Non-Functional Paraganglioma of Retroperitoneum Mimicking Pancreatic Mass with Concurrent Urinary Bladder Paraganglioma: An Extremely Rare Entity
Ankur Verma1, Diwakar Pandey2, Azaz Akhtar3, Ashish Arsia4, Nain Singh5
1 Senior Resident, Department of Surgery, Lady Harding Medical College and SSKH, New Delhi, India.
2 Post graduate student, Department of Surgery, Lady Harding Medical College and SSKH, New Delhi, India.
3 Assistant Professor, Department of Surgery, Lady Harding Medical College and SSKH, New Delhi, India.
4 Associate Professor, Department of Surgery, Lady Harding Medical College and SSKH, New Delhi, India.
5 Associate Professor, Department of Surgery, Lady Harding Medical College and SSKH, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Mr. Diwakar Pandey, HSB 320, Lady Hardinge Medical College and SSKH, Shaheed Bhagat Singh Marg, New Delhi -110001, India.
E-mail: drdiwakarpandey86@gmail.com
Paragangliomas are extra-adrenal tumours of the autonomic nervous system, which rarely present as primary retroperitoneal mass mimicking pancreatic malignancy (incidence 2-8 per million populations). Urinary Bladder Paraganglioma are also extremely rare (0.06% of all Bladder Tumour and 6% of Paragangliomas) with most being malignant and high grade tumours. Non-functional varieties of both tumours are usually incidentally diagnosed. The possibility for malignant transformation in them makes surgical excision the treatment of choice. A 45-year-old lady with abdominal pain was investigated to have a complex retroperitoneal mass behind head of pancreas and a urinary bladder mass. Complete excision of retroperitoneal and bladder lesion was done. Histopathological examinations of both specimens were suggestive of Paraganglioma with no abnormal mitotic activity and capsular/vascular invasion. Although concurrent non functional paragangliomas had been reported but the synchronous non-functional paragangliomas of retroperitoneum and urinary bladder reported in this case is extremely rare and is not reported so far in English literature.
Excision, Pancreas, Retroperitoneal mass, Synchronous
Case Report
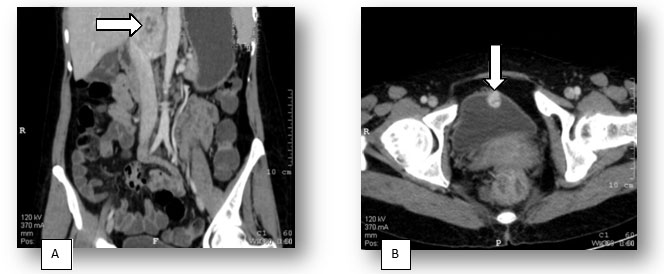
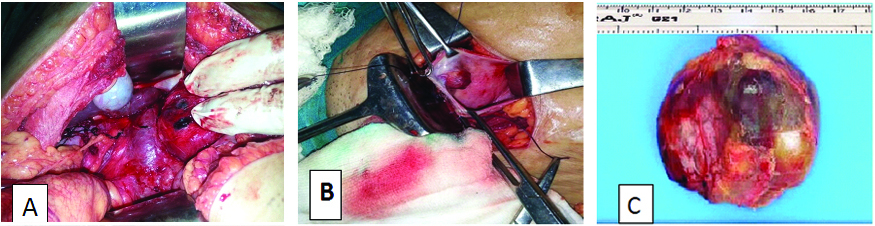
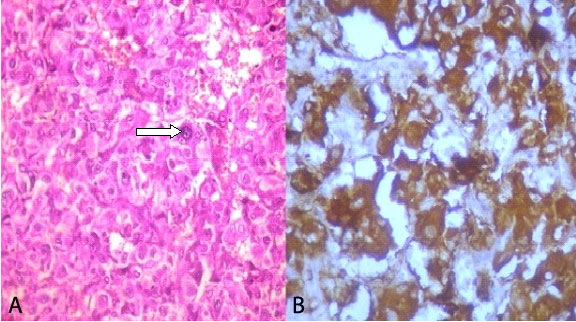
A 45-year-old lady presented with pain in central abdomen and occasional headaches for 2 years. Her family history was unremarkable and she had no previous medical and urinary problem. General and systemic examination was normal. On ultrasound abdomen 6 x 6 cm solid iso-echoic lesion was seen in the retroperitoneum abutting periportal and peripancreatic region displacing hepatic artery and portal vein anteriorly [Table/Fig-1]. CECT abdomen demonstrated 6.5 x 5.4 cm well capsulated lesion in portocaval region with increased enhancement in arterial phase and relative washout in porto-venous phase with central necrotic areas. The portal vein and head of pancreas were displaced anteriorly with no evidence of calcification and metastases [Table/Fig-2a,b]. A 2 x 1.5 cm similar enhancing lesion in anterior bladder wall was present. Urinary metanephrines were normal. Patient underwent cystoscopy and revealed 2 x 2 cm highly vascular lesion in the anterior wall of urinary bladder with normal mucous covering. During exploratory laparotomy a single 6 x 6 cm solid highly vascular mass was seen in the aorto-caval groove without regional lymphadenopathy. Inferior vena cava was compressed with anterior displacement of portal vein and head of pancreas but no invasion into surrounding structures [Table/Fig-3a-c]. Complete excision of retroperitoneal and bladder lesion was done. There was no preoperative or intraoperative fluctuation of blood pressure. Pathological evaluation revealed paraganglioma to be the final diagnosis with no abnormal mitotic activity and capsular/vascular Invasion [Table/Fig-4a,b].
