Cornelia de Lange syndrome (CdLS) is a rare, multiple congenital defect often called as Amsterdam dwarfism. The physical phenotype of CdLS includes low birth body weight, short stature and facio-cranial dysmorphia. The diagnosis of the syndrome is based on clinical grounds as there is no biochemical or chromosomal markers for CDLS that makes its diagnosis more complicated. The purpose of this paper is to present a clinical report of a boy emphasizing the importance of multidisciplinary approach for the diagnosis and treatment of this syndrome.
Case Report
A 7½-year-old boy reported to the Department of Pedodontics and Preventive Dentistry, ITS CDSR, Muradnagar, with a chief complaint of pain in right and left lower back tooth region since fifteen days. Pain was dull and intermittent in nature, which aggravated on chewing food and was relieved on taking medication. Past dental history revealed that patient had undergone pulp therapy in right and left lower back tooth region, one year back. After obtaining a detailed history from the parents, we came to know that the child was born prematurely at 32 wk weighing 2000 gms at birth. After birth the child was noted to have poor general health and delayed developmental milestones. Both parents and elder brother were asymptomatic, with no positive history of any deformity.
During physical examination of the patient, the height was 124 cm and weight 14kgs. The facial features of the child seemed dysmorphic, pilosity on the forehead with thick bushy eyebrows meeting in the midline( synophrys), long curly eyelashes, hypertelorism, long and full philtrum and low front and back hairlines [Table/Fig-1]. His ears were low set, outwardly placed and had thin lips with a crescent shaped mouth. He also had short neck, fairly small hands and feet,fifth finger clinodactyly and hirsutism [Table/Fig-2] Other features are explained in [Table/Fig-3]. Thus, taking orofacial features into consideration, Hand wrist radiograph was advised to assess the child’s growth and development [Table/Fig-4].
Clinical examination showed previously restored 75 and 85 along with Grade II mobility irt 75 and intraoral swelling irt 85. Intra-oral examination showed mixed dentition period ,with widely spaced and rotated irt 31 and 41; grossly decayed irt 54, 64,73 and occlusal caries irt 53,65. On the basis of thorough clinical examination, provisional diagnosis of chronic apical abscess irt 85, pulp necrosis irt 75, chronic irreversible pulpitis irt 54,64,73 and occlusal caries irt 53,65 was made.
After detailed examination , orthopantamograph(OPG) was advised to the patient,which revealed pulpotomised teeth irt 75 and 85, missing permanent teeth irt 32 and 42, root stumps irt 54,64,73. On the basis of oral and radiographic findings, the provisional diagnosis was confirmed [Table/Fig-5]. Other significant intraoral findings were macroglossia, high arched palate, enlarged tonsils, and excessive drooling of saliva [Table/Fig-6,7,8,9,10]. Patient also had a habit of lip biting which was further confirmed by the presence of hyperactive mentalis muscle.
Behaviour management of the child was a challenge as the patient was shy, hesitant to talk or communicate. Treatment plan comprised of glass ionomer restoration irt 65,53 and extraction irt 85,73, 75. Sealant application was done on permanent first molars followed by topical fluoride application. 54 and 64 were asymptomatic,thus left as natural space maintainers. Fixed lip bumper was cemented to intercept the habit of lip biting and to preserve the space in the mandibular arch [Table/Fig-10].
Discussion
Cornelia de Lange syndrome (Brachmann syndrome, Typus degenerativus amstelodamensis) is a multiple congenital anomaly, first documented in 1916 by W. Brachmann followed by Cornelia de Lange in 1933 [1,2]. CdLS is a relatively rare syndrome, affecting between 1/10,000 to 1/60,000 neonates.It is found more frequently in females (1.3: 1). Although, genetic and molecular basis of CdLS remain unclear, most cases are sporadic and only 10% of cases present chromosomal alterations of 3q 26:2-q23 region. Mutations in three cohesion proteins, NIBPL(Nipped-B) homolog gene and cohesion subunits SMC1A and SMC3,etiologically account for 65% of CdLS cases. Absence of Pregnancy associated plasma protein A(PAPPA) maybe considered as a marker for prenatal diagnosis [3,4]. CdLS is mainly characterized by distinct facial features ,growth retardation and limb anomalies with learning difficulties.
Van Allen classified CdLS into 3 types:
• Type I or classic patients: show characteristic facial and skeletal changes of CdLS
• Type II or mild patients: show characteristic facial features and minor skeletal abnormality.
• Type III show phenotypic manifestations of CDLS, related to chromosomal aneuploidies or teratogenic exposures [5]. Based on given classification, the present case falls into type II.
In classical cases, there is rarely any difficulty in making diagnosis, but it is the mildly affected cases that often go undiagnosed [6]. Significant features found in the present case are shown in [Table/Fig-3]. In addition, the child also had problem in swallowing due to enlarged tonsils.
Diagnosis for CdLS is complicated due to phenotypic variability and lack of definitive diagnostic marker. In the present case, the genetic testing was not done due lack of confirmatory genetic tests available particularly for this syndrome. Diffential diagnosis of CdLS is Coffin-Siris syndrome and Rubinstein-Taybi syndrome (RTS). However, our patient did not have delayed motor skills, laxity of joints, wide mouth with thick lips, absence of nails, hypoplasia of tips of fingers . The child also did not have muscle hypotonia, talon’s cusp, gingivitis. Therefore both the syndromes were excluded.
In this case, to assess the child’s growth, a comprehensive radiographic assessment was done using hand wrist radiograph which showed retarded skeletal age (4 y 6 mnth) confirming a forty percent delay in growth. Throughout life these patients present a weight and size inferior to that of their corresponding age [6]. When compared with the average weight for indian boys, the child was 10 kg underweight. Jackson et al (1995) reported that 33% of these children were delivered prematurely and had intrauterine growth retardation (IUGR) [7]. History from parents revealed that the child was also born prematurely at 32 wk. Brylewski (1978), has reported that large majority of such patients have IQ below 50 [8]. On psychiatric evaluation by a clinical psychologist , our patient had IQ of 55 suggesting moderate mental deficiency. Behaviour findings showed that the child was an introvert, only played with his brother and did not mix with other children or strangers. In this patient, we also found habit of lip biting which was timely intercepted by fixed lip bumper. The patient fell ill frequently therefore was referred to the pediatrician who advised echocardiography as a faint heart murmur was felt.
This case report stresses on the orofacial features and dental management of Cornelia de Lange syndrome. Diagnosing mild cases of this syndrome is a challenging task even for an experienced clinician. Medical and developmental complications associated with CdLS makes dental treatment difficult. Management of patients suffering from CdLS syndrome requires a team effort that includes geneticists, cardiologists, gastroenterologists, nutritionists, nephrologists, ophthalmologists and paediatrician.
Extra-oral photograph showing distinct facial features

