Introduction: Symptomatic vaginal discharge is the most frequent symptom in women of reproductive age group. Owing to social stigma majority of affected women hesitate to seek medical consultation. Therefore the actual incidence of vaginal discharge is much more than what is reported. The aim of the study is to determine the microbiological profile of symptomatic vaginal discharge in rural area and its utility in the management of genital tract infection.
Materials and Methods: This was a descriptive type of observational study, conducted in sexually active women of reproductive age group (18-45 years) attending the OPD/IPD of Obstetrics and Gynaecology Department of National Institute of Medical Sciences, Shobhanagar, Jaipur (Rajasthan), over a period of 18 months from June 2012 to December 2013. Hundred sexually active non pregnant women of reproductive age group (18-45 years) were included in the study. After taking consent general physical examination along with pelvic examination was performed. Two high vaginal swabs and blood sample were collected for various tests. Hanging drop preparation was immediately made. This was followed by gram staining and culture. Chlamydia trachomatis IgM antibody was detected by ELISA method.
Results: Out of 100 women with symptomatic vaginal discharge, specific diagnosis was obtained in 89% of cases whereas no specific aetiology was found in 11% cases. Mean age was 32.60 years. Fifty-three percent patient had Bacterial vaginosis, candidiasis was found in 14% cases, 16% had Chlamydia trachomatis infection while Trichomonas vaginalis infection was detected in 6% cases. Homogenous discharge was most prevalent (52%), followed by mucopurulant discharge in 23% of women.
Conclusion: Patient with symptomatic vaginal discharge need to be actively managed with appropriate antimicrobial agents. Judicious management may be helpful in prevention of HIV, HPV, CIN and post infection sequelae.
Bacterial vaginosis, Chlamydia trachomatis infection, Trichomoniasis, Vulvovaginal candidiasis
Introduction
Symptomatic vaginal discharge in the women of reproductive age group is responsible for 5-10 million OPD visits per year throughout the world [1]. Abnormal vaginal discharge also predisposes to significant morbidity in the form of pelvic inflammatory diseases, infertility, endometriosis, cuff cellulitis, urethral syndrome, pregnancy loss, preterm labour, increase susceptibility to sexually transmitted infections (STI), including HIV and to be associated with low birth weight and preterm birth [2]. The prevalence of vaginal discharge in India is estimated to be 30% [1]. Most common cause of symptomatic vaginal discharge is Bacterial vaginosis (33%-47%), followed by candidiasis (20%-40%) and trichomoniasis (8%-10%). These three conditions account for 90% of all etiologies of abnormal vaginal discharge. Multiple infections can also coexist [3]. The normal vaginal flora often includes hemolytic Streptococci, anaerobic Streptococci (Pepto Streptococci), Bacteroids species, Clostridia, Gardnerella vaginalis, Ureaplasma urealyticum and sometimes Listeria or Mobiluncus species but the cervical canal and fallopian tubes are sterile [4]. The aim of the study is to determine the microbiological profile of symptomatic vaginal discharge in rural area and its utility in the management of genital tract infection.
Materials and Methods
This was a descriptive type of observational study, conducted in sexually active women of reproductive age group (18-45 years) Gupta3attending the OPD/IPD of Obstetrics and Gynaecology Department of National Institute of Medical Sciences, Shobhanagar, Jaipur (Rajasthan), over a period of eighteen months from June 2012 to December 2013. Hundred sexually active non pregnant women of reproductive age group (18-45 years) included in the study. Pregnant women, post menopausal, menstruating women, those who had received antimicrobial/antifungal in the previous one month, patient who had delivered or aborted six weeks prior were excluded from the study.
Written informed consent was taken and proper counselling done. Information was collected in relation to the patient’s socioeconomic status, sexual behaviour, medical & surgical history, followed by physical examination with sample collection. General physical examination followed by pelvic examination including a per speculum and a bimanual examination conducted. All the relevant information was recorded on pretested proforma regarding socioeconomic status, Literacy, hygiene and associated symptoms and the clinical examination done and the different varieties of vaginal samples were collected. Blood sample obtained for various tests.
