Introduction: To evaluate the association of high myopia with retinal nerve fibre layer (RNFL) thickness by Fourier domain optical coherence tomography (FD OCT).
Materials and Methods: Fifty highly myopic eyes (25 patients) and forty emmetropic eyes (20 Normal subject) were randomly selected after excluding concomitant ophthalmic disorder and RNFL thickness measured using the Fourier domain optical coherence tomography (FD OCT).
Results: The overall mean RNFL thickness in the myopic groups and control were 87.89 μm and 111.64 μm respectively. The mean retinal nerve fibre thickness was significantly less in myopic eyes as compared to control group (p =0.0001). Retinal nerve fibre layer thickness shows topographic double hump pattern in both the groups (myopes and emmetropes).
Conclusion: Retinal nerve fibre thickness was significantly less in myopic eyes as compared to emmetropic eyes. The retinal nerve fibre layer thinning in high myopes may be confused with open angle glaucoma, a disease also prevalent in high myopes. There is therefore a need to have retinal nerve fibre layer thickness normogram for high myopes of a given population group to avoid wrong interpretation.
Introduction
Myopia, a form of refractive error is a leading cause of visual disability throughout the world. In India uncorrected refractive errors are the most common cause of visual impairment and second major cause of avoidable blindness. The prevalence of myopia varies by the country, age and by ethnic group it is a major cause of visual impairment in both the developed and the developing world. The prevalence of myopia has been reported to be as high as 70-90% in some Asian population like Taiwan. The survey conducted in India in the 1970's by Jain et al., has shown a prevalence of myopia of 4.79% among the school children. It was higher in urban population (6.9%) in comparison to rural population (2.77%). Recent literatures show overall prevalence of myopia in India is 34.6% [1] . Few studies have evaluated possible structural changes in the retina in individuals with moderate to high myopia without clinically overt retinal disease. Eyes with refractive error -6D or more are said to be high myopia [2,3] . The histopathological changes that accompany high myopia are well documented [4-6] . Contrary to histologic findings and clinical observations that retinal thinning or chorioretinal atrophy is more common in myopia [7-9] . The correlation between average macular thickness and myopia has been found to be insignificant in previous in vivo imaging (nerve fibre analyser) studies [10,11] .
Since its introduction in 1991 by Huang et al., [12] the optical coherence tomography (OCT use) is widely used modality for assessing the fovea and peripapillary nerve fibre layer in diseases like macular edema, central serous retinopathy, clinically significant macular edema (CSME) in diabetes, wet age related macular degeneration, traumatic macular involvement, macular and non macular retinoschisis, retinal detachment, optic atrophy and chronic glaucomas. The optical coherence tomography is a non invasive imaging technology, which needs no direct contact with the eye. It is analogous to the B-scan of the ultrasonograph, where light beams used instead of sound waves. Time difference in reflected light from each part of the tissue is measured using optical interferometer [4] . The high myopia and concomitant glaucoma are associated with retinal changes which were extensively studied. Retinal changes in isolated high myopia is still unclear and this emphasize us to detect changes in the RNFL accurately even in early stage.
The present study aims to collect the normographic data of high myopes of ≥ 6D with respect to thickness of nerve fibre layer, so as to interprets and distinguish the physiological changes of high myopia from accompanying diseases in such individuals.
Materials and Methods
After obtaining clearance from Institutional ethics committee, the present study was carried out randomly selected subjects from the outpatient department of eye and Retina Clinic, Institute of Ophthalmology on the basis of routine ophthalmic examination. An informed written consent was taken from each subject. Subjects were matched for age, sex, height and weight. Using the Snellen chart, vision was measured. The same experimenter measured the intraocular pressure three times in each eye with the Goldmann tonometer. The refractive error from the manifest refraction (MR) was adjusted to the spherical equivalent. The visual field was measured using the Humphrey field analyzer, with the central 30-2 SITA-standard program. Every patient was instilled with a drop of 1% tropicamide and 2.5% phenylephrine hydrochloride in each eye 3 times at 15 minute intervals to dilate the pupil. A dilated fundus examination was precisely performed in all subjects
Subjects were divided into two groups: Group I- patients with both high myopic (≥6 D) eyes and Group II- subjects with both emmetropic eyes. For Group I, inclusion criteria were: Patients with myopia of ≥ 6D, Intraocular pressure < 21mm Hg OU, No glaucomatous changes such as disc haemorrhages and glaucomatous cupping e.g. vertical cup-disc ratio>0.7. media opacities, astigmatism up to 2D. Exclusion criteria were: glaucoma, refractive surgery, neurological disease, diabetes mellitus, hypertension and any other systemic illness. For Group II inclusion criteria were BCVA Of 6/6 or 20/20, Intraocular pressure <21 mm Hg and exclusion criteria were Ocular surgery and apparent pathologies.
