Amyand’s Hernia: Case Report -Current Dilemma in Diagnosis and Management
Jonathan Sadhu1, Vasanth Mark Samuel2, Thomas Kodiatte3, Pranay Gaikwad4
1Assistant Professor, Department of General Surgery,Christian Medical College, Vellore, India.
2Assistant Professor, Department of General Surgery,Christian Medical College, Vellore, India.
3Assistant Professor, Department of Pathology,Christian Medical College, Vellore, India.
4Professor, Department of General Surgery,Christian Medical College, Vellore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jonathan Sadhu, Assistant Professor, Department of General Surgery, Christian Medical College, Vellore, India.
E-mail: Jona10sadhu@yahoo.co.in
Amyand’s hernia is an extremely rare condition, often misdiagnosed as a strangulated inguinal hernia, in which the inguinal hernial sac contains the vermiform appendix. It is often a surgical surprise. The reported incidence is approximately 1% of all adult inguinal hernia cases. Acute appendicitis in the Amyand’s hernia is even less common. We report a rare presentation of acute appendicitis associated with Amyand’s hernia managed by en masse reduction of the hernia followed by laparoscopic appendicectomy and open Lichtenstein’s tension free inguinal hernioplasty.
Acute appendicitis, Inguinal hernia, Laparoscopic appendicectomy
Case Report
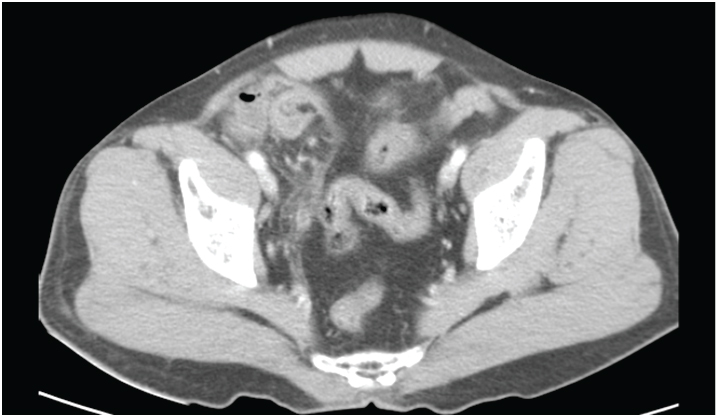
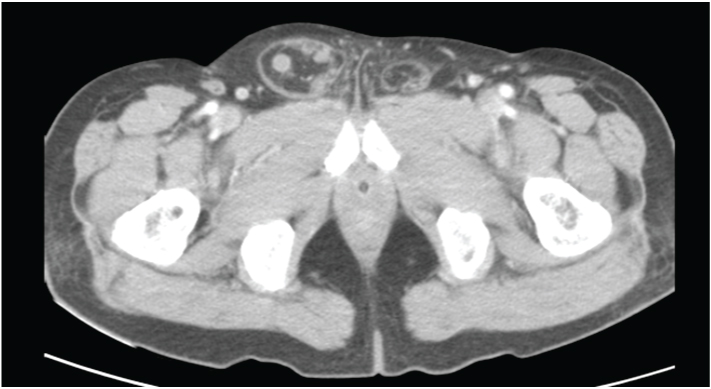
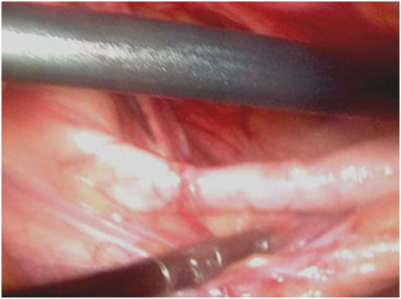
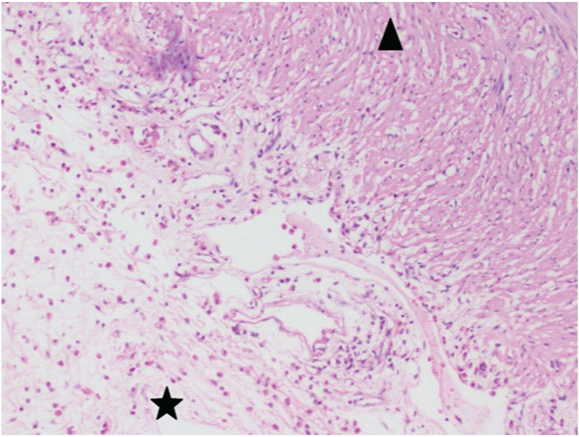
A 60-year-old male presented to the emergency department with history of a swelling in the right groin for 6-months. The swelling became irreducible for 3 days with associated right lower abdominal pain and non-bilious vomiting. On examination, pulse rate was 96 per minute and blood pressure 120/70mm Hg. Abdominal examination revealed minimal tenderness in the right lower quadrant with sluggish bowel sounds and an irreducible right inguinal hernia. Supine X-ray of the abdomen revealed a few dilated jejunal loops in the upper abdomen but was otherwise unremarkable. The patient was planned for emergency herniotomy, however the hernia reduced in the interim and he moved bowel by passing flatus and a small amount of stools. The following day the patient complained of nausea and increased lower abdominal pain. Review examination revealed guarding in the right iliac fossa. The total leukocyte count at admission was 16,100/mm3 with 87% neutrophils, 6% lymphocytes and 7% monocytes. Ultrasound abdomen revealed no gross abnormality. Abdominal CT scan showed right inguinal hernia with caecum as its content [Table/Fig-1] . The appendix was not clearly visualized [Table/Fig-2]. With the clinical impression of a possibility of acute appendicitis, a diagnostic laparoscopy was performed. Intra-operatively, there was a direct inguinal hernia with the caecum and an inflamed appendix forming its content [Table/Fig-3].The patient underwent laparoscopic appendicectomy and an open Lichtenstein inguinal mesh hernioplasty using a polypropylene mesh. The patient was discharged on the 4th post -operative day and the skin staples were removed on the 10th post- operative day. At one month follow up, the patient was well. Biopsy revealed acute appendicitis [Table/Fig-4].
