Introduction: An adequate knowledge of anomalies of gonadal veins will help the radiologists and surgeons in recognition and protection of these veins which play major roles in thermo-regulation that is essential for the efficient functioning of testis on which the survival of the human species depends.
Aim: The aim of this work is to present an analysis of the anatomical variations of gonadal veins. An effort has also been made to explicate the possible embryological model of development of such variants and to present the variable clinical aspects concerning them.
Materials and Methods: Gonadal veins in 60 dissection room cadavers were examined for variations from the classic anatomic description.
Result: In the present study, out of 60 cases, male: female ratio was 2:1(40:20) in which no variation was found in ovarian veins. In the 18 (45%) cases, testicular veins showed variations which consist of duplication and atypical drainage.
Discussion: Variations of drainage of gonadal vein are due to error of embryological development in venous shift and alteration in anastomotic channel of post-cardinal, supra-cardinal and sub cardinal veins.
Conclusion: The gonadal veins present numeric variations as well as variations in its site of drainage, which attributed to the various pathological conditions as varicocele and pelvic congestion syndrome, leading to infertility in patients. Hence, in -depth knowledge of these developmental anomalies of gonadal veins is important.
Introduction
In the era of invasive interventions such as laparoscopic surgery and transplantation of kidney, the variations of gonadal veins are of utmost clinical importance. In living, donor gonadal vein is a readily available material for vascular reconstruction. Vein extension with gonadal vein has been described as a simple and safe method to elongate renal vein [1] . An adequate knowledge of vascular anomalies of testicular veins will help the radiologists and surgeons in recognition and protection of these veins which play major roles in the thermo-regulation that is essential for the efficient functioning of testis on which, the survival of the human species depends.
The gonadal veins are anatomically asymmetric. The testicular veins originate from the pampiniform plexus that condense to form four veins at the superficial inguinal ring, two veins at the deep inguinal ring and one vein at variable levels. The left testicular vein drains in the left renal vein at a straight angle, whereas the right testicular vein drains directly in the inferior vena cava (IVC) at an oblique angle [2] . This anatomical difference is responsible for relatively weak hemodynamic in the left testicular vein and is considered to be a cause of frequent left varicocele [3] . The ovarian veins are similar to the testicular veins as they originate from the plexus in the broad ligament near the ovary and fallopian tube, then left ovarian vein joins the left renal vein and right one drains the IVC [4] .
Variations of gonadal veins may reflect complicated embryogenesis in this area. The gonadal vein presents numeric variations as well as variations in its site of drainage, which attributed to the various pathological conditions as varicocele, pelvic congestion syndrome etc, However, very little is found in the literature about the gonadal veins and their anatomical variations. Therefore, the gonadal veins in 60 dissection room cadavers were examined for variations from the classic anatomic description. The objective of this work is to present an analysis of the anatomical variations of number, course and locale of drainage. An effort has also been made to explicate the possible embryological model of development of such variants and to present the variable clinical aspects concerning them.
Materials and Methods
Material of this study comprised of 60 (120 gonadal veins) well embalmed dissection room cadavers of known sex (40 Male & 20 Female), obtained from Department of Anatomy, GMC Amritsar and AIMSR, Bathinda, Punjab, India. The human cadavers were serialized from 1-60 with suffix M for male and F for female. The abdominal cavity was opened by routine dissection procedure according to cunningham Manual of Practical Anatomy [5] and the retroperitoneal structures were exposed. The connective tissue surrounding the gonadal veins and their tributaries were removed to provide a clear field of vision. Various observations were made and compared with available literature.
Three anatomical aspects of gonadal veins were considered
1) Number.
2) Locale of drainage.
3) Termination angle.
Results
In the present study, out of 60 cases, male: female ratio was 2:1(40:20) in which no variation was found in ovarian veins. In the 18 (45%) cases, testicular veins showed variations which consist of duplication and atypical drainage. These variations were found more frequently in the left side 12 (30%) cases as compared to right 2 (5%). In 4 (10%) cases, the variations were present bilaterally.
The left testicular vein was a tributary of left renal vein in all cases and drained into it at a straight angle. It drained as a single tributary in 28 (70%) cases and as double in 12 (30%). Abnormal drainage of left testicular vein was associated with variation of renal veins. The right testicular vein terminated into IVC in 34 (85%) cases, into right renal vein in 4 (10%) cases and into both in 2 (5%) cases. In 35 (87.5 %) cases, the right testicular vein drained in IVC at an acute angle, and in 5 (12.5%) cases, the angle of drainage in right renal vein was straight. It drained as single tributary in 38 (95%) cases and as double in 2 (5%) of cases.