Ultrasound abdomen showing retroperitoneal mass abutting peri portal and peri pancreatic region (arrow head),

CECT Abdomen (A) coronal section showing the mass sandwiched between the great vessels, (B) axial view, showing urinary bladder mass (arrow heads)
Intraoperative findings (A) Retroperitoneal mass sandwiched between great vessels, (B) Urinary bladder mass, (C) Gross specimen of retroperitoneal mass
(A) Large tumour cell with granular eosinophilic cytoplasm, nests of capillary and nuclear pleomorphism or bizarre nuclei (arrow head) (H&E 400), (B) Immuohistochemical study demonstrating strong expression of chromogranin A and synaptophysin, but negative for cytokeratin
Discussion
Paragangliomas are extra-adrenal chromaffin [1] tumours that develop from the neuroectodermal cells of the autonomous nervous system. Closely related tumours in extra-adrenal sympathetic and parasympathetic paraganglia are classified as extra-adrenal paragangliomas [2,3]. Middle aged men and women were equally affected in most series [4]. Genetic mutation in genes encoding succinate dehydrogenase enzyme had also been observed [5]. Patients with non-functioning retroperitoneal paraganglioma are usually rare and asymptomatic until the tumour reaches sufficient size to produce symptoms of compression of adjacent organs [6]. Paragangliomas of the urinary bladder account for 0.06% of all bladder tumours and 6% of extra-adrenal pheochromocytomas with most being high grade and functional in contrast to their retroperitoneal counterparts [7]. Because of low incidence rate, the prognosis of paraganglioma is not well established. Occasionally these tumours are multiple and may be associated with paraganglioma of other sites or with other tumours [3]. Typical symptoms include abdominal pain in 50% of cases (as in our case), nausea, emesis, abdominal distension and weight loss. Functional excretion of metabolites and increased vascularity causes haematuria and other classical symptoms like headache, blurred vision and palpitation especially during micturation. MRI is more sensitive than CT scan in detecting extra-adrenal tumours. Scintigraphy with I-123 labelled MIBG offers superior specificity than CT and MRI [8,9]. Immunohistochemically, neuron-specific enolase (NSE), synaptophysin, neurofilament protein and chromogranin can be demonstrated in the chief cells of paraganglioma. In addition, the delicate sustentacular network can be demonstrated using antibodies to S-100 protein and in a few instances these same cells coexpress glial fibrillary acidic protein. Paragangliomas metastasize approximately in 20% to 42% of the cases. Dissemination can be haematogenous or through the lymphatic system with most common site being the regional lymph nodes, bone, lung and liver. Thus, the possibility for malignant transformation or metastasis of Paragangliomas makes surgical excision the treatment of choice. Surgical therapy includes open or laparoscopic excision for retroperitoneal tumours, transurethral resection and partial or total cystectomy combined with pelvic lymph node dissection, especially in the presence of metastasis for urinary bladder paraganglioma [10]. Radiation therapy has been advocated in patients where surgery is not feasible or for unresectable tumours [11]. Therapy with radionucleotides (I-131 MIBG) or combination chemotherapy (cyclophosphamide, vincristine and darcabazine) may induce partial responses to malignant paraganglioma [12]. Octreotide may also be used for treatment of inoperable paragangliomas [13]. Although multiple functional and non functional Paragangliomas had been reported [2,5,14], synchronous non functional paragangliomas of retroperitoneum and urinary bladder reported in this case is extremely rare and is not found to be reported after extensive journal search. Complete surgical excision of both the lesions was performed and patient recovered well.