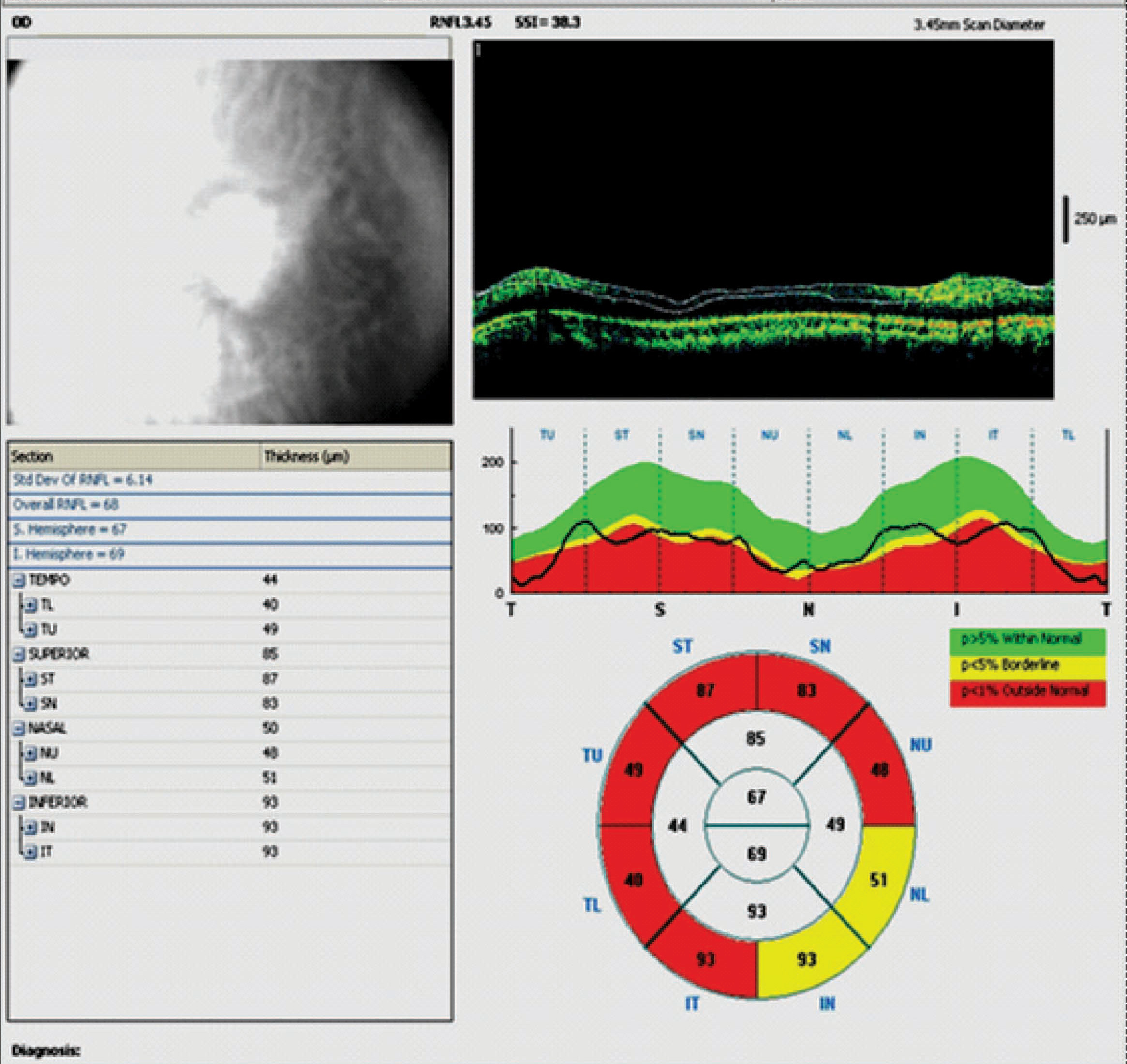
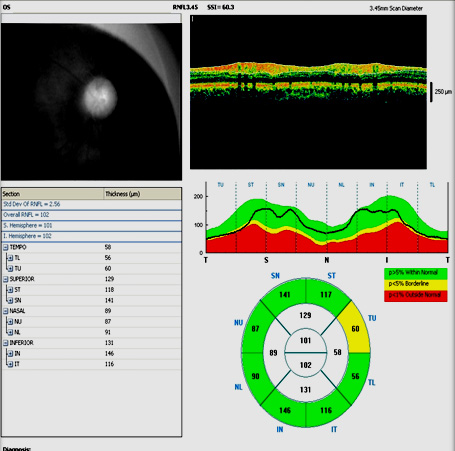
Total 50 high myopic eyes and 40 emmetropic eyes were considered. Following pupillary dilation at least 5mm with 0.5% cyclopentolate solution, Fourier domain optical coherence tomography (fast thickness scan) was used to examine the eyes. Three circular scans were obtained at the peripapillary retina at a default radius of 1.74 mm from the centre of the optic disc, and the measurements were averaged to provide the average peripapillary RNFL thickness. In addition, the peripapillary scan was divided into four equal 90 degree quadrants (superior, inferior, temporal, nasal) and RNFL thickness measurements in these four quadrants were also provided [Table/Fig-1],Table/Fig-2]. In case of astigmatism upto 2D was included and its spherical equivalent added before OCT.
Analysis of the collected data was done using SPSS version 20. Significance of difference of RNFL between myopic (Group I) and emmetropic (Group II) were determined by using unpaired t-test and quadrantic comparison by paired t-test. P-value ≤ 0.05 was considered statistically significant.
Results
In the present study, 50 eyes of high myopic and 40 eyes of emmetropic subjects were enrolled. In both groups age of subjects varied from 11 to 40 y. The mean spherical equivalent (SE) of refractive errors of myopes (Group I) was -10.48 ±03.08 D and range -6.5 to -18 D.
In our study, overall mean RNFL thickness in study group (Group I) was 87.89 μm and in control group (Group II) was 111.64 μm [Table/Fig-3]. The mean retinal nerve fibre thickness was significantly less in myopic eyes (Group I) as compared to control group (Group II). In all the quadrants Retinal nerve fibre thickness was significantly decreased in myopic eyes (Group I) as compared to emmetropic eyes (Group II) [Table/Fig-3].
