In Vitro Fractional Inhibitory Concentration (FIC) Study of Cefixime and Azithromycin Fixed Dose Combination (FDC) Against Respiratory Clinical Isolates
Saiprasad Vilas Patil1, Anoop Laxminarayan Hajare2, Manjusha Patankar3, K Krishnaprasad4
1 Assistant Manager, Medical Services, Glenmark Pharmaceuticals Ltd, Andheri(E). Mumbai, India.
2 Assistant Manager, Medical Services, Glenmark Pharmaceuticals Ltd, Andheri(E). Mumbai, India.
3 Lecturer, Department of Pharmacology, D.Y. Patil Medical College, Navi Mumbai, India.
4 Deputy General Manager, Medical Services, Glenmark Pharmaceuticals Ltd, Andheri(E). Mumbai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anoop Laxminarayan Hajare, Glenmark Pharmaceuticals Ltd, Corporate Enclave, B.D. Sawant Marg, Chakala, Andheri(E). Mumbai - 400099, India. E-mail : anoophajare@gmail.com
Introduction: Acute respiratory infections (ARI) contribute to more than 75% of health care seeking in primary health care facilities in India. Respiratory tract infections (RTIs) are managed frequently by β-lactam, macrolide and fluroquinolone class of antibiotics. However, these recommended classes of antibiotic have shown resistance in community settings. Antibiotic combinations may provide broader spectrum not only in terms of coverage but also to overcome multiple resistance mechanisms overcoming individual class limitations.
Aim: The study aimed to determine In vitro interactions interpreted according to calculated fractional inhibitory concentration (FIC) index between cefixime and azithromycin against common respiratory clinical isolates.
Materials and Methods: Forty four bacterial respiratory clinical isolates from microbiology department of tertiary care hospital from Mumbai were used to determine the minimum inhibitory concentration (MIC) values of cefixime and azithromycin. Synergy testing of cefixime combination with azithromycin was performed by checkerboard method. Interaction was determined according to calculated FIC index.
Results: MIC values were ranging from 2–128 μg/ml and 0.24–128 μg/ml for cefixime and azithromycin respectively against K.pneumoniae, M.catarrhalis, S.pneumoniae and H.influenzae isolates. All the tested isolates were resistant to cefixime. Azithromycin resistance was noted in all the isolates except six M. catarrhalis isolates. FIC index showed synergy and additive effect in 66% (29/44) and 34% (15/44) all bacterial clinical isolates. Maximum synergy between cefixime and azithromycin was observed against K. pneumoniae in 91% isolates.
Conclusion: This is one of the first attempts to check the rationality of fixed dose antibiotic combination of cefixime and azithromycin in India market. Though results of this study cannot be generalized considering the limitations of low sample size and in vitro model, our data provides stepping stone for further validation of cefixime and azithromycin fixed dose combinations (FDCs) in clinical setting by conducting randomized controlled trials. We think that judicious and rational use of FDCs may help to reduce the risk of selection of further drug resistance along with better clinical outcome.
Acute respiratory infections, Fixed dose combination, Fractional inhibitory concentration index, Minimum inhibitory concentration, Synergy
Introduction
Globally, community acquired RTIs account for a large proportion of antibiotic prescriptions and visit to family practitioners [1]. ARIs contribute to more than 75% of health care seeking in primary health care facilities [2]. Majority of ARIs are of viral aetiology, but information from India on various respiratory tract bacterial pathogens and resistance pattern in hospital settings is inadequate [3]. Because of the commonness of the problem, antimicrobial therapy for ARIs is a major predictor for the spread of resistant strains of microbes in the community [2]. In India empiric therapy is often practiced, the tests of antibiotic susceptibility may not be routinely performed in the real life setting [4]. Often, the clinicians resort to clinical pointers of poor response to antibiotics such as lack of effervescence of fever, lack of symptom relief as a guide to estimate the presence of antibiotic resistance.