Conclusion
This case is unique in terms of having two rare synchronous non-functional paraganglioma in retroperitoneum and urinary bladder without any clinical symptoms and to best of our knowledge till date it remains first ever such reported case in literature worldwide. Our case emphasizes the necessity to include extra-adrenal paraganglioma in the differential diagnosis and management of retroperitoneal tumours including pancreatic mass, despite its rarity, with thorough metastatic workup to pickup synchronous or metachronous lesions in other organs. Imaging studies have greatly contributed to a more accurate diagnosis of paraganglioma. Yet, the gold standard for diagnosis remains a pathological one. Lifelong follow-up of patients with retroperitoneal Paragangliomas is essential as silent metastasis and recurrence may occur frequently.
[1]. Lamblin A, Pigny P, Tex G, Rouaix-Emery N, Porchet N, Leteurtre E, [Paragangliomas: clinical and secretory profile. Result of 39 cases]Ann Chir 2005 130(3):157-61. [Google Scholar]
[2]. Whalen RK, Althausen AF, Daniels GH, Extra-adrenal pheochromocytomaJ Urol 1992 147(1):1-10. [Google Scholar]
[3]. Kimura N, Capella C, De Krijger RR, Thompson LDR, Lam KY, Komminoth P, Extra-adrenal symphathetic paraganglioma: Superior and inferior paraaorticIn World Health Organization Classification of Tumours, Tumours of Endocrine Organs. Edited by DeLellis RA, Lloyd RV, Heitz PU, Eng C 2004a Lyon, FranceIARC Press:164-165. [Google Scholar]
[4]. Wen J, Li HZ, Ji ZG, Mao QZ, Shi BB, Yan WG, A case of large silent extra-adrenal retroperitoneal paraganglioma resected laparoscopicallyChin Med Sci J 2010 25(1):61-64. [Google Scholar]
[5]. Vandy FC, Sisk G, Berguer R, Synchronous carotid body and thoracic paraganglioma associated with a germline SDHC mutationJ Vasc Surg 2011 53(3):805-07. [Google Scholar]
[6]. Crozier F, Lechevallier E, Eghazarian C, André M, Sammama D, Wilshire P, Retroperitoneal non-secreting paragangliomaJ Radiol 1999 80:150-52. [Google Scholar]
[7]. Leestma JE, Price EB Jr, Paraganglioma of the urinary bladderCancer 1971 28(4):1063-73. [Google Scholar]
[8]. Mhanna T, Pianta E, Bernard P, Hervieu V, Partensky C, Preaorticparaganglioma mimicking a hypervascular tumor of the pancreasHepato-Gastroenterology 2004 51(58):1198-201. [Google Scholar]
[9]. Rha SE, Byun JY, Jung SE, Chun HJ, Lee HG, Lee JM, Neurogenic tumors in the abdomen: Tumor types and imaging characteristicsRadiographics 2003 23(1):29-43. [Google Scholar]
[10]. Thrasher JB, Rajan RR, Perez LM, Humphrey PA, Anderson EE, Pheochromocytoma of urinary bladder: contemporary methods of diagnosis and treatment optionsUrology 1993 41(5):435-39. [Google Scholar]
[11]. Yang JH, Bae SJ, Park S, Park HK, Jung HS, Chung JH, Bilateral pheochromocytoma associated with paraganglioma and papillary thyroid carcinoma: report of an unusual caseEndocrine Journal 2007 54(2):227-31. [Google Scholar]
[12]. Fitzgerald PA, Goldsby RE, Huberty JP, Price DC, Hawkins RA, Veatch JJ, Malignant pheochromocytomas and paragangliomas: a phase II study of therapy with high-dose 131Imetaiodobenzylguanidine (131I-MIBG)Ann N Y Acad Sci 2006 1073:465-90. [Google Scholar]
[13]. Tonyukuk V, Emral R, Temizkan S, Sertçelik A, Erden I, Corapçio Lu D, Patient with multiple paraganglioma treated with long acting somatostatin analogueEndocrine Journal 2003 50:507-13. [Google Scholar]
[14]. Limani K, Velthoven RV, Aoun F, Bi-Focal Retroperitoneal Paraganglioma in a Young Patient: A Case Report and Review of the LiteratureMed Surg Urol 2014 3(1):127 [Google Scholar]