Tuberculosis of Waldeyer’s Ring with an Atypical Presentation as Chronic Adeno-Tonsilitis
Panduranga M Kamath1, Vijendra S Shenoy2, Nirupama M3, Vishnu Prasad4, Nazeem A Majeed5
1Professor, Department of ENT and Head & Neck Surgery,Kasturba Medical College, Mangalore, Manipal University, India.
2Associate Professor, Department of ENT and Head & Neck Surgery,Kasturba Medical College, Mangalore, Manipal University, India.
3Associate Professor, Department of Pathology,Kasturba Medical College, Mangalore, Manipal University, India.
4Senior Resident, Department of ENT and Head & Neck Surgery,Kasturba Medical College, Mangalore, Manipal University, India.
5Resident, Department of ENT and Head & Neck Surgery,Kasturba Medical College, Mangalore, Manipal University, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vijendra Shenoy S, Associate Professor, Department of Otolaryngology, Kasturba Medical College Hospital, Attavar, Mangalore – 575 001, Manipal University, Karnataka State, India.
E-mail: drvijendras@gmail.com
Primary tuberculosis of the oropharynx and nasopharynx is a rare clinical entity.It usually arises secondary to pulmonary tuberculosis. We report a rare case of a 20-year-female, who presented with fever and throat pain. Examination revealed hypertrophied adenoids and tonsils, which was ultimately proved as tuberculosis.Enlargement of the palatine tonsils could be due to a multitude of causes, and a thorough evaluation is necessary to arrive at the right diagnosis.Increased awareness of nasopharyngeal and oropharyngeal tuberculosis is important in tropical countries, as the disease may be overlooked resulting in inappropriate management.
Adenotonsils, Langhans giant cells, Oral cavity
Case Report
A 20-year-female presented to our centre with severe throat pain, progressive dysphagia and difficulty in breathing for ten days. The pain was constant in nature and was aggravated on swallowing. She also had low grade fever and malaise for the same duration. There was associated nasal block and nasal discharge. There was no history of cough or change in voice. She had no previous history of any similar complaints.
