Cutaneous Angiosarcoma - A Rare Case Report in Indian Female!
Meenakshi Shetty1, Raghavendra Bhat2, Parul Kodan3
1 Associate Professor, Department of Medicine, Kasturba Medical College, Mangalore, Karnataka, India.
2 Professor and Head, Department of Medicine, KMC, Kasturba Medical College, Mangalore, Karnataka, India.
3 Post Graduate Student, Department of Medicine, Kasturba Medical College, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Raghavendra Bhat, Professor and Head, Department of Medicine, Kasturba Medical College, Mangalore, Karnataka, India. E-mail : nita2005bhat@yahoo.co.in
Cutaneous angiosarcoma is a rare vascular tumour especially of elderly males. We present a rare case of elderly female who presented with scalp lesion, parotid swelling and posed a diagnostic challenge. Further work up including biopsy of the lesion revealed the diagnosis of cutaneous angiosarcoma. Rarity of the case due to presence of this rare tumour in a darkcolored female and wide spread presentation of the tumour prompted us to report the case. This case adds to the literature of few cases describing this rare tumour in Indian subcontinent. It attempts to alert the clinicians of this entity, as early diagnosis of the tumour may possibly improve the already known dismal prognosis!
Biopsy, Chemotherapy, Skin lesion
Case Report
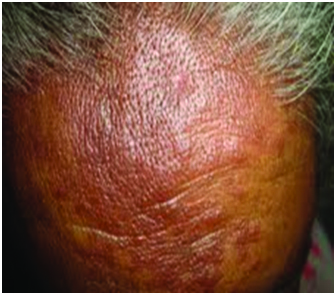
A 67-year-old female who was known case of Diabetes Mellitus and Hypertension on came with history of facial swelling for past four months which was insidious in onset and progressive. She gave history of skin lesions over the face, behind the ear and scalp [Table/Fig-1,Table/Fig-2,3] which were not itchy and painless and progressively increasing over last 4 months. She complained of undue fatigue for 6 months. There was no photosensitivity, recent alopecia or skin lesions elsewhere. She also gave history of swelling around eye for 3-4 months which was gradually increasing. She had no history decreased urine output, breathlessness on exertion, yellowish discoloration of skin and sclera, fever and cough.
Malar skin rash and plaques in scalp region

Post auricular cystic lesion

Shows plaques in scalp region
On examination, patient was moderately built and nourished. She was conscious and oriented. She was hemodynamicaly stable. There was no pallor, icterus, clubbing, cyanosis or Raynaud’s phenomenon. Bilateral pitting pedal edema was present. Pitting periorbital edema with erythema was present. Eye examination was normal. No swelling in thyroid region.
Multiple indurated, hyper pigmented, erythematous pitting plaques were noticed on the scalp. Erythematous rash was present in malar area. Diffuse swelling present in the left parotid region, soft to firm in consistency, non tender, no local rise of temp. Fluid filled cystic lesion behind her left ear overlying left mastoid was present. Systemic examination was within normal limits.
Based on history and examination we initially considered differential of lupus, connective tissue disorder and hypothyroidism. Due to parotid involvement and skin lesion we considered a differential diagnosis of sarcoid which is a common lesion in black women. Also other differentials of parotid swelling like Sjogrens syndrome, Non-Hodgkin’s lymphoma were considered but ruled out on further workup.
Routine investigations showed: Hemoglobin - 11.8 gm%, Total Count - 7470 cells/mm3, ESR: 2 mm/1st hour, Platelets: 2, 53,000/mm3, urea - 17mg/dl, creatinine - 0.7 mg/dl. LFT within normal limits, Serum electrolytes and Urine routine were normal. Thyroid profile (T3, T4 & TSH) was normal. To look for any multisystem involvement Chest X-ray, USG abdomen; ECG and ECHO were done which were normal. HIV test was done which was negative.