Discussion
Amyand’s hernia is a rare condition and its diagnosis pre-operatively remains elusive. Apostolidis et al., have shown that only one out of 60 cases was diagnosed pre-operatively [1]. Thomas et al., reported their series of seven patients that presented with pain in the right iliac fossa, vomiting, fever and tender swelling in the right groin with the initial diagnosis of strangulated hernia [2]. However, in contradiction to the constant pain seen in strangulation, the pain in Amyand’s hernia has been described as episodic and crampy [3].Pyrexia and leukocytosis are inconstant findings [4]. In men, the condition may be confused with acute scrotal or testicular conditions [5]. Inflammation of the appendix is attributed to its compression at the neck of the sac. In the past when associated with an inflamed or perforated appendix, appendicectomy and primary repair (Bassini) of the hernia have been suggested [6]. Logically, in the presence of a normal appendix within the sac, a prophylactic appendicectomy should be avoided due to potential contamination of the otherwise clean operative field that utilizes placement of prosthetic mesh for hernia repair. Chatzimavroudis et al., however have shown that the presence of an inflamed or perforated appendix in the hernial sac is not an absolute contra-indication for use of synthetic mesh and reported no post-operative complications with repair [7]. Torino et al., also support the use of synthetic mesh if the wound is irrigated intra-operatively with antibiotics, drains are placed and antibiotics are continued postoperatively [8].
Amyand’s hernia has been classified by Fernando et al., according to the degree of inflammation of the appendix to Type A - non-inflamed, Type B - inflamed and Type C - perforated; Type A accounting for nearly 90% of cases [9]. Types B and C mandate appendicectomy and according to them, are contra-indications for the mesh repair due to the high risk of infection. All case series, to date, have described the open or laparoscopic appendicectomy followed by primary repair of inguinal hernia [10,11]. Khan et al., have described the complete laparoscopic repair of an Amyand’s hernia (laparoscopic appendicectomy with laparoscopic suture closure of the deep inguinal ring) in a patient on high dose systemic steroids to avoid an additional incision [12]. A total laparoscopic repair can be attempted with both trans-abdominal or preperitoneal approaches having been described [13,14]. In our case, exploratory laparoscopy revealed a direct inguinal hernia with a probable sliding component containing the caecum and appendix for which laparoscopic appendicectomy and open mesh repair of the right direct inguinal hernia were performed.