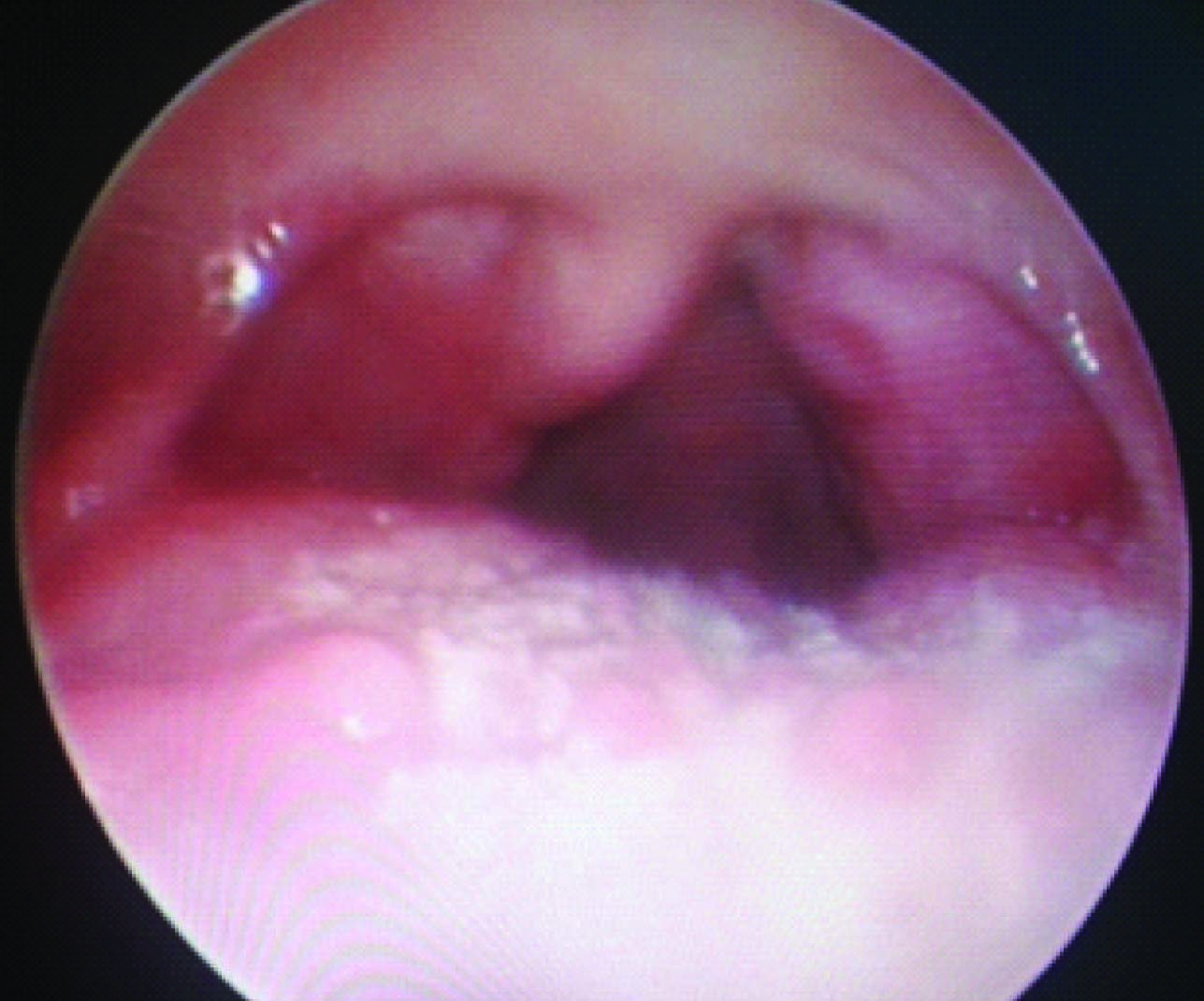
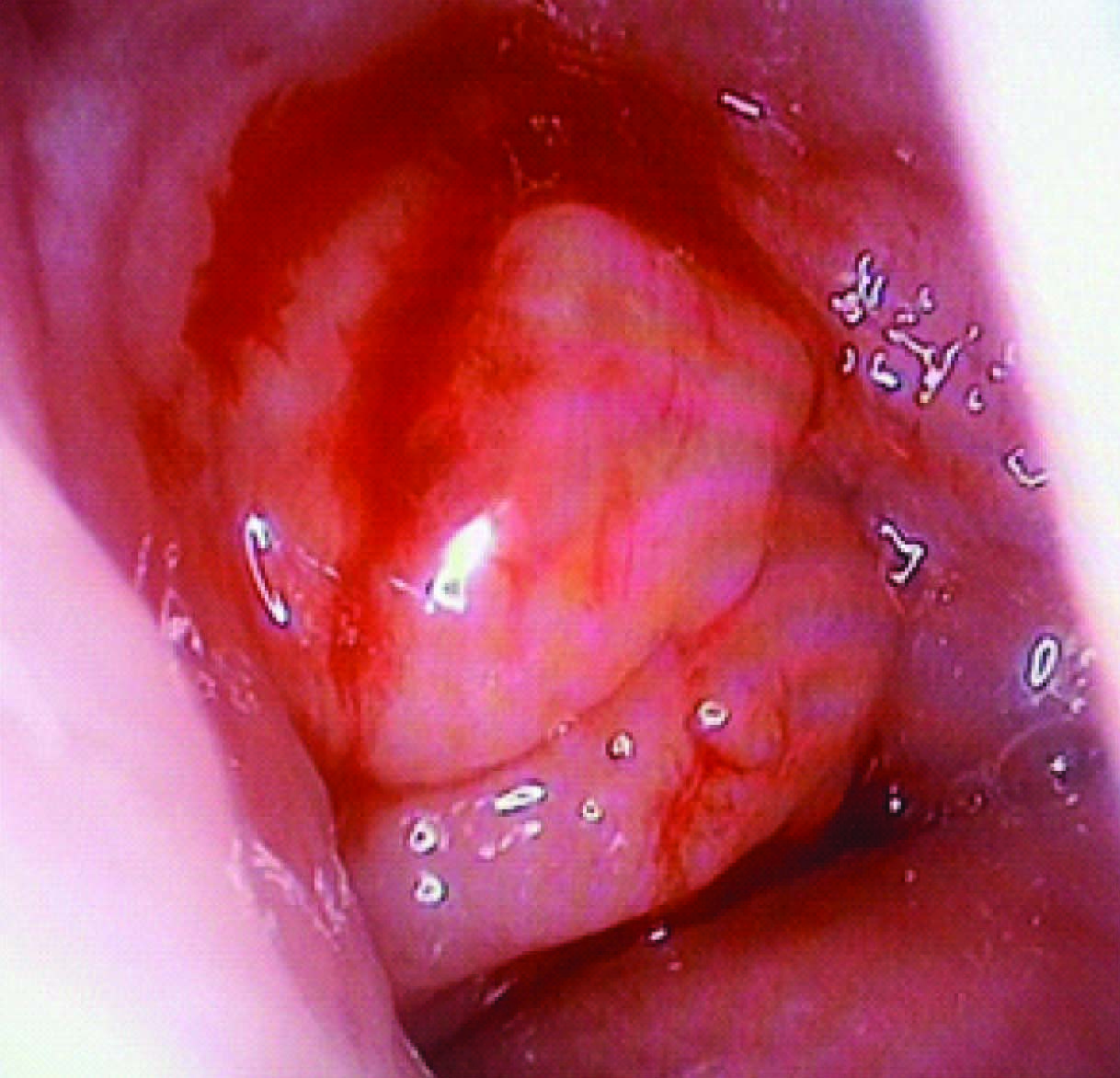
Clinical examination revealed her to be afebrile and her vitals were stable. On examination of the oral cavity, the anterior pillars were congested bilaterally.The palatine tonsils were congested and showed grade 3 enlargement bilaterally. The posterior pharyngeal wall was also congested and granular. In view of her nasal block, a diagnostic nasal endoscopy was performed which showed marked hypertrophy of the nasopharyngeal lymphoid tissue involving the roof and lateral wall of the nasopharynx, and completely obstructing the posterior nasal choanae [Table/Fig-1,Table/Fig-2]. On palpation of the neck, bilateral cervical lymph nodes were palpable, which were significantly enlarged, tender, and firm in consistency.
Hematological investigations revealed a total leucocyte count of 7300 /cubic mm with a neutrophil count of 82%.The ESR was 32 mm at the end of the first hour. All other routine blood investigations were found to be normal. The patient was seronegative for HIV. Keeping in mind a provisional diagnosis of Infectious Mononucleosis, a Monospot test was done which returned as negative. Throat swab showed Candida Gieberta. Her chest X-ray was normal. Sputum was negative for acid fast bacilli. An ultrasound scan of the neck was done which showed bilateral hypoechogenic cervical lymph nodes with echogenic hilus. FNAC of the cervical lymph node showed reactive adenitis.
She was treated conservatively with intravenous antibiotics, and supportive management for ten days following which her symptoms improved but the nasopharyngeal lymphoid tissue and paltine tonsil hypertrophypersisted, leading to obstructive symptoms. To rule out any malignant cause of tonsillar enlargement and to relieve the patient of her obstructive symptoms, an endoscopic adenoidectomy and tonsillectomy was performed. The tonsillar tissue was friable and there was considerable bleeding during the operative procedure which was controlled.
