Osteoblastic and Osteoclastic Metastases in a Single Vertebra-A Rare Presentation
Gian Chand1, Ajay Chhabra2, Deepshikha Mangat3, Suparna Grover4
1Associate Professor, Department of Medicine,Government Medical College, Amritsar, India.
2Associate Professor, Department of Medicine,Government Medical College, Amritsar, India.
3Resident Doctor, Department of Microbiology,Government Medical College, Amritsar, India.
4Assistant Professor, Department of Obstetrics and Gynaecology,Government Medical College, Amritsar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ajay Chhabra, 429, Akash Avenue, Fatehgarh Churian Road, Amritsar-143001, India.
E-mail: drajaychhabra@gmail.com
Malignancies may produce bony metastases which may be osteoclastic or osteoblastic. Vertebrae are a common site for bony metastases. Prostatic adenocarcinoma is an important source of vertebral metastases that are mainly osteoblastic in nature. As the osteoblastic metastases are developing there is an ongoing osteoclastic activity which is going on at the microscopic level. Presence of gross osteoblastic and osteoclastic lesions, in the same vertebra, have not been reported at the time of presentation. Here a rare case of vertebral metastases is being presented which shows osteoblastic and osteoclastic gross lesions in the same vertebra.
Metastasis, Osteoclastic, Osteoblastic, Prostate
Case Report
A 67-year-old male patient presented to the outpatient department with chief complaint of backache since three months which had been gradually progressive and it radiated to the lower limbs. It was aggravated by walking, stooping down and going up the stairs. There was no history of fall or any trauma to the back. Besides, patient had a history of significant weight loss of around 9 kg over the previous three months. He had to strain while micturition. There was no significant past history except that the patient was a known case of hypertension taking antihypertensive regularly.
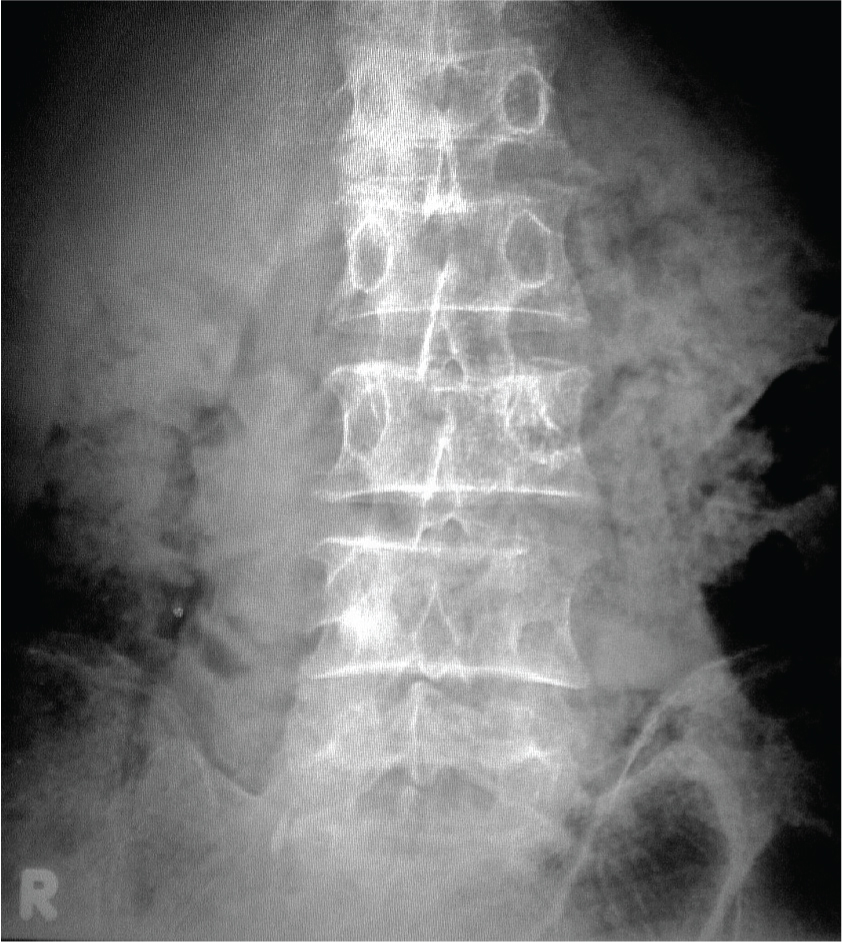
On general examination patient had mild pallor. There was tenderness over the lumbar region but there was no swelling or any deformity. In the left inguinal region a hard lymph node was noticed. Digital rectal examination was suggestive of enlarged prostate which was hard in consistency and asymmetrical. Routine laboratory investigations were normal except that the patient had anemia (Hb-9.4 g/dL). Serum alkaline phosphate levels were Grover4increased to 573 IU/L. Serum prostate specific antigen was 117ng/ml. X-ray lumbo-sacral spine showed a lytic and a blastic lesion in the same L4 vertebra [Table/Fig-1]. Computerised tomographic scanning confirmed the presence of osteoblastic and osteoclastic lesions in the same L4 vertebra, with rest of the spine being spared [Table/Fig-2]. Prostatic biopsy was done which showed presence of prostatic adenocarcinoma with a Gleason score of 9. Patient was advised bilateral orchiectomy and is on follow up.
Discussion
Bones constantly undergo a process of remodeling. Two main types of bone cells normally work in conjunction to keep bones healthy and strong. The cells that form new bone are called osteoblasts. Certain paracrine secretions of the metastatic cells enhance their activity that leads to new bone formation, which is hard sclerotic but abnormal. The cells that remove old bone are called osteoclasts which lead to bone break down without new bone being formed under the influence of peptides released by cancer cells. The porosities that develop when parts of bones get dissolved are called osteolytic or lytic lesions [1,2].
