A Comparison of Platelet Count and Enrichment Percentages in the Platelet Rich Plasma (PRP) Obtained Following Preparation by Three Different Methods
Ram Sabarish1, Vamsi Lavu2, Suresh Ranga Rao3
1 Lecturer, Department of Periodontics, Faculty of Dental Sciences, Sri Ramachandra University, Chennai, India.
2 Associate Professor, Department of Periodontics, Faculty of Dental Sciences, Sri Ramachandra University, Chennai, India.
3 Professor and Head, Department of Periodontics, Faculty of Dental Sciences, Sri Ramachandra University, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Suresh Ranga Rao, Professor and Head, Department of Periodontics, Faculty of Dental Sciences, Sri Ramachandra University, Chennai 600116, India.
E-mail: chennaidentist@gmail.com
Introduction: Platelet rich plasma (PRP) represents an easily accessible and rich source of autologous growth factors. Different manual methods for the preparation of PRP have been suggested. Lacuna in knowledge exists about the efficacy of PRP preparation by these different manual methods.
Aims: This study was performed to determine the effects of centrifugation rate revolutions per minute (RPM) and time on the platelet count and enrichment percentages in the concentrates obtained following the three different manual methods of PRP preparation.
Setting and Design: In vitro experimental study.
Materials and Methods: This was an experimental study in which platelet concentration was assessed in the PRP prepared by three different protocols as suggested by Marx R (method 1), Okuda K (method 2) and Landesberg R (method 3). A total of 60 peripheral blood samples, (n=20 per method) were obtained from healthy volunteers. Baseline platelet count was assessed for all the subjects following which PRP was prepared. The platelet count in the PRP was determined using coulter counter (Sysmex XT 2000i).
Statistical Method: The mean of the platelet count obtained and their enrichment percentage were calculated and intergroup comparison was done (Tukey’s HSD test).
Results: The number of platelets and enrichment percentage in PRP prepared by method 1 was higher compared to method 2 and method 3; this difference in platelet concentrates was found to be statistically significant (p < 0.05).
Conclusion: The centrifugation rate and time appear to be important parameters, which influence the platelet yield. Method 1 which had lower centrifugation rate and time yielded a greater platelet count and enrichment percentage.
Centrifugation, Platelet count, Platelet-rich plasma
Introduction
Wound healing is the body’s ability to repair and replace injured or dead cells. It is an absolute prerequisite for survival and can be divided into four overlapping stages: hemostasis, inflammatory, proliferative, and remodeling [1]. The initial response to tissue injury is inflammation, whereby the goal is to provide rapid hemostasis and begin the sequence of events that leads to regeneration of tissue. Platelets play a key role in wound healing and release various growth factors and cytokines that result in cell migration, proliferation, differentiation, and matrix synthesis [2].
PRP is defined as an “autologous concentration of platelets in a small volume of plasma” and is considered to be a rich source of autologous growth factors [2]. The various growth factors present in PRP are Platelet derived growth factor (PDGF), Transforming growth factor beta ( TGF-beta), Vascular endothelial growth factor (VEGF), Epidermal Growth Factor (EGF), Platelet factor 4 (PF-4), Insulin like growth factor-1 (IGF-1), Platelet derived angiogenesis factor (PDAF) [3]. PRP represents a contemporary approach to tissue regeneration and has been found to be a valuable adjunct to promote healing in many oral surgical procedures [4].
The use of PRP in dental surgical procedures could have beneficial outcomes in terms of reduction in bleeding, enhanced soft tissue healing and bone regeneration [5]. Varied methods of preparation of PRP have been reported in the literature. These include commercial systems such as Vivostat ®, PCCS®, Harvest Smart PReP®, Fibrinet ®. Manual methods using laboratory centrifuge have been reported by Marx [6] , Landesberg et al., [7], and Okuda et al., [8]. The clinical effectiveness of each of these methods remains unclear and depends on several variables [9]. The role of centrifugation rate and time on the platelet concentrations achieved in each of the methods has not been evaluated. Thus the objective of this study was to determine the effects of centrifugation rate RPM and time on the platelet numbers in the concentrates obtained following the three different methods of PRP preparation.
Materials and Methods
This was an experimental study in which platelet concentration was assessed in the PRP prepared by using three different protocols.
The sample size was calculated based on the data (difference between mean recovery efficiency in percentage of platelet at different centrifugation times) from a recent study by Perez et al., [10]. Based on the true probability of exposure, inclusion of 18 individuals will be able to reject the null hypothesis (centrifugation rate and time have no influence on the platelet enrichment percentage) with the type I error of 5% and power of 80%. The sample size chosen for the study was 20 individuals.