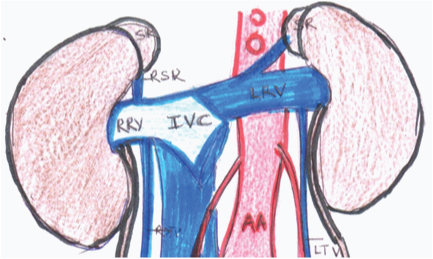
A variation regarding the drainage of right testicular vein was encountered in a case where the right testicular vein and right supra renal vein drained into right renal vein instead of IVC [Table/Fig-1a,Table/Fig-1b].
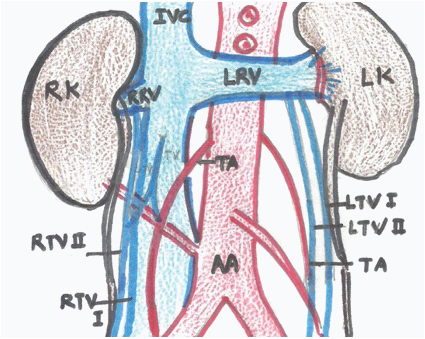
In another uncommon case, both testicular veins showed variations. The right testicular vein had a normal course initially and about 7cm before its termination, it bifurcated into two veins of almost equal size. Medial right testicular vein drained into IVC and lateral one into right renal vein. There was an arterio-venous anastomosis between medial right testicular vein and right testicular artery. In the left side, two testicular veins, formed 2cm above deep inguinal ring, drained into left renal vein. An accessory right renal artery was also entering lower pole of right kidney in this case coursing posterior to testicular vessels and ureter [Table/Fig-2a,Table/Fig-2b].
Discussion
The anatomy of the gonadal veins has assumed importance because of the development of new operative techniques within the abdominal cavity for operations such as varicocele, undescended testes and renal transplantations [6]. During laparoscopic surgery of abdomen and pelvis, most of the complications are due to unfamiliar anatomy in the operative field [7]. Knowledge of the variations of gonadal vessels may provide safety guidelines for these techniques [8]. Variations of drainage of gonadal vein are due to error of embryological development in venous shift and alteration in anastomotic channel of post-cardinal, supra-cardinal and sub cardinal veins [9].
Embryological basis
The development of gonadal vein is closely related to the development of renal vein and IVC. The embryogenesis of these veins involves the development, regression, anastomosis and replacement of three pairs of venous channels: posterior cardinal, sub-cardinal and supra-cardinal. Anastomosis between the supra-cardinal and the sub-cardinal veins, which occur bilaterally, form the renal segment of IVC [10]. Gonadal vein develops from caudal part of sub-cardinal vein and it drains into the supra-sub cardinal anastomosis. In the right side, this supra- sub cardinal anastomosis and also a small portion of Sub-cardinal vein are incorporated into the formation of IVC, so right gonadal vein usually drains into the IVC. In the left side, this supra-sub cardinal anastomosis forms part of left renal vein where the left gonadal vein drains [11].
In our study, only testicular veins showed variations which were encountered more in the left side. Asala et al., [12] have done an extensive study on the gonadal vessels and have found that the variations were seen in 21.3% of the cadavers, were more common on the left side and in 18.8% of cases, the variations were present bilaterally.
The incidence of duplicated testicular vein may act as additional collateral route. Duques et al., [13] presented a single testicular/ovarian vein in 85.2% and double in 8.8% of cases. Presence of duplicated testicular veins has been found to be more common on left side [2,10]. According to study of Lechter et al., [14], double testicular veins occurred in 5% of cases in right side while in left side, two veins in 15%, three veins in 2% and four veins in 1% of the cases were found . In the present study also, the testicular vein showed duplication in 30% cases of left side and in 5% cases of right side. In no case triple or four left gonadal veins were found as was reported earlier [Table/Fig-3].
Duplication of Gonadal vein is of interest for radiologists in avoiding diagnostic errors as well as to surgeons as anomalous veins that ought to be ligated during surgery for varicocele, go unnoticed and result in recurrence of the varicocele which is regarded as the cause of male infertility [15].
Locale of drainage
Anatomical variations of locale of drainage of testicular veins were found mainly on right side. All the left testicular veins (single or multiple) drain to the renal vein, while the right testicular vein drained to the IVC in more than 83% of cases [4] [Table/Fig-4]. The observation of present study is almost in consonance with earlier workers. Variation encountered in [Table/Fig-1] can be explained on the basis of development of IVC. In this case right supra cardinal vein was replacing sub cardinal, forming a large part of IVC. So, middle part of right sub cardinal in place of forming IVC form right renal vein. Hence right suprarenal vein and right gonadal vein are drained into right renal vein instead of IVC [19]. This anomaly might predispose to varicocele on right side. After detailed research of the literature, a case report by Nayak et al., [20] has been found regarding combination of abnormal termination of the right testicular veins in right renal vein and IVC both, as seen in [Table/Fig-2] of current study. Andreas Vesalius, very early, in 1543, also described an almost similar variation, thus a case of bilateral incompletely double right testicular veins terminated on the right renal vein and IVC and the left testicular vein terminated on the left renal vein and the lower portion of the IVC [21] Nayak et al., [20] suggested that the right testicular vein develops from the lower part of the right sub cardinal vein. The terminal bifurcation of the right testicular vein might be due to the bifurcation of the right sub cardinal vein, during its development. Functionally this variation might cause confusions in assessing the radiological findings or during retroperitoneal surgeries.