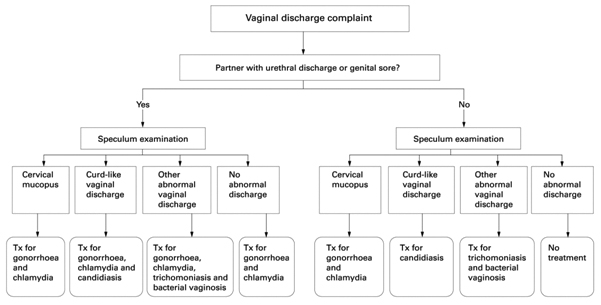
The pH was measured using litmus papers ranging from 2 to 10. Wet mount preparation/Hanging drop preparation was made and examined under microscope immediately for the presence of Trichomonas vaginalis. The first swab taken and smears were made on a clean and grease free glass slide, then heat fixed by just passing the glass slide over the flame. Then the smear was stained by Gram’s method and observed under oil immersion objective and assessed using the Nugent’s score for diagnosis of Bacterial vaginosis and the presence gram positive oval yeast like budding cells (2-4μm) and/or pseudohyphae [5] [Table/Fig-1]. The second swab taken and all samples immediately transported to microbiology laboratory for culture and sensitivity. Two millilitre blood was collected in plain vial under all aseptic precautions and refrigerated at 2-80C for detecting Chlamydia trachomatis IgM antibody. After collecting all the required samples, treatment given as recommended by the National AIDS Control Organization (NACO) for the management of vaginal discharge [6] [Table/Fig-2]. The data was analyzed using Software for statistical calculations: Medcalc 14.0.0 version.
Results
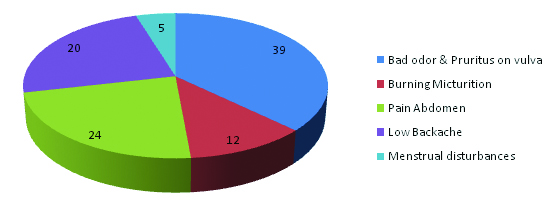
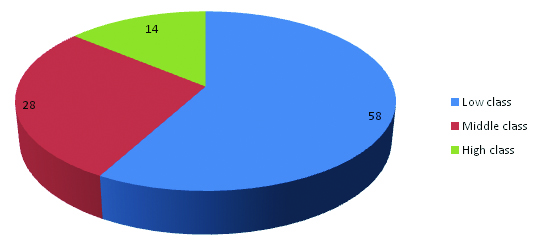
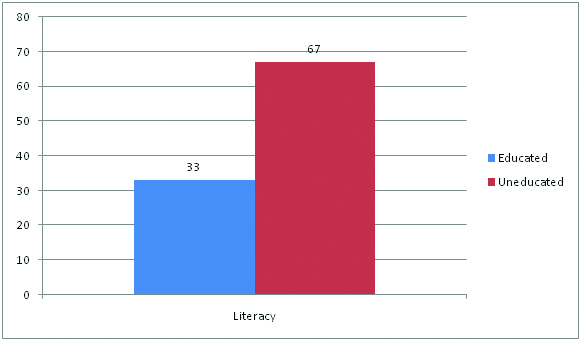
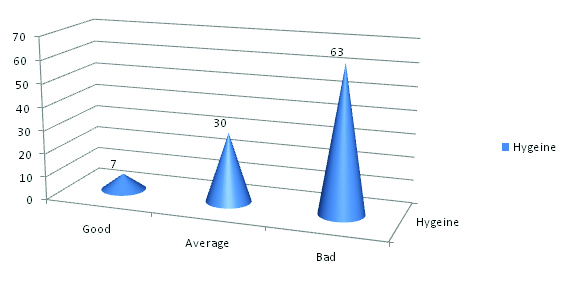
Out of 100 women with symptomatic vaginal discharge, specific diagnosis was obtained in 89% of cases whereas no specific aetiology detected in 11% cases [Table/Fig-3]. Majority (46%) patients belong to age group of 21-30 years while 25% cases were in age group of 31-40 years and 20% between 41-50 years. Bacterial vaginosis, Trichomonas vaginalis and Chlamydia trachomatis infection was common in women between the age groups 21-30 years accounting for 77% of cases while candidiasis was seen in women between age group 31-40 years. The association of age with the vaginal infections was not statistically significant (p >0.5). Majority of women (44%) complained of symptoms more than one year while (24%) patient had duration of disease between four and six months. Most of the women presented with homogenous discharge (52%) [Table/Fig-3]. Trichomonas vaginalis detected in 6% cases while clue cells were detected in 44% cases and 20% cases showed pus cells [Table/Fig-4,5,6]. The commonest symptom was malodorous discharge and pruritus in 27% cases [Table/Fig-7]. In Bacterial vaginosis and Chlamydia trachomatis infection homogenous discharge was most prevalent. 58% & 28% patients belongs to low and medium socioeconomic status respectively [Table/Fig-8], 67% cases were uneducated [Table/Fig-9] and 63% patient had bad hygiene [Table/Fig-10].
