1990 169:206-07. [Google Scholar]
[7]. Ellis GL, Abrams AM, Melrose RJ, Intraosseous benign neural sheath neoplasms of the jaws. Report of seven new cases and review of the literatureOral Surg Oral Med Oral Pathol 1977 44:731-43. [Google Scholar]
[8]. Ord RA, Rennie JS, Central Neurilemmoma of the maxilla. Report of a case and review of the literatureInt J Oral Surg 1981 10:137-39. [Google Scholar]
[9]. Takeda Y, Neurilemmoma of the maxillary alveolar bone: report of a caseBr J Oral Maxillofac Surg 1991 29:208-10. [Google Scholar]
[10]. Minic AJ, Central schwannoma of the maxillaJ Oral Maxillofac Surg 1992 21:297-98. [Google Scholar]
[11]. Villanueva J, Gigoux C, Sole F, Central neurilemmoma of maxillaOral Surg Oral Med Oral Pathol Oral Radiol Endod 1995 79:41-43. [Google Scholar]
[12]. Amir R, Altman KW, Zaheer S, Neurilemmoma of the herd palateJ Oral Maxillofac Surg 2002 60:1069-71. [Google Scholar]
[13]. Pandarakalam C, Sudha S, Shameena PM, Varghese VI, An unusual presentation of a case of schwannomaJ Oral MaxillofacPathol [serial online] 2005 [cited 2012 Mar 27] 9:27-9.Available from: http://www.jomfp.in/text.asp?2005/9/1/27/39057 [Google Scholar]
[14]. Lopez-Carriches C, Baca-Perez-Bryan R, Montalvo-Montero S, Schwannoma located in the palate: Clinical case and literature reviewMed Oral Patol Oral cirBucal 2009 14(9):e465-68. [Google Scholar]
[15]. Parikh NR, Desai N, Intraoral schwannoma (neurilemmoma): An unusual anterior palatal swelling – A Case reportJ. Int Oral Health 2010 2(4):87-91. [Google Scholar]
[16]. Dhupar A, Yadav S, Dhupar V, Schwannoma Of The Hard Palate: A Rare CaseThe Internet Journal of Head and Neck Surgery 2011 4(2) [Google Scholar]
[17]. Rahpeyma A, Jafarian AH, Ahmadi SK, Sarabadani J, A Schwannoma of the soft palate in a child: Histological and Immunohistochemical Features and Surgical MethodIranian Journal of Otorhinolayngology 2012 24(2):95-99. [Google Scholar]
[18]. Artzi Z, Taicher S, Nass D, Neurilemmoma of the mental nerveJ Oral Maxillofac Surg 1991 49:196-200. [Google Scholar]
[19]. Metwaly H, Maruyama S, Cheng J, Hoshina H, Takagi R, Hayashi T, Central Schwannoma of the mandible:report of a case and review of the literatureOral Med Pathol 2010 15:29-33. [Google Scholar]
[20]. Kim SH, Kim NH, Kim KR, Lee JH, Choi HS, Schwannoma in Head and Neck: Preoperative Imaging Study and IntracapsularEnucleation for Functional Nerve PreservationYonsei Med J 2010 51(6):938-42. [Google Scholar]
[21]. Chi CA, Carey J, Muller S, Intraosseousschwannoma of the mandible: A case report and review of literatureOral Surg Oral Med Oral Pathol Oral Radiol Endod 2003 96:54-65. [Google Scholar]