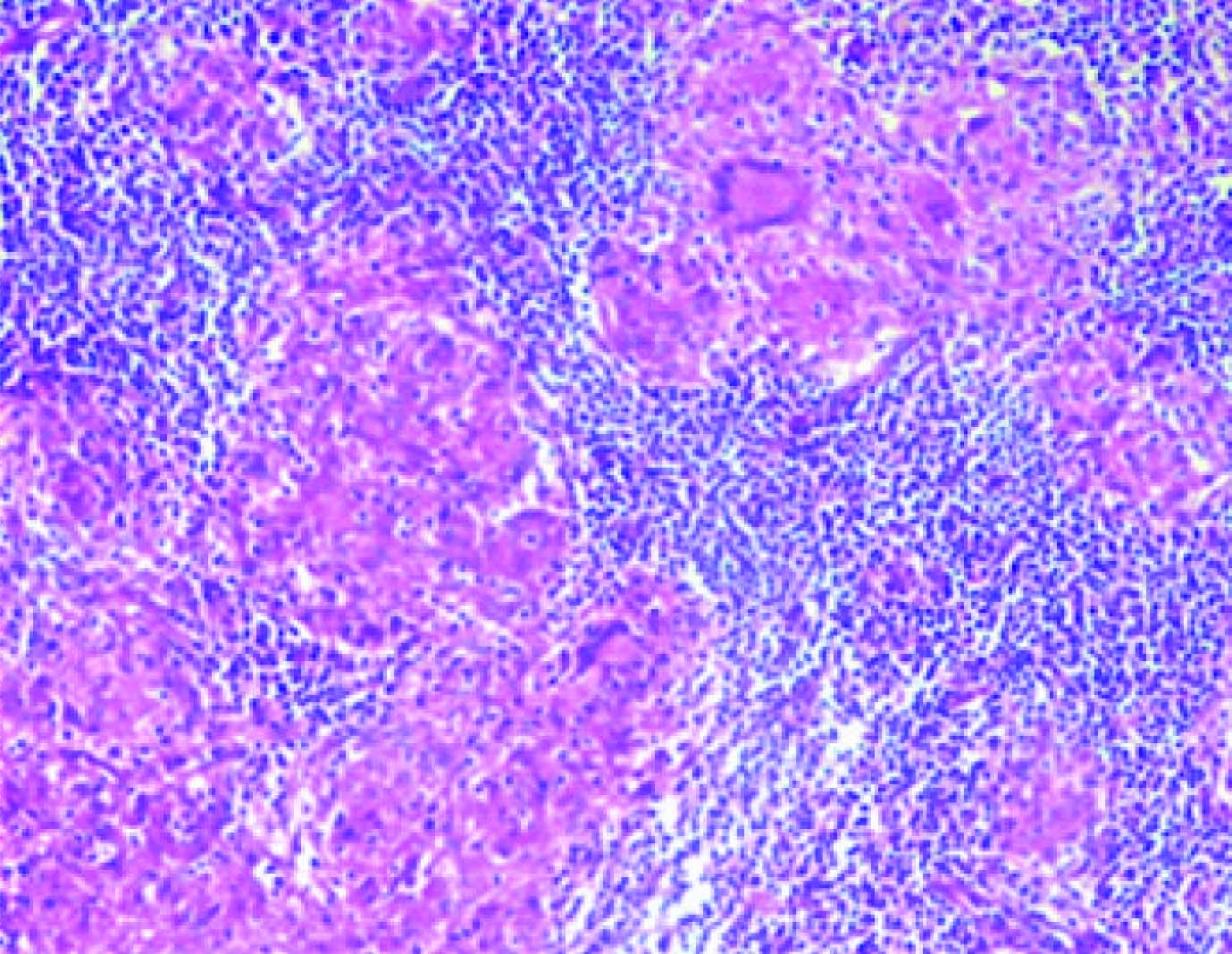
Gross examination showedmarkedly enlarged and congested adenotonsils. Cut surface showed small cheesy white material with map like areas. Microscopic examination revealed confluent caseating epithelioid granulomas with areas of fibrosis. Many Langhans giant cells were seen [Table/Fig-3]. Ziehl-Neelsen staining for AFB was found to be negative. Patient was started on antitubercular treatment and is doing fine after 6 months.
Discussion
Tuberculosis remains one of the major causes of morbidity and death worldwide. But it is rare to find tuberculosis manifesting in the tonsils without any primary pulmonary focus [1]. Tuberculosis of the oral cavity is rare and the tonsillar forms are extremely uncommon [2]. Prior to the introduction of chemotherapy, when tonsils removed from asymptomatic patients were subjected to histopathological examination, 6.5% of the tonsils were found to be infected with tubercles [3]. With the advent of effective antitubercular therapy and pasteurisation of cow’s milk, a considerable reduction in the worldwide prevalence of tuberculosis was achieved and tonsillar tuberculosis became rare [4]. The upper respiratory tract is generally resistant to tuberculosis. Saliva by virtue of its cleansing action is thought to have an inhibitory effect on tubercular bacilli. The inhibitory effect of saliva is due to the presence of saprophytes, the antagonism of striated musculature to bacterial invasion, and the thickness of the epithelial covering of the oropharyngeal mucosa [5]. Involvement of the oral cavity and oropharynx by tuberculosis can be primary or, more often, secondary to pulmonary tuberculosis. The lesions of primary oral tuberculosis generally occur in younger patients whereas, secondary lesions are most commonly seen in older individuals [6]. Oral tuberculosis may occur at any site, but most commonly occurs on the tongue. Other sites which may be involved include the palate, lips, gingiva, buccal mucosa, palatine tonsils and floor of mouth [7]. Our patient was diagnosed to have tuberculosis of the tonsils and adenoids. A similar disease was reported in Russia where a patient presented with dysphagia, and examination revealed a soft friable mass involving the nasopharynx and tonsils [8]. A biopsy was taken from the right tonsil which showed caseating granulomas and the patient was diagnosed to have primary tuberculosis of the tonsils. Oral cavity tuberculosis is difficult to differentiate from other conditions based on clinical signs and symptoms alone. Therefore a high index of suspicion should be kept in mind while evaluating a patient presenting with fever, sore throat and malaise. The lesion may occur in a variety of forms, such as an ulcer, nodule, tuberculoma and peri apical granuloma [9]. The identification of such a tuberculous lesion in the oral cavity is an unusual finding and it usually indicates underlying primary pulmonary tuberculosis. Therefore in all cases of oral cavity tuberculosis, the patient should be evaluated for pulmonary tuberculosis inspite of having no clinical symptoms or signs of pulmonary disease. However, in our case there were no signs of pulmonary tuberculosis. Tuberculosis of the tonsil is rare, but tonsillar tuberculosis may be seen in immunocompromised individuals, such as people who have HIV infection, and in chronic alcoholics. A wide spectrum of diseases should be borne in mind while diagnosing a patient with tuberculosis of the tonsil. These include traumatic ulcer, aphthous ulcer, Wegeners granulomatosis, malignancy and syphilis [10]. It has been suggested that such infections are acquired by inhalation, and the disease is harboured in the Waldeyer’s ring [11]. The organism may also enter through minor breaks in the mucosal surface [12]. The individual may be self-inoculated through infected sputum, or by hematogenous or lymphatic dissemination [13]. The diagnosis of tonsillar tuberculosis is made by histopathological examination and the identification of tubercle bacilli. Treatment is in the form of antituberculosis therapy [8].