Clinical picture showing hands of the patient

comparison of reported features of CdLS with the present case
| Common Manifestations Of Cdls | Reports From Literature [1,4,6,8] | Our Case |
|---|
| Cranium | Microbrachycephaly | + | - |
| Forehead | pilosity on forehead low anterior and posterior | + + | + + |
| Eyes | Bushy and confluent eyebrows (synophrys) Long curly eyelashes Ptosis, nystagmus | + + + | + + - |
| Nose | Anteverted nostrils | + | - |
| Mouth | Thin lips High arched palate Long philtrum Cleft palate,perioral cyanosis (rare) Disturbance of nasopharyngeal function | + + + + + | + + + - + |
| Mandible | Micrognathia, Macroglossia Spurs in the anterior angle of the mandible | + + + | - + - |
| Teeth | Microdontia (deciduous tooth) Delayed tooth eruption (deciduous tooth) Partial anadontia Dental malalignment Dental erosion,periodontal disease | + + + + + | - + + + - |
| Ears | Low set , outwardly placed ears Hypoacusis | + + | + + |
| Feet | Limb and digital anomalies | + | - |
| Other general features | Hirsutism Retarded bone age Structural anomalies of limbs Clinodactyly of fifth finger Delayed growth and development Cardiac, respiratory and GI abnormalities Mental retardation (varying degrees) Self injurious tendencies | + + + + + + + + | + + - + + +(cardiac) + (moderate) + (lip biting) |
Hand wrist radiograph showing delay in skeletal growth
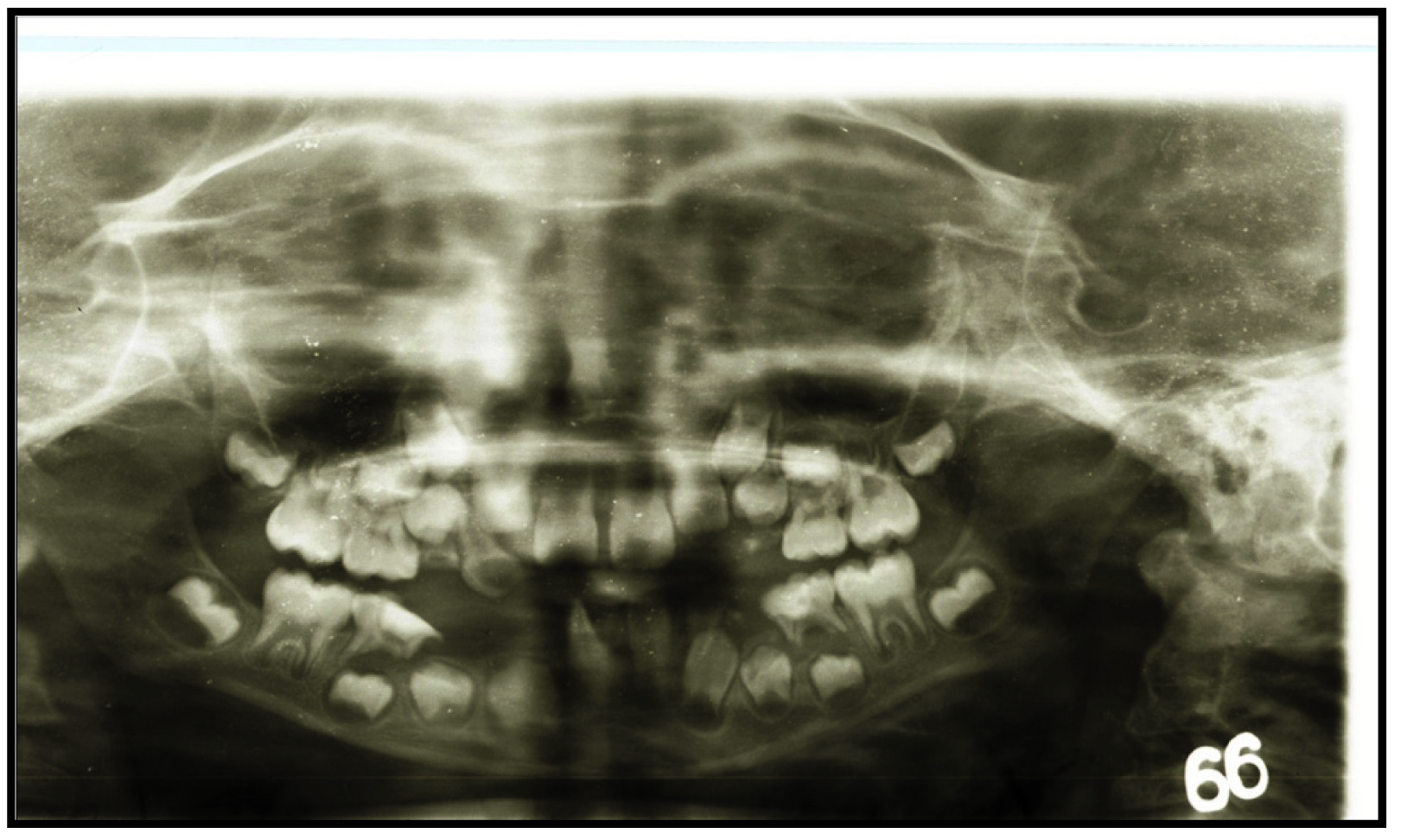
Pre-operative orthopantamograph (OPG)
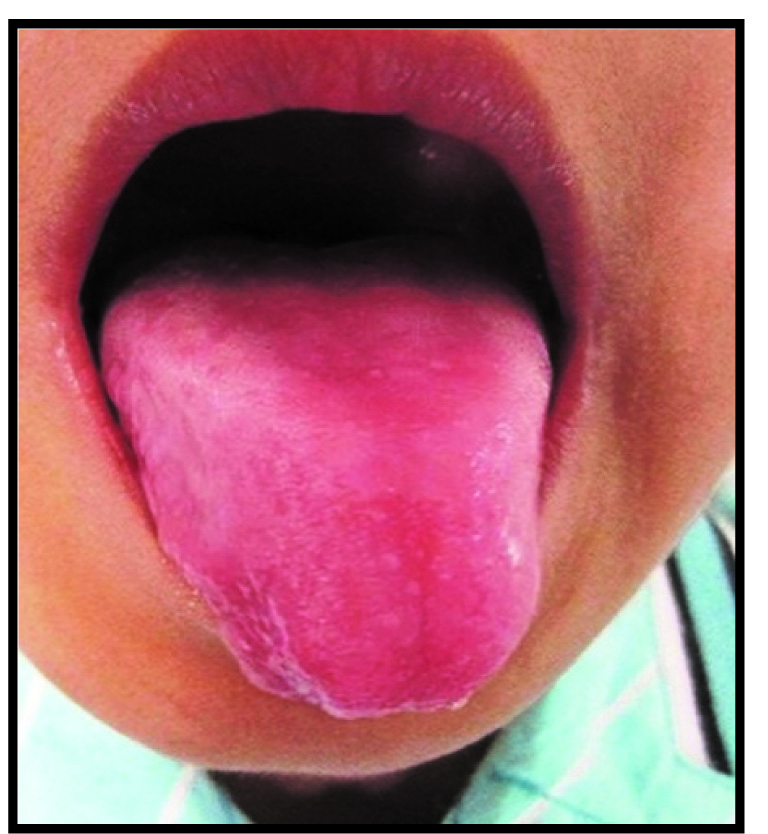
Clinical picture showing macroglossia