Discussion
The presence of lower genital tract infection poses a great threat to the health of women. Reproductive tract infections are one of the most serious public health issues in both developed and developing countries. Around 150,000,000 cases of reproductive tract infections in Southeast Asia [7].
Epidemiological studies have been limited by the use of variable case definitions and diagnostic methods among heterogeneous populations. In our study 100 cases were studied. Mean age was 32.60 years. Maximum cases of symptomatic vaginal discharge were observed between 21 and 30 year of age (46%). Similar peak age incidence (15-30 years 82.8%) is noted in other studies done by Rekha et al., Singh et al., and Madhivanan et al., [1,8,9]. Out of 100 cases homogenous discharge was most prevalent (52%), followed by mucopurulant discharge in 23% of women. Symptomwise 39% of women presented with malodorous vaginal discharge, other symptoms were burning micturition (12%), pain in abdomen (24%), low backache (20%) and dyspareunia (5%). Majority of women (44%) complained of symptoms for more than one year while (33%) between one and six months. Other studies also show similar results as ours for discharge and symptoms [1,3].
Bacterial vaginosis has yet to be shown as an independent risk factor for pelvic inflammatory disease, infertility and miscarriages in the absence of sexually transmitted infections [10].
The presence of Bacterial vaginosis increase susceptibility to human papilloma virus (HIV) infection [11,12]. Trichomonas vaginalis may play a critical and under recognized role in amplifying HIV transmission [12]. This study showed that by using microbiological methods we can prevent the susceptibility to HIV, HPV, CIN and many more adverse squeal of vaginal infections caused by various organisms.
Microbiological methods revealed that staphylococcus aureus was most prevalent and was found in 20% of total 100 patients. This was followed by Chlamydia IgM positive in 16% patients. These findings correlate with study done previously in south India (staphylococci in 30% cases of Bacterial vaginosis) and Lybia (28% staph aureus) [13]. Similarly Doddaiah et al., found 17.7% Candida and Mohanty et al., reported 18.5% Candida species infection in their study on vaginal discharge [14,15]. Chlamydia trachomatis was detected in 23.0 per cent of patients attending gynaecology OPD and among 19.9 per cent patients attending STD clinic in a study from New Delhi [16].
WHO recommends that all women complaining of abnormal vaginal discharge be treated empirically with metronidazole and when Candida noted, to treat for candidiasis as well. This study shows if blanket treatment was advocated to all the women complaining of abnormal vaginal discharge, most of the women would receive unnecessary antibiotic and antifungal therapy. Over diagnosis and unnecessary use of antibiotics and antifungal treatment not only have financial consequences for the health system but also carries the risk of possible social consequences in the community [17].
Oral metronidazole is associated with anorexia, nausea, vomiting and skin rashes. It crosses the blood brain barrier and may cause dizziness, convulsion and peripheral neuropathy .Antifungal therapy is associated with renal and hepatic complications, hypersensitivity reactions, nausea and vomiting, flatulence and rarely angioedema. FDA condemns blanket therapy and combination therapy for treatment of vaginal infections without proof of infections [6].