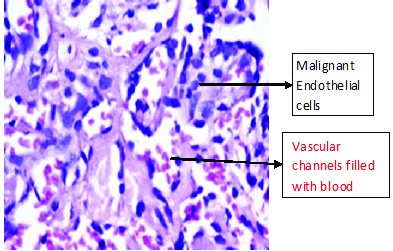
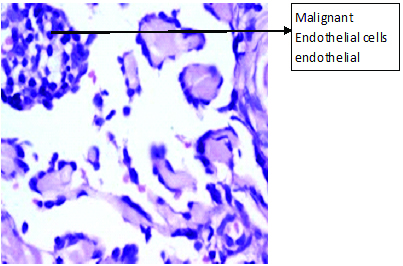
USG neck revealed enlargement of left parotid gland with multiple hypoechoic lesions of varying sizes. FNAC of the left parotid gland revealed a lymphoepithelial lesion. However, Sarcoidosis was unlikely because Chest X-ray did not reveal any hilar lymphadenopathy, ESR was normal and serum Calcium was normal. Punch biopsy from the plaques over scalp revealed atrophic changes of epidermis, with invasive tumour in dermis made up of mesh work of vessels with their endothelial cells showing oval to elongated hyperchromatic nuclei. The histological features were suggestive of cutaneous angiosarcoma [Table/Fig-4–5]. This case shows a rare case of cutaneous angiosarcoma of scalp in elderly female who presented with periorbital edema, skin lesion and parotid swelling signifying an extensive angiosarcoma.
Cutaneous Angiosarcoma - H&E section shows anastomosing vascular channels lined by highly atypical endothelial cells,
Cutaneous Angiosarcoma - H&E section shows highly atypical endothelial cells
Patient was advised chemotherapy and radiotherapy. However unfortunately was lost to follow up.
Discussion
Angiosarcomas are rare neoplasms. Approximately 50% of angiosarcoma occur in the head and neck, but they account for less than 0.1% of head and neck malignancies [1]. It is usually seen in white elderly male and rare in coloured races [2]. This rare malignancy has infrequently been reported from non-white races and such cases are confined to handful of case reports [3]. Our case report is unique as it presents in elderly female with skin type 5. Data from the National Cancer Institute's Surveillance, Epidemiology, and End Results program which recorded 434 cases of cutaneous angiosarcoma from 1973 to 2007 concluded that the incidence of cutaneous angiosarcoma was most common in white (88%) with a mean age of 73 years and African Americans made up only 4% of the cases [4].
Cutaneous angiosarcoma of the scalp and face is the most common form of angiosarcoma. Most patients present with an enlarging bruise, a blue-black nodule, or an unhealed ulceration. Our patient also presented with scalp and face lesions. Case reports of eyelid and periocular lesions have been reported but are rare [5]. However unlike the common presentation our patient presented with plaques on scalp, malar rash, periorbital swelling and post auricular cyst- such a presentation with so many lesions of different kind which all started almost at the same time and were now progressive is extremely rare and possibly the first of its kind in literature with all these lesions together!
Etiology of cutaneous angiosarcoma is unclear but may be related to previous radiation exposure or chronic lymphedema [6]. Few cases related to lesion after trauma have been documented although its significance is unknown [7]. However in our case there was no such history and no known predisposing factor was there in our patient.
Angiosarcoma is a fast spreading tumour with the highest rate of lymph node metastasis among all soft tissue sarcomas of the head and neck. Our patient also had extensive involvement of face and scalp. She also had parotid and periorbital swelling possibly due to widespread disease. The prognosis of tumour has been reported as dismal. Late diagnosis may be a possible reason for poor prognosis of the disease.
Early detection by means of biopsy offers the only realistic chance of a cure [8]. Diagnosis is based on the microscopic features of the biopsy or specimen and the ultrastructural and histochemical markers.Morgan et al., has shown that the most common histologic pattern was characterized by anastomosing dissecting sinusoids lined by atypical endothelial cells (64%) with 15% of cases showing a diffuse epithelioid or spindle cell proliferation and 21% showing a mixture of the 2 histologic patterns [8].