Lower RTIs particularly community acquired pneumonia (CAP) are common and can be potentially serious. These are managed frequently by β-lactam, macrolide and fluroquinolone class of antibiotics. But resistance towards these class of antibiotics in community settings of India is on rise [5].
Clinicians are increasingly opting for two or more antibiotics as empiric choice to ensure complete clinical cure. Antibiotic combinations are sought to provide synergistic killing, but its impact on the evolution of resistance is unclear. Synergistic interactions are usually thought of as advantageous since, for a given amount of drug, they more effectively inhibit the growth of drug-sensitive pathogens [6].
Antibiotic combinations may provide broader spectrum not only in terms of coverage but also to overcome multiple resistance mechanisms overcoming individual class limitations [Table/Fig-1]. Better clinical outcome of respiratory infections (particularly pneumonia) with antibiotics combination therapy than monotherapy has been documented by several studies [7].
Individual antibiotic class limitation in RTI management
| Class | Limitation |
|---|
| β-lactam | No activity against atypical pathogen and development of S. pneumoniae resistant isolates > 50 % |
| Macrolides | 30.9 % resistant S. pneumoniae isolates reported |
| Fluroquinolones | Increase potential for emergence of resistant strain of gram negative microorganism |
Parameters which have been used to show interactions during combination therapy are the FIC indices, derived from checkerboard titrations [8]. In this study, in vitro synergy between cefixime and azithromycin in Cefixime-azithromycin FDC was investigated by evaluating FIC indices for Haemophilus influenzae, Klebsiella pneumoniae, Moraxella, catarrhalis and Streptococcus pneumoniae respiratory clinical isolates.
MATERIALS AND METHODS
Forty four bacterial respiratory clinical isolates were collected from microbiology department of a tertiary care hospital in Mumbai, These included 11 Haemophilus influenzae, 11 Klebsiella pneumoniae, 11 Moraxellacatarrhalis and 11 Streptococcus pneumoniae. Study period was from June 2014 to August 2014.
The MIC values of cefixime and azithromycin were determined for all 44 bacterial isolates. In order to determine the MICs, ultrapure water was used to dissolve the antibiotics so as to give stock concentrations of 5120 μg/ml. Subsequently, twofold serial dilutions of cefixime and azithromycin were made to give concentrations ranging from 1 to 512 μg/ml. An inoculum of 5 × 105 CFU/ml was obtained by adding 500 μl of 106 CFU/ml bacterial suspension to the sterile capped test tubes. Another 500 μl of cefixime or cefixime and azithromycin combination were pipetted into the tubes. Control was prepared by adding the test bacteria to tube containing inert solvent to dissolve the antibiotics. After overnight incubation at 370C, the tube containing lowest concentration of the antibiotic showing no visible growth was recorded for calculation of MIC. MIC values for isolates were interpreted according to CLSI criteria. Synergy testing of cefixime combination with azithromycin was performed by checkerboard method. Interaction was determined according to calculated FIC index.
Results
MIC values were ranging from 2–128 μg/ml and 0.24–128 μg/ml for cefixime and azithromycin [Table/Fig-2,3,4,5] respectively against K. pneumoniae, M. catarrhalis, S. pneumoniae and H. influenzae isolates. All tested isolates were resistant to cefixime. Azithromycin resistance was noted in all isolates except six M. catarrhalis isolates [Table/Fig-2–5]. Comparison of mean MIC of each bacterial type with cefixime and azithromycin alone and cefixime in combination with azithromycin [Table/Fig-6] showed 4.4, 9.1, 12.8 and 5.8 fold reduction in cefixime MIC in combination against K. pneumoniae, M. catarrhalis, S. pneumoniae and H. influenzae respectively.