Primaries with predominantly osteoblastic metastases are prostatic carcinoma, bladder cancer, stomach cancer and breast cancer after radiotherapy. Mixed lytic and osteoblastic lesions may coexist in rare cases of breast, lung, kidney and liver cancer especially after irradiation. Primaries producing osteolytic metastases include lung, gastrointestinal tract, breast, kidney cancers and multiple myeloma [1].
One of the most common sites of skeletal metastases is the vertebrae [2]. Vertebral metastases most commonly occur in the lumbar region [3]. Prostatic carcinoma metastasizes in 33-85% cases [3]. Metastasizing prostatic carcinoma produces mainly osteoblastic metastasis [4].
Prostatic cancer contributes to 60% of bony metastasis in males [1]. Prostatic metastasis may produce both osteoblastic and osteoclastic metastasis. More than 90% of metastases arising from the prostate are osteoblastic [5]. One can see osteolytic along with osteoblastic activity in the same histopathological section. It is unusual to see both types of lesions grossly. Within the same lesion one can see both types of activities microscopically [6]. Metastases are either osteoblastic or osteoclastic, however, osteoid formation and mineralization is of limited help in determining the primary tumour as some metastases may secrete osteoblast- and osteoclast-stimulating factors at the same time [6].
Osteoblastic proliferation is affected by endothelin-1 [7], transforming growth factor-β2 [8] and fibroblastic growth factors [9] which are expressed by metastatic prostatic cells. Prostatic cell also produce prostate specific antigen (PSA) which not only is a tumour marker but also acts as a serine protease responsible for cleavage of various peptides like parathyroid hormone related peptide (PTHrH), insulin like growth factor and transforming growth factor-β into active forms which stimulate osteoblast activity [10]. IL-6 expressed in prostatic cells stimulates osteoclasts strengthening the effects of PTHrP onto osteoclasts [11]. PTHrP and IL-6 induce osteoclastic bone resorption stimulating osteoblasts and stromal cells to produce the receptor activator of nuclear factor-kB. This factor links to its receptor on the osteoclastic precursors inducing their proliferation and differentiation [12].
Our patient had two lesions one osteoblastic and the other osteoclastic that to in the same vertebra, which is a rare finding. Although osteoblastic and osteoclastic activity can be seen going together at the cellular level, to see metastasis of the same tumour producing two different lesions grossly is an uncommon presentation.
X-ray lumbo-sacral spine at the time of presentation showing an osteoblastic and osteoclastic lesion
Computerised tomographic image of the lumbar vertebra showing both types of metastases

Conclusion
Osteoblastic activity coexists with osteoclastic activity at the microscopic level but a tumour metastases producing different lesions in the same vertebra at the macroscopic level is intriguing and requires further study.
[1]. Kogon Peter L, McLaughlin Kevin J, Metastatic bone disease: a review of various concepts and report of a caseJ Can Chiropr Assoc 1988 32:127-32. [Google Scholar]
[2]. WA Abdu, M Provencher, Primary bone and metastatic tumours of the cervical spineSpine 1998 23:2767-77. [Google Scholar]
[3]. G Maccauro, MS Spinelli, S Mauro, C Perisano, C Graci, MA Rosa, Physiopathology of Spine MetastasisInt J Surg Oncol 2011 8 [Google Scholar]
[4]. K Jung, M Lein, C Stephan, KV Hosslin, A Semjonow, P Sinha, Comparison of 10 serum bone turnover markers in prostate carcinoma patients with bone metastatic spread: diagnostic and prognostic implicationsInt J Cancer 2004 111:783-91. [Google Scholar]
[5]. MP Roudier, C Morrissey, LD True, CS Higano, RL Vessella, SM Ott, Histopathological assessment of prostate cancer bone osteoblastic metastasesJ Urol 2008 180(1):1154-60. [Google Scholar]
[6]. GR Mundy, Metastasis to bone: causes, consequences and therapeutic opportunitiesNat Rev Cancer 2002 2:584-93. [Google Scholar]
[7]. JB Nelson, SP Hedican, DJ George, AH Reddi, S Piantadosi, MA Eisenberger, Identification of endothelin-1 in the pathophysiology of metastatic adenocarcinoma of the prostateNat Med 1995 1:944-49. [Google Scholar]
[8]. H Marquardt, MN Lioubin, T Ikeda, Complete amino acid sequence of human transforming growth factor type- β2J Biol Chem 1997 262:12127-30. [Google Scholar]
[9]. E Canalis, M Centrella, T McCarthy, Effects of basic fibroblast growth factor on bone formation in vitroJ Clin Invest 1988 81:1572-77. [Google Scholar]
[10]. M Iwamura, J Hellman, AT Cockett, H Lilja, S Gershagen, Alteration of the hormonal bioactivity of parathyroid hormone-related protein (PTHrP) as a result of limited proteolysis by prostate-specific antigenUrology 1996 48:317-25. [Google Scholar]
[11]. J De La Mata, HL Uy, TA Guise, B Story, BF Boyce, GR Mundy, GD Roodman, Interleukin-6 enhances hypercalcemia and bone resorption mediated by parathyroid hormone-related protein in vivoJ Clin Invest 1995 95:2846-52. [Google Scholar]
[12]. GD Roodman, Role of stromal-derived cytokines and growth factors in bone metastasisCancer 2003 97:733-38. [Google Scholar]