The nugent scoring system for diagnosis of Bacterial vaginosis
| Score | Lactobacillus morphotype per field | Gardnerella morphotype per field | Curved bacteria (mobiluncus) per field |
|---|
| 0 | >30 | 0 | 0 |
| 1 | 5-30 | <1 | 1-5 |
| 2 | 1-4 | 1-4 | >5 |
| 3 | <1 | 5-30 | 5-30 |
| 4 | 0 | >30 | >30 |
Algorithm recommended by the National AIDS Control Organisation (NACO) [6] or the management of vaginal discharge
Distribution of cases according to type of discharge (n=100)
| Discharge | No. | % |
|---|
| Homogenous | 52 | 52.00 |
| Curdy White | 17 | 17.00 |
| Muco-Purulent | 23 | 23.00 |
| Yellowish Green | 8 | 08.00 |
| Total | 100 | 100.00 |
Reproductive tract infection causing vaginal discharge according to organism
| Microbiological Diagnosis | No. | % |
|---|
| Bacterial vaginosis | 53 | 53.00 |
| Candida | 14 | 14.00 |
| Chlamydia trachomatis | 16 | 16.00 |
| Trichomonas vaginalis | 6 | 06.00 |
| Etiology not found | 11 | 11.00 |
| Total | 100 | 100.00 |
Various aetiological agents isolated from vaginal discharge
| Microbiological Diagnosis | No. | % |
|---|
| Staphylococcus aureus | 18 | 18.00 |
| E.Coli | 9 | 9.00 |
| Chlamydia Igm positive | 16 | 16.00 |
| Enterococcus | 9 | 9.00 |
| Candida albicans | 8 | 8.00 |
| Candida species other than albicans | 6 | 6.00 |
| Trichomonas vaginalis | 6 | 6.00 |
| Coagulase negative staphylococcus | 5 | 5.00 |
| Klebsiella oxytoca | 3 | 3.00 |
| MRSA | 2 | 2.00 |
| haemolytic strept ococci | 1 | 1.00 |
| Pseudomonas aeruginosa | 2 | 2.00 |
| Proteus species | 1 | 1.00 |
| Acinitobacter | 1 | 1.00 |
| Enterobacter | 1 | 1.00 |
| Citrobacter | 1 | 1.00 |
| Etiological agent not found | 11 | 11.00 |
| Total | 100 | 100.00 |
Comparison of wet mount results (n=100)
| Wet Mount | No. | % |
|---|
| Clue cells | 44 | 44.00 |
| Pus cells | 20 | 20.00 |
| Trichomonas vaginalis | 06 | 6.00 |
| Inconclusive | 30 | 30.00 |
| Total | 100 | 100.00 |
Distribution of cases according to symptom
Distribution of cases according to socio-economic status
Distribution of cases according to literacy
Distribution of cases according to hygiene
Conclusion
Vaginal infections are common gynaecological problem. Known predisposing factors for symptomatic vaginal discharge are poor hygiene, low socioeconomic status, early sexual activity and multiple partners. The most ideal approach is the microbiological diagnostic approach for the aetiological diagnosis of symptomatic vaginal discharge. Large scale randomized controlled trials should also be used to elucidate the most effective treatment options. These trials must be followed by robust economic analyses to quantify the possible health gains. It can help clinicians to institute appropriate antimicrobial therapy to treat these conditions and prevent long term sequelae and also prevent the over treatment and development of resistance against various antibiotics. Further studies are recommended to emphasize the role of microbiological diagnosis, as clinical diagnosis alone can lead to false interpretation.
