Neurocysticercosis (NCC) with Hydrocephalus, Optic Atrophy and Vision Loss: A Rare Presentation
Nagendra Chaudhary1, Shyam Kumar Mahato2, Salamat Khan3, Santosh Pathak4, B.D Bhatia5
1Assistant Professor, Department of Pediatrics,Universal College of medical Sciences, Bhairahawa, Nepal.
2Assistant Professor, Department of Pediatrics,Universal College of medical Sciences, Bhairahawa, Nepal.
3Professor, Department of Surgery,Universal College of medical Sciences, Bhairahawa, Nepal.
4Junior Resident, Department of Pediatrics,Universal College of medical Sciences, Bhairahawa, Nepal.
5Professor and Head of Department, Department of Pediatrics,Universal College of medical Sciences, Bhairahawa, Nepal.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Nagendra Chaudhary, Assistant Professor, Department of Pediatrics, Universal College of Medical Sciences, Bhairahawa, Nepal.
E-mail: enagendra@hotmail.com
Neurocysticercosis (NCC) is one of the most common parasitic infestations (Taenia solium) of central nervous system (CNS) in children. Seizures are the common presenting symptoms. Hydrocephalus and optic atrophy are rare complications which may require neurosurgical interventions. We report a case of NCC with hydrocephalus and bilateral optic atrophy associated with vision loss in a Nepalese patient who improved with anti-parasitic therapy followed by ventriculo-peritoneal (VP) shunting.
Central nervous system, Parasitic infestations, Taenia solium
Case Report
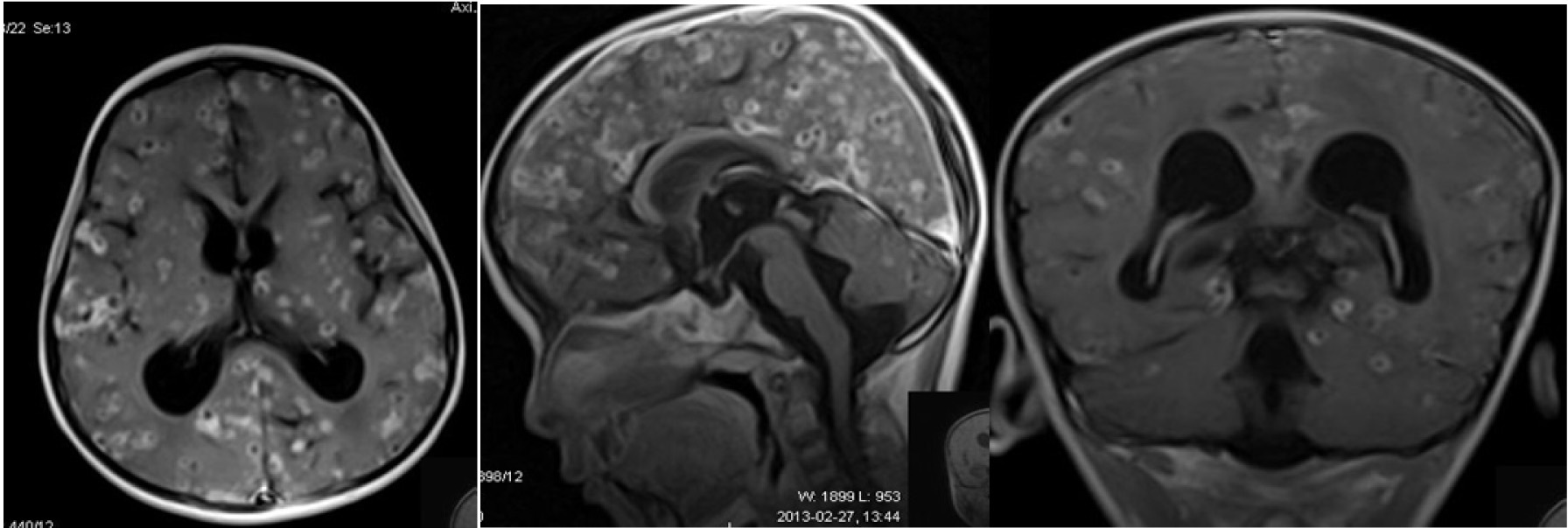
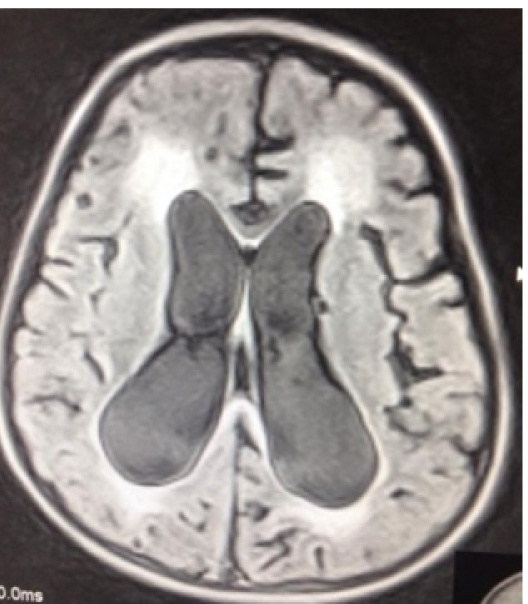
An 8-year-old male from western Nepal presented with history of bilateral frontal headache for six months, blurring of vision, and double vision with progressive decrease in visual acuity for one month. On presentation, he could view objects at a distance of about 30-35 cm but could not identify their colour. There was no history of seizures. He had normal developmental history with no regression of any milestones. Birth history was uneventful. He was immunized appropriately. On examination, vitals were stable. CNS examination revealed bilateral equal symmetrical pupils, sluggishly reacting to light with intact consensual light reflex.Visual acuity revealed finger counting up to 30-35 cm distance. Colour vision was absent. Fundus examination showed bilateral pale disc with features suggestive of optic atrophy. There was UMN type facial palsy with no other neurological deficits. Other systemic examination was normal.Complete blood count and chest X-ray were normal. Mantoux test was negative. Magnetic resonance imaging (MRI) of brain revealed ring enhancing lesions (active stage) in multiple locations, bilateral hydrocephalus with diffuse high signal intensity involving periventricular white