Quadrantic comparison within group (on PAIRED t-TEST): In group I (myopic eyes) retinal nerve fibre layer thickness in superior quadrant was observed to be the thickest and in nasal quadrant was the thinnest. However, the intragroup comparison was statistically insignificant except when superior quadrant was compared with nasal quadrant (on paired t-test).
In Group II (emmetropic eyes) retinal nerve layer thickness in inferior quadrant was thickest and temporal quadrant was thinnest, and intragroup comparison was statistically highly significant (p-value <0.0001) when superior quadrant was compared with nasal and inferior, and inferior quadrant was compared with nasal quadrant.
Discussion
Average RNFL thickness in myopia is debatable. Our study showed a mean RNFL thickness of 111.64 μm in emmetropic subjects. Parvaresh et al., measured the mean RNFL in Iranian population was 131.12 μm and in Turkish population mean RNFL was 125.9 μm measured by Oner et al., [13,14]. The RNFL was thickest in the inferior and superior quadrants, which is consistent with previous studies. Reported range of RNFL thickness in emmetropic subjects is 86 to 130.5 μm which is consistent with our finding [13].
In Schumann [15] and Bowd [16] reports a difference and was found between the nasal and temporal RNFL thickness, with the nasal quadrant thinner than the temporal quadrant. But, in our study the temporal RNFL thickness was thinner than that of the nasal quadrant (p<0.0001). These observations are supported by previous study by Parvaresh et al., [13] and histological data. Indeed, histological measurements of the thickness of the RNFL in normal eyes demonstrate that superior, inferior, and nasal quadrant RNFL at the disc margin are significantly thicker than the temporal quadrant RNFL at the disc margin. It is possible that this results from subtle differences in axon trajectory away from the optic nerve head (ONH) and emphasizes the importance of eccentricity when comparing RNFL thickness around the ONH [17,18] The difference between these two studies can be related to population characteristics, and the measurement technique.