[1]. S Rekha, S Jyothi, Comparison of visual, clinical and microbiological diagnosis of symptomatic vaginal discharge in the reproductive age groupInt J Pharm Biomed Res 2010 1(4):144-48. [Google Scholar]
[2]. J Schwebke, Bacterial vaginosisCurr Infect Dis Rep 2000 2(1):14-17. [Google Scholar]
[3]. Poonam Choudhary, Laxmipriya Dei, S Sharma, A RCT on the efficacy of nimbadi yoni varti on abnormal vaginal discharge in reproductive aged womenJournal of Ayurveda and Holistic Medicine 2014 2(6):1-12. [Google Scholar]
[4]. Khamees Samia S, characterization of vaginal discharge among women Complaining of genital tract infection Omar Al-Mukhtar University, Tobruk, LybiaInt.J. of Pharm. & Life Sci 2012 3(10):1997-2002. [Google Scholar]
[5]. P G Larsson, B Carlsson, L Fahraeus, T Jakobsson, U Forsum, Diagnosis of Bacterial vaginosis: need for validation of microscopic image area used for scoring bacterial morphotypesSex Transm Infect 2004 80:63-67. [Google Scholar]
[6]. Snehalata Vishwanath, Vibha Talwar, Rajendra Prasad, Kurus Coyaji, Elias Christopher J, Zoysa Isabelle de, Syndromic management of vaginal discharge among women in a reproductive health clinic in IndiaSex Transm Inf 2000 76:303-06. [Google Scholar]
[7]. JE Tolosa, S Chaithongwongwatthana, S Daly, WW Maw, H Gaitan, P Lumbiganon, The international infection in pregnancy (IIP) study: variations in the prevalence of Bacterial vaginosis and distribution of morphotypes in vaginal smears among pregnant womenAm J Obstet Gynecol 2006 195(5):1198-1204. [Google Scholar]
[8]. MM Singh, R Devi, S Garg, M Mehra, Effectiveness of syndromic approach in management of reproductive tract infections in womenIndian J Med Sci 2001 55:209-14. [Google Scholar]
[9]. P Madhivanan, K Krupp, V Chandrasekaran, C Karat, A Arun, CR Cohen, Prevalence and correlates of Bacterial vaginosis among young women of reproductive age in Mysore, IndiaIndian J Med Microbiol 2008 26(2):132-37. [Google Scholar]
[10]. H Moi, Prevalence of Bacterial vaginosis and its association with genital infections, inflammation and contraceptive methods in women attending sexually transmitted disease and primary health clinicsInt J STD AIDS 1990 1(1):86-94. [Google Scholar]
[11]. P Mayaud, H Grosskurth, J Changalucha, Risk assessment and other screening options for gonorrhoea and Chlamydial infections in women attending rural Tanzanian antenatal clinicsBulletin of the WHO 1995 73:621-30. [Google Scholar]
[12]. M Laga, A Manoka, M Kivuvu, Non-ulcerative sexually transmitted diseases as risk factors for HIV-1 transmission in women: results from a cohort studyAIDS 1993 7:95-102. [Google Scholar]
[13]. P Madhivanan, MT Bartman, L Pasutti, Prevalence of T. vaginalis infection among young reproductive age women in india: implications for treatment and preventionSex Health 2009 6:339-44. [Google Scholar]
[14]. Vijaya Doddaiah, Dhanalakshmi Tumkur Anjaneya, Kulkarni Sunanda, Changing trends of vulvovaginal candidiasisJournal of Laboratory Physicians. 2014 6(1):216-19. [Google Scholar]
[15]. Srujana Mohanty, Immaculata Xess, Fahmi Hasan, Arti Kapil, Suneeta Mittal, Tolosa Jorge E., Prevalence and susceptibility to fluconazole of Candida species causing vulvovaginitisIndian J Med Res 2007 :216-19. [Google Scholar]
[16]. Meenakshi Malhotra, Seema Sood, Anjan Mukherjee, Sumathi Muralidhar, Bala Manju, Genital Chlamydia trachomatis: an updateIndian J Med Res 2013 138:303-16. [Google Scholar]
[17]. S Hawkes, L Morison, S Foster, K Gausia, J Chakraborthy, RW Peeling, Lancet 1999 354:1776-1781. [Google Scholar]