matter, cerebellum and sub cortical U fibers as shown in [Table/Fig-1,2,3]. Child was treated with Methyl Prednisolone (30 mg/kg/day) for five days followed by oral Prednisolone (2 mg/kg/day) for 28 days and finally tapered and stopped. Albendazole (15 mg/kg/day) was given for 28 d. He was also given Phenytoin (5 mg/kg/day) and Acetazolamide (30 mg/kg/soliumday). Repeat MRI [Table/Fig-4] after one month was suggestive of worsening of hydrocephalus with periventricular ooze. A VP shunt was put. On 12 months follow up, there was no evidence of shunt blockage and child had improvement in visual acuity.
Discussion
NCC, one of the most common helminthic infestations of the brain, is highly prevalent in countries like India and Nepal.WHO estimates that more than 50,000 deaths occur every year due to NCC. CNS involvement is seen in 60–90% of infested patients [1]. Cerebrum and cerebellum are common sites but cysticerci may involve brainstem, basal ganglion, thalamus and lateral sinus as well. The larval stage of T. solium can migrate to any organ in the body, but most reports have focused on cysts located in the CNS, eyes, muscles or subcutaneous tissues [2]. Intraventricular (5–10%) and meningeal cysticerosis are associated with hydrocephalus, signs of meningeal irritation and raised intracranial pressure [1].
The clinical manifestation depends on the location of the cyst along with the host`s immunity [3]. Seizures are the most common manifestations followed by headache, hydrocephalus, chronic meningitis, focal neurological deficits and psychological disorders [4]. It is the most common cause of acquired epilepsy and neurological morbidity in many developing countries [3]. Studies from India suggest that seizures/epilepsy is common in children than adult population [5]. A community based survey conducted [6] in Morang district of Nepal showed the prevalence of epilepsy around 7.3% and a cohort of 300 patients showing NCC as an important aetiological agent. In a recent study, Adhikari et al., [7] reported NCC as the common CT findings in abnormal brain scans and a common cause of epilepsy in western Nepal.
Hydrocephalus is a well-known complication of NCC which occurs due to mechanical compression of ventricles or the basal cisterns either due to the cysts or inflammation of ependyma or arachnoid matter which requires aggressive management. It is generally managed by VP shunt but shunt blockage remains major complications [8]. Medical treatment (Acetazolamide, Furosemide) has little role in hydrocephalus secondary to intraventricular and subarachnoid cysts (Extra parenchymal NCC). Although intraventricular cysts are rare, three cases have been reported by Pant et al., in Nepal [9] which is best managed by endoscopic removal of the cysts.