Intra-oral photograph showing high arched palate

Intra-oral photograph showing enlarged tonsils

Intra-oral photograph showing excessive drooling of saliva

Intra-oral photograph showing Fixed Habit breaking Appliance: Lip Bumper

Conclusion
It is important to understand that the role of pediatric dentist in treating patients suffering from CdLS is not just limited to treating the dental defects. Managing and shaping behavior of such children is crucial to deliver quality dental care. These patients are at a higher risk for dental caries, orthodontic problems and self inflicting oral habits which makes thorough evaluation and early intervention necessary.
[1]. DA Johns, DL Bhonsale, VY Shivashanker, M Johns, Aesthetic and functional management of a patient with Cornelia de Lange syndromeContemp Clin Dent 2012 3(Suppl 1):S86-91. [Google Scholar]
[2]. VD Desai, R Kaur, Neonatal syndrome present in adulthood: A new perspective of Cornelia de Lang syndrome-A case reportAsian J Pharma Hea Sci 2012 2(3):353-56. [Google Scholar]
[3]. J Grau-Carbó, J López-Jiménez, MJ Giménez-Prats, M Sànchez-Molins, Cornelia de Lange Syndrome: A case reportMed Oral Patol Oral Cir Bucal 2007 12(6):445-48. [Google Scholar]
[4]. R Muppa, NV Penumatsa, MK Duddu, D Karre, Complete oral rehabilitation in a child with classical cornelia de lange syndrome: A rare case reportJournal of Dr. NTR University of Health Sciences 2012 1(4):268-71. [Google Scholar]
[5]. AS Toker, S Ay, H Yeler, I Sezgin, Dental Findings in Cornelia De Lange SyndromeYonsei Med J 2009 50:289-92. [Google Scholar]
[6]. SS Reddy, V Shweta, P Chauhan, K Sahana, CORNELIA DE LANG SYNDROMEe-Journal of Dentistry 2012 2(4):269-72. [Google Scholar]
[7]. L Jackson, AD Kline, MA Barr, S Koch, De Lange syndrome: A clinical review of 310 individualsAm J Med Genet 1993 47:940-46. [Google Scholar]
[8]. D Gupta, S Goyal, Cornelia de Lange syndromeJ Indian Soc Pedod Prev Dent 2005 23(1):38-41. [Google Scholar]