MIC values of azithromycin alone and in combination with cefixime for K. pneumoniae
| K. pneumoniae |
|---|
| Strains | MIC Azithromycin | MIC Cefixime | FIC index | Outcome |
|---|
| Alone (μg/ml) | With Cefixime (μg/ml) | Alone (μg/ml) | With Azithromycin (μg/ml) |
|---|
| A1 | 128 | 16 | 64 | 16 | 0.375 | Synergy |
| A2 | 128 | 16 | 64 | 8 | 0.25 | Synergy |
| A3 | 128 | 32 | 64 | 16 | 0.5 | Synergy |
| A4 | 128 | 64 | 64 | 4 | 0.563 | Additive |
| A5 | 128 | 16 | 128 | 32 | 0.375 | Synergy |
| A6 | 128 | 32 | 128 | 32 | 0.5 | Synergy |
| A7 | 64 | 16 | 64 | 16 | 0.5 | Synergy |
| A8 | 64 | 16 | 128 | 32 | 0.5 | Synergy |
| A9 | 128 | 16 | 32 | 8 | 0.5 | Synergy |
| A10 | 256 | 64 | 128 | 32 | 0.5 | Synergy |
| A11 | 128 | 8 | 64 | 16 | 0.313 | Synergy |
MIC values of azithromycin alone and in combination with cefixime for M. Catarrhalis
| M. catarrhalis |
| Strains | MIC Azithromycin | MIC Cefixime | FIC index | Outcome |
| Alone (μg/ml) | With Cefixime (μg/ml) | Alone (μg/ml) | With Azithromycin (μg/ml) |
| A1 | 0.48 | 0.24 | 8 | 1 | 0.375 | Synergy |
| A2 | 0.24 | 0.24 | 8 | 1 | 0.375 | Synergy |
| A3 | 0.48 | 0.06 | 8 | 2 | 0.375 | Synergy |
| A4 | 0.24 | 0.12 | 16 | 0.5 | 0.531 | Additive |
| A5 | 0.24 | 0.06 | 8 | 2 | 0.5 | Synergy |
| A6 | 0.24 | 0.12 | 16 | 1 | 0.563 | Additive |
| A7 | 0.48 | 0.12 | 4 | 1 | 0.5 | Synergy |
| A8 | 0.96 | 0.48 | 8 | 0.5 | 0.563 | Additive |
| A9 | 0.96 | 0.12 | 4 | 0.5 | 0.25 | Synergy |
| A10 | 0.48 | 0.24 | 8 | 0.5 | 0.563 | Additive |
| A11 | 0.24 | 0.12 | 8 | 0.5 | 0.563 | Additive |
MIC values of azithromycin alone and in combination with cefixime for S. pneumoniae
| S. pneumoniae |
| Strains | MIC Azithromycin | MIC Cefixime | FIC index | Outcome |
| Alone (μg/ml) | With Cefixime (μg/ml) | Alone (μg/ml) | With Azithromycin (μg/ml) |
| A1 | 16 | 4 | 4 | 0.5 | 0.375 | Synergy |
| A2 | 16 | 4 | 8 | 2 | 0.5 | Synergy |
| A3 | 16 | 8 | 16 | 2 | 0.563 | Additive |
| A4 | 64 | 8 | 8 | 2 | 0.375 | Synergy |
| A5 | 16 | 8 | 8 | 0.5 | 0.563 | Additive |
| A6 | 64 | 32 | 8 | 0.5 | 0.563 | Additive |
| A7 | 64 | 8 | 8 | 0.3 | 0.375 | Synergy |
| A8 | 1 | 0.25 | 32 | 0.3 | 0.375 | Synergy |
| A9 | 64 | 8 | 8 | 0.3 | 0.375 | Synergy |
| A10 | 1 | 0.5 | 16 | 0.5 | 0.563 | Additive |
| A11 | 16 | 4 | 4 | 0.5 | 0.5 | Synergy |
MIC values of azithromycin alone and in combination with cefixime for H. influenzae
| H. influenzae |