In study of Mrugacz et al., [17] the mean NFL thickness was 152 μm in eyes with low myopia (-1.0 to -4.0 D), 150 μm in eyes with medium myopia (-4.0 to -8.0 (D)) and 140 in eyes with high-myopia (> -8.0 D). Statistically significant differences were revealed between patients with high-myopia and the control group. Parveresh et al., measured the RNFL thickness in high myope in Iranian population was 107.94 μm [13]. Leung et al., measured the Mean RNFL thickness in Chinese population was 90.46 μm [4]. We measured average RNFL thickness in high-myopic groups 87.89 μm which was significantly different with emmetrope eyes. The difference of RNFL thickness values between Mrugacz et al., [17] study and ours can be explained by the fact that mean age in their study was 15-year-old and in our study was 23.76 y (in Leung et al., 32 y and in Pervaresh et al., 24.5 y) and also due to racial or ethinic differences. On the other hand, Alamouti et al., [18] found that older individuals had thinner RNFL than younger individuals, so the lower RNFL thickness values in our study may be attributed to older patients’ age. Above findings are also similar to our finding. But in study of Sek-Tien Hoh found mean peripapillary RNFL thickness did not correlate with SE in myopic eyes [3]. In Mrugacz et al., [17] series the different groups were categorized according to the subjects’ refraction regardless of their AL. So, the cases in high-myopic groups could be within normal AL with subsequent higher RNFL thickness.
In Parvaresh et al., study, there was a strong negative correlation correlation between RNFL thickness and AL (r -0.91, p 0.003) could be explained by the fact that the number of axons which forms the RNFL is equal and not proportional to AL. On the other hand larger AL causes larger surface area and distribution of an equal amount of retinal nerves in larger area, causes a thinner layer. We did not measured the axial length so unable to correlate which is existing lacuna of our study.
Our study found significant differences in the peripapillary RNFL thickness in four quadrants. This present study has demonstrated that the eyes of myopic adults, who had otherwise healthy ocular status have less RNFL thickness. Retinal nerve fibre layer thickness shows double hump pattern in both the groups (myopes and emmetropes). This is similar to previous literature reported by Lee et al., and Leung et al., [19,20]. Our results also showed the characteristic‘ double hump pattern’ of the normal eye, where the superior and inferior retinal nerve fibre layer were thickest. Emmetropic eyes are consistently spherical but myopic eyes demonstrated symmetrical or asymmetrical anteroposterior elongation and posterior protrusions. The distribution of the RNFL bundles conforms to the shape of the globe which lead to double hump pattern.
RNFL thickness scan of myopic eye
RNFL thickness scan of emmetropic eye
Retinal nerve fibre thickness in Group I (Myopia) and Group II (Emmetropia)
| RNFL Thickness | Group I Mean±SD (μm) | Group II Mean±SD (μm) | 95% CI (μm) | p-value |
|---|
| Average | 87.89±10.37 | 111.64±12.6 | -28.59 to -18.91 | =0.00001 |
| Temporal | 70.06±14.13 | 81.30 ±10.51 | -16.57 to -05.90 | =0.000068 |
| Superior | 109.47±19.83 | 137 ±23.64 | -36.63 to -18.42 | =0.00001 |
| Nasal | 67.06±17.37 | 86.80 ±14.95 | -26.63 to -12.85 | =0.00001 |
| Inferior | 104.74±14.05 | 141.5±19.63 | -43.81 to -29.68 | =0.00001 |
Conclusion
In this study, measurement of the RNFL thickness was significantly affected by spherical errors and temporal deviation of the RNFL thickness profile was observed. Thus, in myopic subjects, the measured RNFL thickness may be less than the actual thickness, and owing to the temporal shift in the contour of the RNFL thickness profile, the superior and inferior RNFLs may be deemed abnormal in comparison with the normative reference provided by FD-OCT. The current normative database may be misleading for a correct diagnosis of glaucoma in varying degrees of myopia. To make a correct diagnosis, either the axial length-induced magnification effect should corrected by ophthalmologists or the current FD OCT database should be improved by taking axial length into account.