The arterio-venous anastomosis between the right testicular vessels is quite rare. In this variation, blood may flow in either direction. If the blood is shunted to the vein from the artery through this anastomosis, it might hinder the upward flow of blood in the vein, resulting in Varicocele. If the blood is shunted from the vein to the artery, that might result in lack of proper oxygen supply to the testis resulting in its decreased function or degeneration [20].
Termination angle
Left gonadal vessels joined the left renal veins at right angle in all the cases, while in 35 (87.5%) of the cases, the right gonadal vein drained in IVC at acute angle and in 5(12.5%) cases, the right testicular vein drained into right renal vein at right angle. Graif et al., [22] hypothesized that flow of blood in the left testicular vein is impaired because it has to make a ‘double 90 degree turn’, before reaching the IVC, whereas on the right side there is direct flow into the IVC. The almost abolished suction effect of the right atrium on the proximal segment of left renal vein has been suggested as an aggravating factor for the stasis in the left pampiniform plexus leading to varicocele.
The above variations may remain silent clinically and unnoticed until discovered during surgery and autopsy and when present, might increase the possibility of varicocele and infertility in patients. Hence, in -depth knowledge of these developmental anomalies of gonadal veins is important.
Dissection picture showing right testicular vein and right supra renal vein draining into right renal vein
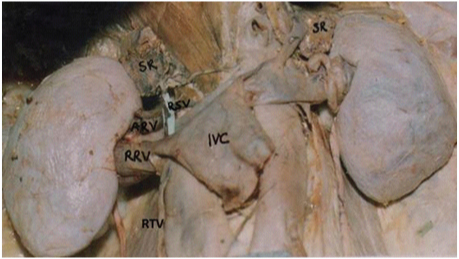
Schematic diagram of [Table/Fig-1a] (IVC- Inferior vena cava, AA- Abdominal aorta, LRV- Left renal vein, RRV- Right renal vein, RSV- Right suprarenal vein, RTV- right testicular vein, LTV- Left testicular vein, SR- Supra renal gland)
Dissection picture showing bifurcated right testicular vein with an arteriovenous anastomosis. Two left testicular veins can also be seen
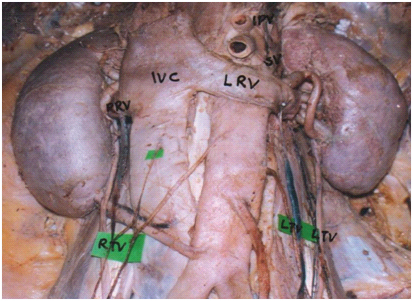
Schematic diagram of picture [Table/Fig-2a] (IVC- Inferior vena cava, AA- Abdominal aorta, LRV- Left renal vein, RRV- Right renal vein, RTV- right testicular vein, LTV- Left testicular vein, TA-Testicular artery, LK- Left kidney, RK- Right kidney)
| RT Testicular Vein | LT Testicular Vein |
|---|
| Single | Double | Single | Double |
|---|
| Lechter et al., [14] | 75% | | 60% | |
| Asala et al., [12] | 96% | 4% | 85% | 15% |
| Favorito et al., [2] | 85% | 5% | 82% | 18% |
| Present study (2014) | 95% | 5% | 70% | 30% |
Locale of drainage of right gonadal vein
| IVC | RRV | BOTH |
|---|
| Pick and Anson [16] | 76.1% | 15% | 6.7% |
| Anson et al., [17] | 78.3% | 22.% | - |
| Asala et al., [12] | 98.7% | 1.3% | - |
| Sharmistha et al., [18] | 95.8% | 4.2% | - |
| Present study (2014) | 85.0% | 10% | 5.0% |
Conclusion
The incidence of anatomical variation of gonadal veins has been observed in this study. Occurrence of variations of gonadal veins was found to be common in males and mostly on the left side. In view of the practical importance of such variations in renal transplantation, renal and gonadal surgeries, and other therapeutic and diagnostic procedures, the present study is quite significant surgically and radiologically.
