Thrombocytopenia with Unilateral Dysplastic Radius- Is it Thrombocytopenia - Absent Radius (TAR) Syndrome?
Mani Kant Kumar1, Indradeo Prasad Chaudhary2, Ram Bilas Ranjan3, Prashant Kumar4
1 Associate Professor, Department of Pediatrics, Narayan Medical College & Hospital, Jamuhar, Sasaram, District-Rohtas, Bihar, India.
2 Professor, Department of Pediatrics, Narayan Medical College & Hospital, Jamuhar, Sasaram, District-Rohtas, Bihar, India.
3 Assistant Professor, Department of Pediatrics, Narayan Medical College & Hospital, Jamuhar, Sasaram, District-Rohtas, Bihar, India.
4 Assistant Professor, Department of Pediatrics, Narayan Medical College & Hospital, Jamuhar, Sasaram, District-Rohtas, Bihar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr Mani Kant Kumar, Associate Professor, Department of Pediatrics, Narayan Medical College and Hospital, Jamuhar, Sasaram, Dist- Rohtas, Bihar-821305, India.
E-mail: manikant7@yahoo.com
Thrombocytopenia - absent radii (TAR) syndrome is an autosomal recessive genetic rare disorder with hypomegakaryocytic thrombocytopenia and bilateral absent radius that may have additional anomalies. This disorder is characterized by thrombocytopenia resulting in potentially severe bleeding episodes primarily during infancy. We report the case of a 7-day-old term appropriate for gestational age (AGA) male baby, product of non consanguineous marriage presented with bloody loose stool, right sided upper limb deformity and paleness of the body, was diagnosed as TAR syndrome with some atypical presentation. Such type of atypical presentation has not been previously reported in a case with TAR Syndrome.Patient was managed in our hospital with packed cell transfusion and two units platelets concentrates transfusion, Intra-venous antimicrobials, and other supportive treatment. He gradually improved and was discharged after seven days of hospital stay with advice to consult orthopedic surgeon for opinion regarding limb reconstruction.
Absent unilateral radius, Atypical presentation, Thrombocytopenia
Case Report
A 7-day-old term baby boy was the first child, a product of a non-consanguineous marriage. The pregnancy was uneventful without any history of maternal illness, fever or rash. The baby was delivered by normal spontaneous vaginal delivery in government hospital. On 3rd day of life, baby developed bloody stool, 8 times per day. Parents consulted paediatrician in a private nursing home, where he was treated with intravenous antimicrobials, vitamin K, probiotics without any significant improvement. On 7th day of life, baby was brought to our hospital in emergency with complain of malformed right upper extremity, bloody loose stool for past 4 days, small pin point reddish spot over chest and buttock, Progressively increasing paleness of the whole body. Physical examination at presentation revealed a baby with stable vital signs who was alert, pale and active, with a length of 49 cm, a weight of 2,750 g, and a head circumference of 34 cm (all on the 50th percentile). He had severe palor and purpuric rash over chest. He had short and deformed right forearm and radial deviation of right upper limbs with rudimentary thumb without metacarpal [Table/Fig-1]. Systemic examination was unremarkable.
Photograph of the baby showing short right forearm with absent radius and radial deviation of hand, purpuric rash over chest (Black arrow)

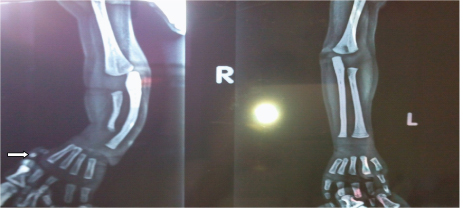
Initial laboratory investigations gave the following results: complete blood count: hemoglobin, 7 g/dL; corrected reticulocytic count, 3 %; total leukocytes count (TLC): 12600/uL, differential count revealed 55% neutrophils, 38% lymphocytes, 5% band cells (Immature neutrophils), eosinophil and monocytes 1% each, platelet count, 18,000/uL; Coagulation profile - prothrombin time, 14 sec (control 13 sec); partial thromboplastin time, 30 sec (control 30). Liver function test had the following results: total serum bilirubin 7.5 mg/dL; Indirect serum bilirubin 7.1 mg/dL (direct), 0.4 mg/dL; and serum glutamic pyruvic transaminase (SGPT) 28 U/L. Serum Electrolytes, Serum C reactive protein (CRP) and kidney function were within normal limits. TORCH screens were normal. Bone marrow aspiration cytology was not done because parents did not given consent for bone marrow aspiration cytology. Skiagram of the forearm showed dysplastic radius, curved ulna and absent first metacarpal bone of right hand and only two dysplastic phalangeal bone (white arrow) of right thumb [Table/Fig-2]. Ultrasongraphic study of his abdomen and brain were normal. On the basis of clinical presentation, physical findings, isolated thrombocytopenia, and X-ray results, the diagnosis of TAR syndrome with atypical presentation was made. Patient was managed in our hospital with packed cell transfusion at rate of 10 ml /kg two times on alternate day and two units platelets concentrates transfusion, Intra-venous antimicrobials, and other supportive treatment. He gradually improved and on day 3 of admission became asymptomatic and discharged after seven days of hospital stay with advice to consult orthopedic surgeon for opinion regarding limb reconstruction and echocardiogram to rule congenital heart disease. In follow up for past one month, he had gained weight 1kg, without any new bloody diarrhoeal episode, bleeding manifestation and his echocardiogram was normal.