| Strains | MIC Azithromycin | MIC Cefixime | FIC index | Outcome |
| Alone (μg/ml) | With Cefixime (μg/ml) | Alone (μg/ml) | With Azithromycin (μg/ml) |
| A1 | 64 | 4 | 2 | 1 | 0.563 | Additive |
| A2 | 64 | 4 | 16 | 8 | 0.563 | Additive |
| A3 | 16 | 8 | 8 | 0.5 | 0.563 | Additive |
| A4 | 64 | 8 | 8 | 2 | 0.375 | Synergy |
| A5 | 64 | 32 | 16 | 1 | 0.563 | Additive |
| A6 | 64 | 4 | 16 | 0.5 | 0.188 | Synergy |
| A7 | 16 | 4 | 16 | 1 | 0.313 | Synergy |
| A8 | 16 | 4 | 32 | 8 | 0.5 | Synergy |
| A9 | 64 | 32 | 16 | 1 | 0.563 | Additive |
| A10 | 128 | 32 | 16 | 4 | 0.5 | Synergy |
| A11 | 64 | 8 | 8 | 0.25 | 0.156 | Synergy |
Comparison of cefixime mean MIC as alone and in combination with azithromycin against study bacterial types
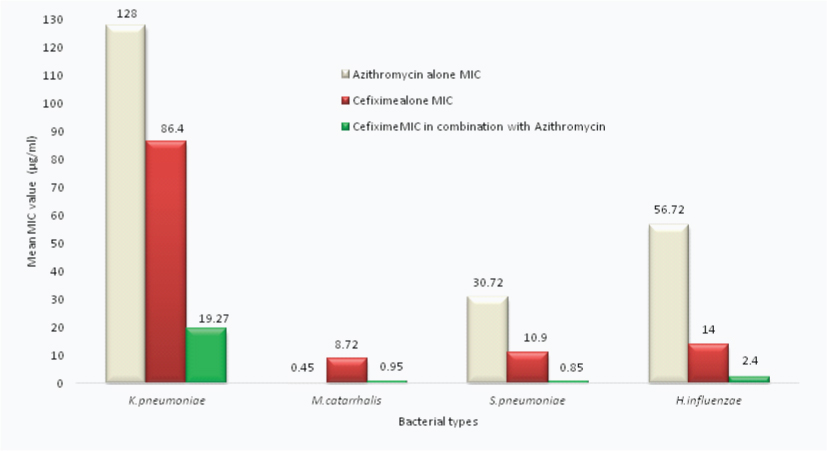
Similarly the mean MIC of azithromycin in combination with cefixime as compared to alone dropped by 5, 2.6, 3.9 and 4.5 fold for K. pneumoniae, M. catarrhalis, S. pneumoniae and H. influenzae respectively.
FIC index showed synergy in 66% (29/44) isolates, while additive effect in 34% (15/44) isolates. Maximum synergy of Cefixime-azithromycin FDC was observed against K. pneumoniae in 91% isolates.
Discussion
Third generation cephalosporins and macrolides such as Azithromycin have been found to be effective drugs in the management of RTIs. But rampant use of these antibiotics in the real life setting has led to the emergence of resistant strains of respiratory tract pathogens.
Cefixime is an orally active third-generation cephalosporin. It has broad spectrum of activity against various pathogens, including gram-negative organisms which are beta-lactamase producing strains [9]. Azithromycin is a macrolide with an expanded spectrum of activity and improved tissue pharmacokinetic. The drug is noted for its activity against some gram-negative organisms associated with RTIs, particularly. H. influenzae [10]. Azithromycin has similar properties to other macrolides against S. pneumoniae and (M. catarrhalis), and is active against atypical pathogens such as (L. pneumophilae), C. pneumoniae and M. pneumoniae [11].
The current study has demonstrated synergism of cefixime and azithromycin combination. There are few studies in literature documenting the in vitro effects of cefixime in combination with azithromycin. Furuya et al., demonstrated that cefixime can have synergistic effects in combination with azithromycin for Neisseria gonorrhoea [12].