[1]. M Veeramani, V Jain, A Ganpule, RB Sabnis, MR Desai, Donor gonadal vein reconstruction for extension of the transected renal vessels in living renal transplantationIndian J Urol 2010 26(2):314-16. [Google Scholar]
[2]. LA Favorito, WS Costa, FJ Sampaio, Applied Anatomic Study of Testicular Veins in Adult Cadavers and in Human FetusesInt Braz J Urol 2007 33(2):176-80. [Google Scholar]
[3]. M Itoh, H Moriyama, Y Tokunaga, K Miyamoto, W Nagata, I Satriotomo, Embryological consideration of drainage of the left testicular vein into the ipsilateral renal vein: analysis of cases of a double inferior vena cavaInt J Androl 2001 24(3):142-52. [Google Scholar]
[4]. K Devrim, K Musturay, K Deniz, A Deniz, O Mustafa, MDCT of the Ovarian Vein: Normal Anatomy and PathologyAJR 2009 192(1):295-99. [Google Scholar]
[5]. GJ Romanes , Cunningham, manual of practical anatomy abdomen 2000 15th EditionNew YorkTokyo: Oxford University press:142-53. [Google Scholar]
[6]. Dhar Pushpa, Lal Kumud, Main and accessory renal arteries – A morphological studyJ Anat Embryol 2005 110:101–10-10. [Google Scholar]
[7]. RA Brohi, MF Sargon, N Yener, High origin and unusual suprarenal branch of a testicular arterySurg Radiol Anat 2001 23:207-08. [Google Scholar]
[8]. Sharma Punita, Salwan Surinder Kumar, Anomalous right testicular artery and vein: embryologic explanation and clinical implicationsJournal of Clinical and Diagnostic Research 2011 5(1):1631-33. [Google Scholar]
[9]. P Vijisha, N Muganthan, JR Devi, J Anbalagan, A study of renal vein and gonadal vein variationsNJCA 2012 3(1):125-28. [Google Scholar]
[10]. U Rudloff, RJ Holmes, JT Prem, GR Faust, R Moldwin, D Siegel, Mesoaortic compression of the left renal vein (nutcracker syndrome): case reports and review of the literatureAnn Vasc Surg 2006 20(1):120-29. [Google Scholar]
[11]. P Sharma, SK Salwan, Anomalous Right Testicular Artery and VeinJ Clin Diagn Res 2011 5(8):1631-33. [Google Scholar]
[12]. S Asala, SC Chaudhary, N Masumbuko-Kahamba, M Bidmos, Anatomical variations in the human testicular blood vesselsAnn Anat 2001 183(6):545-49. [Google Scholar]
[13]. P Duques, JR Rodrigues, FB Silva Neto, EMVS Neto, ES Toledo, Estudo anatômico da veia renal esquerda de cadavers humanos brasileirosMedicina Ribeirão Preto 2002 35:184-91. [Google Scholar]
[14]. A Lechter, G Lopez, C Martinez, J Camacho, Anatomy of the gonadal veins: a reappraisalSurgery 1991 109(6):7335-39. [Google Scholar]
[15]. RS Tubbs, ES Salter, WJ Oakes, Unusual drainage of the testicular veinsClin Anat 2005 18:536-39. [Google Scholar]
[16]. JW Pick, BJ Anson, The renal vascular pedicle: Anatomical study of 430 body halvesJ Urol Balt 1940 44:411-34. [Google Scholar]
[17]. BJ Anson, EW Cauldwell, JW Pick, LE Beaton, Anatomy of the pararenal system of vein, with comment on the renal arteryJ Urol 1948 60(5):714-37. [Google Scholar]
[18]. B Sharmistha, JC Chattopadhayay, H Panicker, J Anbalagan, SK Ghosh, Variations in renal and testicular veins- A case reportJ Anat Soc India 2006 55(2):69-71. [Google Scholar]
[19]. S Vettivel, A Mansingh, S Abraham, T Indrasingh, G Chandi, A rare variation in the drainage of right supra renal and gonadal veins into right renal vein; a case reportJ Anat Soc Ind 1998 4(2):76-79. [Google Scholar]
[20]. BS Nayak, KGM Rao, SD Shetty, SR Sirasanagandla, N Kumar, A Guru, Terminal Bifurcation of the Right Testicular Vein and Left Testicular Arterio-Venous AnastomosisKathmandu Univ Med J 2013 42(2):168-70. [Google Scholar]
[21]. GK Paraskevas, O Ioannidis, A Raikos, B Papaziogas, K Natsis, I Spyridakis, High origin of a testicular artery: a case report and review of the literatureJ Med Case Reports 2011 23(5):75 [Google Scholar]
[22]. M Graif, R Hauser, A Hirshebein, A Botchan, A Kessler, H Yabetz, Varicocele and the Testicular–Renal Venous Route: Hemodynamic Doppler Sonographic InvestigationJ Ultrasound Med 2000 19:627-31. [Google Scholar]