Bilateral tonsillar enlargement
Caseating epithelioid granulomas with langhans gaint cells and admixed chronic inflammatory infiltrate
Conclusion
Patients with primary tuberculosis affecting the nasopharynx (adenoids) and oropharynx (palatine tonsil) has rarely been reported in the literature. Since India is a country with a high incidence of tuberculosis, the diagnosis of tonsillar tuberculosis should be borne in mind while evaluating any patient with enlarged tonsils who is not responding to treatment. It should also be considered in any patient with pulmonary tuberculosis who is found to have tonsillar hypertrophy.
[1]. P Prasad, M Bhardwaj, Primary Tuberculosis of Tonsils: A Case Report. Case Rep Med 2012 2012:120382 [Google Scholar]
[2]. F Ricciardiello, S Martufi, M Cardone, Otorhinolaryngology-related tuberculosisJ ActaOtorhinolaryngol Ital 2006 :38-42. [Google Scholar]
[3]. S Jadia, A Chauhan, R Hazari, A Maurya, R Biswas, An unusual case of recurrent tonsillitisBMJ Case Rep 2010 2010 [Google Scholar]
[4]. N Kulkarni, GS Gopal, SG Ghaisas, N Gupte, Epidemiological considerations and clinical features of ENT tuberculosisThe Journal of Laryngology & Otology 2001 115(07):555-58. [Google Scholar]
[5]. K Yamamoto, F Iwata, A Nakamura, Tonsillar tuberculosis associated with pulmonary and laryngeal fociInt Med 2002 41(8):664-66. [Google Scholar]
[6]. MH Dadgarnial, Baradaranfar Yazdani A Kouhi, Oropharyngeal tuberculosis: an unusual presentationActa Medica 2008 46:521-24. [Google Scholar]
[7]. S Kataria, S Singh, P Tanwas, S Kumar, G Singh, Primary tuberculosis of the tongue in an immunocommpetent patient: a case reportAsian Pacific Journal of Tropical Disease 2012 2(1):78-79. [Google Scholar]
[8]. Fl Chumakov, NV Gerasimenko, Isolated tuberculosis of pharyngeal and palatine tonsilVestn Otonnolanngol 2000 2:58 [Google Scholar]
[9]. I Dimitrakupoulos, L Zouloumis, N Lazaridis, D Karakasis, G Trigonidis, L Sichletidis, Primary tuberculosis of the oral cavityOral Surg Oral Med Oral Pathol 1991 72:712-15. [Google Scholar]
[10]. KB Gupta, S Tandon, TS Jaswal, S Singh, Tuberculosis of tonsil with unusual presentationInd J Tub 2001 48:223-24. [Google Scholar]
[11]. E Selimoglu, Primary tonsillar tuberculosisJ Laryngol Otol 1995 109(9):880 [Google Scholar]
[12]. NK Jain, SP Agnihotri, U Alavadi, Tubercular ulcer of mouth following clove chewing in a pulmonary tuberculosis patientCurr Med Trends 2002 6:1219-22. [Google Scholar]
[13]. N Gupta, P Nuwal, ML Gupta, RC Gupta, RK Dixit, Primarytuberculosis of soft palateIndian J Chest Dis Allied Sci 2001 43:119-21. [Google Scholar]