The present case had bilateral optic atrophy. Vision loss is one of the serious complications of NCC which can occur either due to direct involvement of optic nerve or any part of the visual pathway from the eye ball to the visual cortex. Optic nerve can be affected due to compression of the nerve in the optic canal and optic chiasma or due to raised ICP. All the manifestations like papilledema, unilateral optic atrophy and bilateral optic atrophy have been reported in literature [10]. Optic disc atrophy leads to damage or death of the optic nerve fibers that derive from the retinal ganglion cells of the inner retina leading to vision loss as well as loss of colour vision. Pansey et al., has reported a five-year-old boy with B/L optic atrophy, headache and blindness who recovered after anti-parasitic treatment [11]. Atypical ophthalmological features like nystagmus and diplopia too have been reported in two cases by Jethani et al., who recovered with medical treatment [12]. Simultaneous intraocular and extra ocular cysticercosis reported by Chadha in a 21-year-old boy having sudden loss of vision and seizure improved with Albendazole and Prednisolone therapy [13]. Our case also underwent anti-parasitic treatment and required VP shunting with no further deterioration in vision and hydrocephalus in subsequent follow-up.
Magnetic resonance imaging (Transverse, sagittal and coronal sections) showing multiple NCC with hydrocephalus
Shows repeat MRI (FLAIR) section showing worsening of hydrocephalus
Conclusion
The peculiarity of this case was progressive vision loss, hydrocephalus and optic atrophy without any evidence of seizures or encephalopathy. Neurocysticercosis, being a common aetiology of seizures in developing countries, can even present with devastating complications like hydrocephalus and optic atrophy which can lead to permanent loss of vision with persisting neurological sequlae. Timely diagnosis with appropriate medical and surgical interventions (VP shunting) decreases the morbidity and death in such cases.
Acknowledgement
We acknowledge the patient and his parent for giving the consent for publication.
[1]. MW Hawk, K Shahlaie, KD Kim, JH Theis, Neurocysticercosis: a reviewSurg Neurol 2005 63(5):123-32. [Google Scholar]
[2]. SK Handique, RR Das, B Saharia, P Das, R Buragohain, P Saikia, Coinfection of Japanese encephalitis with neurocysticercosis: an imaging studyAJNR Am J Neuroradiol 2008 29(1):170-75. [Google Scholar]
[3]. KN Prasad, A Prasad, A Verma, AK Singh, Human cysticercosis and Indian scenario: a reviewJ Biosci 2008 33(4):571-82. [Google Scholar]
[4]. HH García, AE Gonzalez, CAW Evans, RH Gilman, Cysticercosis Working Group in Peru. Taenia solium cysticercosisLancet 2003 362(9383):547-56. [Google Scholar]
[5]. P Singhi, S Singhi, Neurocysticercosis in childrenIndian J Pediatr 2009 76(5):537-45. [Google Scholar]
[6]. KC Rajbhandari, Epilepsy in NepalCan J Neurol Sci J Can Sci Neurol 2004 31(2):257-60. [Google Scholar]
[7]. S Adhikari, B Sathian, DP Koirala, KS Rao, Profile of children admitted with seizures in a tertiary care hospital of Western NepalBMC Pediatr 2013 13:43 [Google Scholar]
[8]. HH Garcia, G Herrera, RH Gilman, VC Tsang, JB Pilcher, JF Diaz, Discrepancies between cerebral computed tomography and western blot in the diagnosis of neurocysticercosis. The Cysticercosis Working Group in Peru (Clinical Studies Coordination Board)Am J Trop Med Hyg 1994 50(2):152-57. [Google Scholar]
[9]. B Pant, B Devleesschauwer, P Shrestha, I Shrestha, N Praet, P Dorny, Intraventricular Taenia solium neurocysticercosis: a report of three casesJNMA J Nepal Med Assoc 2011 51(184):192-95. [Google Scholar]
[10]. GY Chang, JR Keane, Visual loss in cysticercosis: analysis of 23 patientsNeurology 2001 57(3):545-48. [Google Scholar]
[11]. BK Pansey, KS Basra, R Pasricha, Medically treated neurocysticercosis in a blind child. A case reportSurg Neurol 1989 32(1):56-58. [Google Scholar]
[12]. J Jethani, P Vijayalakshmi, M Kumar, Atypical ophthalmological presentation of neurocysticercosis in two childrenJ AAPOS Off Publ Am Assoc Pediatr Ophthalmol Strabismus Am Assoc Pediatr Ophthalmol Strabismus 2007 11(5):495-96. [Google Scholar]
[13]. V Chadha, PK Pandey, D Chauhan, S Das, Simultaneous intraocular and bilateral extraocular muscle involvement in a case of disseminated cysticercosisInt Ophthalmol 2005 26(1-2):35-37. [Google Scholar]