The FIC of each agent was calculated as a ratio of the MIC when used in combination and the MIC when used alone. FIC index is the sum of the FIC of the two agents used in the combination [13]. FIC indexes were interpreted as previously defined synergy at a FIC index ≤0.5; additive at a FIC index >0.5 to 1; indifference at a FIC index >1–<2; and antagonism at a FIC index ≥2 [14]. Fall of MIC for both cefixime and azithromycin in combination along with combinational FIC index of less than one in all clinical isolates of has proved synergistic and additive effects of Cefixime-azithromycin.
Macrolide alone in S.pneumoniae has shown resistance upto 14% in Chawla et al., study. Prevalence of BLNAR positive H.influenzae is rising in South East Asian countries, showing upto 73% resistance towards conventional BL/BLIs. Incidence of atypical pathogens causing CAP in India is around 24% in Kashyap et al., study [15–18]. Macrolides once the cornerstone in the treatment of atypical pathogens, resistance is on the rise globally. Clinical studies by Waterer et al., Lodies et al., Rodrigo et al., Weiss et al., and Dudas et al., on the combination use of β-lactam and macrolide in CAP and pneumococcal bacteremia showed better results in terms of clinical outcome, length of stay and mortality [19–23].
Antibiotic combination therapy produces synergistic effects and reduces mortality at high risk for treatment failure, in comparison with monotherapy [24]. Various speciality societies like American Thoracic Society (ATS), British Thoracic Society (BTS), Infectious Disease Society of America (IDSA) and Canadian Infectious Disease Society (CIDS) recommended use of empiric combination therapy in management of RTI like CAP [5].
Conclusion
This is one of the first attempts to check the rationality of fixed dose antibiotic combination of cefixime and azithromycin in Indian market. Though results of this study cannot be generalized considering the limitations of low sample size and in vitro model, our data provides stepping stone for further validation of cefixime and azithromycin FDCs in clinical setting by conducting randomized controlled trials. We think that judicious and rational use of fixed dose antibiotic combinations may help to reduce the selection of further drug resistance along with proved clinical outcome.
[1]. Biswas PP, Prabhu TK, Bacterial causes of lower respiratory tract infections in patients attending central referral hospital, Gangtok with reference to antibiotic resistance patternJ of Evolution of Med and Dent Sci 2013 42(2):8126-35. [Google Scholar]
[2]. Indira KS, Chandy SJ, Jeyaseelan L, Kumar R, Suresh S, Antimicrobial prescription patterns for common acute infections in some rural & urban health facilities of IndiaIndian J Med Res 2008 128(2):165-71. [Google Scholar]
[3]. Gonzales R, Bartlett JG, Besser RE, Cooper RJ, Hickner JM, Hoffman JR, Principles of appropriate antibiotic use for treatment of acute respiratory tract infections in adults: background, specific aims, and methodsAnn Emerg Med 2001 37(6):690-97. [Google Scholar]
[4]. Leekha S, Terrell CL, Edson RS, General principles of antimicrobial therapyMayo Clin Proc 2011 86(2):156-67. [Google Scholar]
[5]. Mehta KC, Dargad RR, Borade DM, Swami OC, Burden of antibiotic resistance in common infectious diseases: role of antibiotic combination therapyJ Clin Diagn Res 2014 8(6):ME05-08. [Google Scholar]
[6]. Torella JP, Chait R, Kishony R, Optimal drug synergy in antimicrobial treatments. Bourne PEPLoS Comput Biol. Public Library of Science 2010 6(6):e1000796 [Google Scholar]