The optimal treatment for angiosarcoma of the skin involves complete surgical resection, followed by local radiation therapy. If surgical excision not possible, no standard treatment is documented [9]. Palliative Chemotherapy and radiotherapy alone and in combination have been tried with varying results. Liposomal doxorubicin has been tried as single agent chemotherapy [10]. Paclitaxel has been tried [11]. Despite aggressive treatment, prognosis is poor, although early detection and multidisciplinary approach may improve survival [12]. The median time of survival ranges from 15-24 months, with a 5-year survival rate of 12-33%. Findings of significantly favourable prognostic importance appear to be tumour size (<5 cm), complete surgical resection, and a moderate or marked lymphoid infiltrate in and around the tumour. Death can occur either from local extension or metastasis. Delayed diagnosis and treatment explain, in part, the poor prognosis of cutaneous angiosarcoma.
Conclusion
Our case is unique as it describes a rare presentation of this rare tumour in an Indian female and shows extensive and peculiar form of the disease presentation and adds to the existing literature of rare case reports of extensive form of this rare malignancy. The presence of this rare malignancy in elderly Indian female is unusual and posed a diagnostic dilemma for us. However prognosis in our case was dismal. Diagnosis at an earlier stage may have possibly given us more option for management and better outcome.
[1]. Sturgis EM, Potter BO, Sarcomas of the head and neck regionCurr Opin Oncol 2003 15(3):239-52. [Google Scholar]
[2]. Matsumoto K, Inoue K, Fukamizu H, Okayama H, Takigawa M, Prognosis of cutaneous angiosarcoma in Japan: A statistical study of sixty-nine casesChir Plastica 1986 8:151 [Google Scholar]
[3]. Ambujam S1, Audhya M, Reddy A, Roy S, Cutaneous angiosarcoma of the head, neck, and face of the elderly in type 5 skinJ Cutan Aesthet Surg 2013 6(1):45-47. [Google Scholar]
[4]. Albores-Saavedra J, Schwartz AM, Henson DE, Kostun L, Hart A, Cutaneous angiosarcoma. Analysis of 434 cases from the Surveillance, Epidemiology, and End Results Program, 1973-2007Ann Diagn Pathol 2011 15(2):93-97. [Google Scholar]
[5]. Ettl T, Kleinheinz J, Mehrotra R, Schwarz S, Reichert TE, Driemel O, Infraorbital cutaneous angiosarcoma: A diagnostic and therapeutic dilemmaHead Face Med 2008 4:18 [Google Scholar]
[6]. Jonathan S Zager. Angiosarcoma of the Scalp. eMedicine. Retrieved 22/8/2014 from http://emedicine.medscape.com/article/1296442-overview [Google Scholar]
[7]. Glickstein J, Sebelik ME, Lu Q, Cutaneous angiosarcoma of the head and neck: a case presentation and review of the literatureEar Nose Throat J 2006 85:672-74. [Google Scholar]
[8]. Morgan MB, Swann M, Somach S, Cutaneous angiosarcoma: a case series with prognostic correlationJ Am Acad Dermatol 2004 50(6):867-74. [Google Scholar]
[9]. DeVita VT Jr, Hellman S, Rosenberg SA, Cancer: Principles & Practice of Oncology 2008 8th edPhiladelphia, PaLippincott Williams & Wilkins [Google Scholar]
[10]. Ockenfels H, Brockmeyer N, Hengge U, Goos M, Cutaneous angiosarcoma: a novel therapy with liposomal doxorubicinJ Eur Acad Dermatol Venereol 1996 6:71 [Google Scholar]
[11]. Fata F, O’Reilly E, Ilson D, Pfister D, Leffel D, Kelsen DP, Paclitaxel in the treatment of patients with angiosarcoma of the scalp or faceCancer 1999 86:2034-37. [Google Scholar]
[12]. Rathod GB, Jain A, Parmar P, Cutaneous angiosarcoma of face – a case reportIJCRR 2013 5(1):120-26. [Google Scholar]