[1]. IS Jain, S Jain, K Mohan, The epidemiology of high myopia—changing trendsIndian journal of Ophthalmology 1983 31(6):723-28. [Google Scholar]
[2]. MC Lim, S Hoh, PJ Foster, Use of optical coherence tomography to assess variations in macular retinal thickness in myopiaInvest Ophthalmol Vis Sci 2005 46:974-78. [Google Scholar]
[3]. T Ho, Y Shih, S Lin, LL Lin, M Chen, Peculiar arcuate scotoma in pathologic myopia-optical coherence tomography to detect peripapillary neural tissue loss over the disc crescentGraefes Arch Clin Exp Ophthalmol 2005 243:689-94. [Google Scholar]
[4]. CK Leung, S Mohamed, KS Leung, Retinal nerve fiber layer measurements in myopia: an optical coherence tomography studyInvest Ophthalmol Vis Sci 2006 47:5171-76. [Google Scholar]
[5]. S Choi, S Lee, Thickness changes in the fovea and peripapillary retinal nerve fiber layer depend on the degree of myopiaKorean J Ophthalmol 2006 20:215-19. [Google Scholar]
[6]. S Hoh, MC Lim, SK Seah, Peripapillary retinal nerve fiber layer thickness variations with myopiaOphthalmology 2006 113:773-77. [Google Scholar]
[7]. M Yanoff, BS Fine, Ocular Pathology: A Text and AtlasTetracyclineTeratology 1982 Row Philadelphia:513-514. [Google Scholar]
[8]. WH Spencer, Ophthalmic Pathology: an Atlas and Textbook 1985 3rd EditionWB Saunders Philadelphia:395-400. [Google Scholar]
[9]. BJ Curtin, DB Karlin, Axial length measurements and fundus changes of the myopic eyeTrans Am Ophthalmol Soc 1970 68:312-34. [Google Scholar]
[10]. Y Wakitani, M Sasoh, M Sugimoto, Macular thickness measurements in healthy subjects with different axial lengths using optical coherence tomographyRetina 2003 23:177-82. [Google Scholar]
[11]. H Zou, X Zhang, X Xu, Quantitative in vivo retinal thickness measurement in Chinese healthy subjects with the retinal thickness analyzerInvest Ophthalmol Vis Sci 2006 47:341-47. [Google Scholar]
[12]. D Huang, EA Swanson, CP Lin, Optical coherence tomographyScience 1991 254:1178-81. [Google Scholar]
[13]. MM Parvaresh, M Imani, M Bahmani-Kashkouli, M Soltan-Sanjari, Optical Coherence Tomography-Measured Nerve Fiber Layer and Macular Thickness in Emmetropic, High-Myopic and High-Hyperopic EyesIranian Journal of Ophthalmology 2008 20(2):4-9. [Google Scholar]
[14]. V Oner, V Aykut, M Tas, MF Alakus, Y Iscan, Effect of refractive status on peripapillary retinal nerve fibre layer thickness: a study by RTVue spectral domain optical coherence tomographyCurrent Eye res 2013 38:1241-47. [Google Scholar]
[15]. JS Schumann, MR Hee, CA Puliofito, Quantification of nerve fiber layer thickness in normal and glaucomatous eyes using optical coherence tomographyArch Ophthalmol 1995 113(5):586-96. [Google Scholar]
[16]. C Bowd, RN Weinreb, JM Williams, LM Zangwill, The retinal nerve fiber layer thickness in ocular hypertensive, normal and glaucomatous eyes with optical coherence tomographyArch Ophthalmol 2000 118:22-26. [Google Scholar]
[17]. M Mrugacz, A Bakunowicz-Lazarczyk, D Sredzinska-Kita, Use of optical coherence tomography in myopiaJ Pediatr Ophthalmol Strabismus 2004 41:159-62. [Google Scholar]
[18]. B Alamouti, J Funk, Retinal thickness decreases with age: an OCT studyBr J Ophthalmol 2003 87:899-901. [Google Scholar]
[19]. JH Lee, CS Ahn, DY Lee, Qauntification of retinal nerve fiber layer thickness in the normal subjects using optical coherence tomographyJ Korean Ophthalmol Soc 1999 40:2804-15. [Google Scholar]
[20]. CK Leung, M Yu, RN Weinren, HK Mak, G Lai, C Ye, Retinal Nerve Fiber Layer Imaging with Spectral-Domain Optical Coherence Tomography: Interpreting the RNFL Maps in Healthy Myopic EyesInvest Ophthalmol Vis Sci 2012 53:7194-200. [Google Scholar]