Caecum forming content of the right inguinal hernia
Appendix within the hernial sac
Appendix after reduction from the hernial sac
(Photomicrograph - 100x) demonstrates acute inflammatory cells (eosinophils and neutrophils) in the muscularispropria of the appendix (arrow head) and sub-serosal connective tissue (star)
Conclusion
Amyand’s hernia is rare and remains a surgical enigma. If diagnosed pre-operatively by imaging we recommend use of early diagnostic laparoscopy. If a direct sac is identified with an inflamed appendix, a laparoscopic appendicectomy with open mesh repair (without opening the sac) is recommended as it reduces the need for an elective appendicectomy later.
[1]. S Apostolidis, V Papadopoulos, A Michalopoulos, D Paramythiotis, N Harlaftis, Amyand’s hernia: A case report and review of literatureInternet J Surg 2005 6:1 [Google Scholar]
[2]. WE Thomas, KD Vowles, RC Williamson, Appendicitis in external herniaeAnn R Coll Surg Engl 1982 64:121-22. [Google Scholar]
[3]. S Lyass, A Kim, J Bauer, Perforated appendicitis within an inguinal hernia: case report and review of the literatureAm J Gastroenterol 1997 92:700-0. [Google Scholar]
[4]. R Hutchinson, Amyand’s herniaJ R Soc Med 1993 86(1):104-05. [Google Scholar]
[5]. LC Carey, Acute appendicitis occurring in hernias: a report of 10 casesSurgery 1967 61(2):236-38. [Google Scholar]
[6]. H Sharma, A Gupta, NS Shekhawat, B Memon, MA Memon, Amyand’s hernia: a report of 18 consecutive patients over a 15-year periodHernia J Hernias Abdom Wall Surg 2007 11(1):31-35. [Google Scholar]
[7]. G Chatzimavroudis, B Papaziogas, I Koutelidakis, P Tsiaousis, T Kalogirou, S Atmatzidis, The role of prosthetic repair in the treatment of an incarcerated recurrent inguinal hernia with acute appendicitis (inflamed Amyand’s hernia)Hernia J Hernias Abdom Wall Surg 2009 13(3):335-36. [Google Scholar]
[8]. G Torino, C Campisi, A Testa, E Baldassarre, G Valenti, Prosthetic repair of a perforated Amyand’s hernia: hazardous or feasible?Hernia J Hernias Abdom Wall Surg 2007 11(6):551-52. [Google Scholar]
[9]. J Fernando, S Leelaratna, Amyand’s herniaCeylon Med J 2002 47(2):71 [Google Scholar]
[10]. JF Tycast, AL Kumpf, TL Schwartz, CE Coln, Amyand’s hernia: a case report describing laparoscopic repair in a pediatric patientJ Pediatr Surg 2008 43(11):2112-14. [Google Scholar]
[11]. JM Vermillion, SW Abernathy, SK Snydern, Laparoscopic reduction of Amyand’s herniaHernia 1999 3:159-60. [Google Scholar]
[12]. O Khan, S McInnes, A Parvaiz, Totally Laparoscopic Repair of an Acutely Inflammed Amyand’s HerniaJ Minim Invasive Surg Sci 2012 2(1):28-33. [Google Scholar]
[13]. B Elias, E Chelala, JL Allé, Transabdominal Laparoscopic Repair of Amyand’s Hernia: A Case ReportCase Rep Surg 2011 2011(11):823-936. [Google Scholar]
[14]. SK Sarker, K Jackson, Laparoscopic extraperitoneal repair of Amyand’s inguinal herniaJSLS J Soc Laparoendosc Surg Soc Laparoendosc Surg 2006 10(4):528-30. [Google Scholar]