Skiagram of the both forearm showing dysplastic radius, curved ulna and absent first metacarpal bone of right hand and only two dysplastic phalangeal bone (white arrow) of right thumb
Discussion
We reported a case with bleeding manifestation due isolated thrombocytopenia and unilateral dysplastic radius, was diagnosed as Atypical TAR syndrome. Atypical TAR syndrome because unilateral dysplastic radius in association with isolated thrombocytopenia, not reported so far in world literature. TAR syndrome is an autosomal recessive inherited disorder characterized by bleeding manifestation due to isolated thrombocytopenia and bilateral absent radius. Thrombocytopenia, which may be transient, but present in 100% of cases diagnosed with TAR syndrome [1]. TAR syndrome without thrombocytopenia does not exist, but the platelet count varies from case to case. In earlier study, researchers found that patients with TAR syndrome are usually diagnosed at birth, due to thrombocytopenia as they present with petechial rash or bleeding manifestation like bloody diarrhea in the first week of life or later during the next four months. Platelet counts at birth are usually 15,000 to 30,000/uL [2,3]. Present case also presented on third day of life with bloody diarrhea and petachial rash platelets count was 18000/μL. In our case we have ruled out other possible cause of thrombocytopenia like sepsis, intrauterine TORCH group infection. The exact pathophysiology of the thrombocytopenia is still unclear, but it may be explained by the following different mechanisms: (1) the absence of humoral or cellular stimulators of megakaryocytopoiesis (2), the absence of megakaryocytic progenitor cells (3), cellular defects in megakaryocytic precursors (for example, receptor defects) or (4) the presence of humoral or cellular inhibitors of megakaryocytopoiesis [2]. In our case bone marrow aspiration cytology was not done because parents did not given consent for bone marrow aspiration cytology.
Other characteristic feature of TAR Syndrome is bilateral absence of radii. In contrast to this, our case demonstrated only unilateral dysplasia of radius and radial deviation of the right forearm. Other upper limb anomalies (aplasion and hypoplasion of ulna and humerus, hypoplasion of carpal bones, sindactylia, clinodactylia are rare [1,4]. None of the above lower limb anomalies were not present in our case. However, the frequency of appearance of the lower limb anomalies (hips dysplasia, femoral and tibial torsion, pes equinovarus and equinovalgus and knee deformations) may be present in 47% [2]. Most close differential diagnosis is Radial club Hand, which is characterized by complete absent of radius to dysplastic radius, but not presented with bleeding manifestation, thrombocytopenia and presence of the thumb [5]. In present case thumb was present but in rudimentary form that was hanging without metacarpal bone.
Congenital heart anomalies (Tetralogy of Fallot, atrial and ventricular septum anomalies) appeared in 22-33 % of the cases [1,2], but none of the above congenital heart disorder were present in the present case. All changes of limbs and other organs of TAR syndrome that were here described can be present at the syndromes and other diseases (Holt-Oram syndrome, Fanconi anemia, VACTERLS Association, Cornelia de Lange syndrome: embriopathy due to thalidomide etc.), which may be considered with the differential diagnosis with TAR syndrome [5,6].
The most frequent cause of mortality among children with TAR syndrome was bleeding. The rate of mortality depends on the platelet count and other accompanied anomalies. The most frequent cause of death was due to the intracranial bleeding, especially during the first two years of life [4,7].
Conclusion
TAR syndrome is a rare genetic disorder characterized by low platelet level and radial aplasia. In this case report we present a baby boy with thrombocytopenia, bleeding manifestation, unilateral dysplastic radius and rudimentary thumb. Although we have diagnosed this case as Atypical TAR syndrome, but still there is a big question that, is it Atypical TAR Syndrome or a new syndrome?
[1]. Hall JG, Levin J, Kuhn JP, Thrombocytopenia with absent radius (TAR)Medicine (Baltimore) 1969 48(6):411-39. [Google Scholar]
[2]. Greenhalgh KL, Howell RT, Bottani A, Ancliff PJ, Brunner HG, Verschuuren-Bemelmans CC, Thrombocytopenia absent radius syndrome: a clinical genetic studyJ Med Genet 2002 39:876-81. [Google Scholar]
[3]. Omran Ahmad, Sahmoud Shaimaa, Peng Jing, Ashhab Usman, Yin Fei, Thrombocytopenia and absent radii (TAR) syndrome associated with bilateral congenital cataract: a case reportJournal of Medical Case Reports 2012 6:168 [Google Scholar]
[4]. Hedberg VA, Lipton JM, Thrombocytopenia absent radii. A review of 10 casesAm J Pediatr Hematol/Oncol 1988 10:51-64. [Google Scholar]
[5]. Kumar MK, Suman SK, Radial club hand: A Neglected caseJournal of Clinical and Diagnostic Research 2011 5:1458-60. [Google Scholar]
[6]. Ahmad R, Pope S, Association of Mayer-Rokantinsky, Kuster-Hauser. Syndrome with Thrombocytopenia Absent Radii syndrome: a rare presentationEur J Obstet Gynecol Reprod Biol 2008 :257-58. [Google Scholar]
[7]. Tangsong T, Sirichottyakul S, Chanprapaph P, Prenatal diagnosis of thrombocytopenia - absent radius (TAR) syndromeUltrasound Obstet Gynecol 2000 15:256-58. [Google Scholar]