[7]. Caballero J, Rello J, Combination antibiotic therapy for community-acquired pneumoniaAnn Intensive Care 2011 1(1):48 [Google Scholar]
[8]. Den Hollander JG, Mouton JW, Verbrugh HA, Use of pharmacodynamic parameters to predict efficacy of combination therapy by using fractional inhibitory concentration kineticsAntimicrob Agents Chemother. 1998 42(4):744-48. [Google Scholar]
[9]. Matsumoto Y, Combination cefixime/amoxicillin against penicillin-resistant Streptococcus pneumoniae infectionChemotherapy 1998 44(Suppl 1):6-9. [Google Scholar]
[10]. Dunn CJ, Barradell LB, Azithromycin. A review of its pharmacological properties and use as 3-day therapy in respiratory tract infectionsDrugs 1996 51(3):483-505. [Google Scholar]
[11]. Thibodeau KP, Viera AJ, Atypical pathogens and challenges in community-acquired pneumoniaAm Fam Physician 2004 69(7):1699-706. [Google Scholar]
[12]. Furuya R, Nakayama H, Kanayama A, Saika T, Iyoda T, Tatewaki M, In vitro synergistic effects of double combinations of beta-lactams and azithromycin against clinical isolates of Neisseria gonorrhoeaeJ Infect Chemother 2006 12(4):172-76. [Google Scholar]
[13]. Den Hollander JG, Mouton JW, Verbrugh HA, Use of pharmacodynamic parameters to predict efficacy of combination therapy by using fractional inhibitory concentration kineticsAntimicrob Agents Chemother 1998 42(4):744-48. [Google Scholar]
[14]. Source:Terminology relating to methods for the determination of susceptibilityof bacteria to antimicrobial agents. Eucast Definitive Document E.Def 1.2. 2000 [Google Scholar]
[15]. Chawla K, Gurung B, Mukhopadhyay C, Bairy I, Reporting Emerging Resistance of Streptococcus pneumoniae from IndiaJ Glob Infect Dis 2010 2(1):10-14. [Google Scholar]
[16]. Tristram S, Jacobs MR, Appelbaum PC, Antimicrobial resistance in Haemophilus influenzaeClin Microbiol Rev 2007 20(2):368-89. [Google Scholar]
[17]. Hasegawa K, Yamamoto K, Chiba N, Kobayashi R, Nagai K, Jacobs MR, Diversity of ampicillin-resistance genes in Haemophilus influenzae in Japan and the United StatesMicrob Drug Resist 2003 9(1):39-46. [Google Scholar]
[18]. Bébéar C, Pereyre S, Peuchant O, Mycoplasma pneumoniae: susceptibility and resistance to antibioticsFuture Microbiol 2011 6(4):423-31. [Google Scholar]
[19]. Waterer GW, Somes GW, Wunderink RG, Monotherapy may be suboptimal for severe bacteremic pneumococcal pneumoniaArch Intern Med 2001 161(15):1837-42. [Google Scholar]
[20]. Lodise TP, Kwa A, Cosler L, Gupta R, Smith RP, Comparison of beta-lactam and macrolide combination therapy versus fluoroquinolone monotherapy in hospitalized Veterans Affairs patients with community-acquired pneumoniaAntimicrob Agents Chemother 2007 51(11):3977-82. [Google Scholar]
[21]. Rodrigo C, Mckeever TM, Woodhead M, Lim WS, Single versus combination antibiotic therapy in adults hospitalised with community acquired pneumoniaThorax 2013 68(5):493-95. [Google Scholar]
[22]. Weiss K, Low DE, Cortes L, Beaupre A, Gauthier R, Gregoire P, Clinical characteristics at initial presentation and impact of dual therapy on the outcome of bacteremic Streptococcus pneumoniae pneumonia in adultsCan Respir J11(8):589-93. [Google Scholar]
[23]. Dudas V, Hopefl A, Jacobs R, Guglielmo BJ, Antimicrobial selection for hospitalized patients with presumed community-acquired pneumonia: a survey of nonteaching US community hospitalsAnn Pharmacother 2000 34(4):446-52. [Google Scholar]
[24]. Tamma PD, Cosgrove SE, Maragakis LL, Combination therapy for treatment of infections with gram-negative bacteriaClin Microbiol Rev 2012 25(3):450-70. [Google Scholar]