A total of 60 peripheral blood samples required for the study were obtained from the 20 healthy volunteers. The age range of the subjects included in the study was 18–27 years that comprised of 12 males and 8 females. The subjects who were systemically healthy, not presently under any medications and who had no smoking, alcohol consuming habits were included in the study [7]. An informed consent was obtained from all the participants included in the study. The study was in accordance with the ethical standards of the responsible committee and was approved by the Institutional Ethics Committee of the university.
Blood Sample Collection
Peripheral blood samples were collected from the antecubital fossa of 20 subjects under aseptic conditions. Three samples of venous blood (2 ml each) were drawn in vacutainer containing 0.5 mL of 0.129 mol/L sodium citrate (BD vacutainer, BD Franklin Lakes, NJ, USA) from each of the 20 study subjects which accounted for a total of 60 samples. Baseline platelet counts for all the subjects were assessed using the Coulter counter (Sysmex XT 2000i, Kobe, Japan).
PRP Preparation
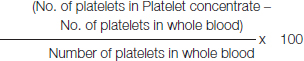
PRP was prepared via a 2 step centrifugation procedures following the protocols suggested by Marx [6], Landesberg et al., [7] and Okuda, et al., [8]. The samples were centrifuged using the laboratory centrifuge (Eppendorf 5810 R, Hanau, Germany) at a constant temperature of 22°C with different centrifugation rate and time. Two spins involved are the separation spin and concentration spin. Following the separation spin, the tube contains all the red blood corpuscles’s at the bottom, above which the buffy coat layer containing the platelets and the white blood corpuscles is present and on top is the plasma. All of the plasma and the buffy coat layer were transferred to an empty tube using a 1 mL pipette. This portion was subjected to the concentration spin. The concentration spin resulted in a clump of cells (platelet concentrate) at the bottom of the tube. The clear supernatant (platelet poor plasma- PPP) was removed with a pipette avoiding disturbance to the underlying platelet concentrate. The remnant PRP was introduced into a coulter counter for platelet count (Sysmex XT 2000i, Kobe, Japan). The above-mentioned procedure [Table/Fig-1] is common for all the tested methods with variations only in centrifugation rate and time of the two spins. The centrifugation rates and times of the different protocols are summarized in [Table/Fig-2]. The mean of Platelet counts obtained in each of these methods was calculated and the enrichment percentage attained by each of these methods was determined as follows:
Flowchart of the PRP preparation methodology
Protocol of PRP preparation by three different methods
| Methods | Separation Spin | Concentration Spin |
|---|
| Rate (Rpm*) | Time (Mts†) | Rate (Rpm*) | Time (Mts†) |
|---|
| Method 1 (Marx et al.,) | 1000 | 4 | 800 | 9 |
| Method 2 (Okuda et al.,) | 2400 | 10 | 3600 | 15 |
| Method 3 (Landesberg et al.,) | 1400 | 10 | 1600 | 10 |
*rpm- revolutions per minute, †mts – minutes

Statistical Analysis
The mean values and frequency were calculated for the demographic variables. Mean values of the platelet number obtained in each of the methods were calculated. Data was analysed with statistical software SPSS version 11. Comparison of platelets concentration at baseline and following centrifugation by different methods was done using Tukey’s HSD test. A p-value of <0.05 was considered as statistically significant.
Results
The demographic data of the study population is summarized in [Table/Fig-3]. A total of 60 samples, 20 samples for each method were analysed. The mean platelet concentration for each method was derived and used for the statistical analysis. Gender distribution was not even, however the difference between the number of platelet in venous blood of males and females was not statistically significant. (p-value = 0.512).
Demographic data of the study population
| Clinical Parameters |
|---|
| AGE Range (years) | 18 – 27 |
| SEX | MALE: 12 FEMALE: 8 |
| OHI (S) SCORE(mean±SD) | 0.629± 0.3 |
| PROBING DEPTH (Mean ± SD) mm | 1.286± 0.1 |
| CAL (Mean±SD) mm | 0.00 ± .00 |
The number of platelets in PRP and enrichment percentage in Method 1 was higher than in Method 2 and Method 3 and the difference in platelet concentrates was found to be statistically significant (p < 0.05) as shown in the [Table/Fig-4].
Intergroup comparison of platelet concentrations and enrichment percentages
| Groups | Mean Platelet Concentration | Percentage of Platelet Yielded as Compared to the Baseline | 95% Confidence Interval | Significance p-value |
|---|
| Lower Limit | Upper Limit |
|---|
| WHOLE BLOOD | 2.18 x 108 | NA | - | - | - |
| METHOD 1 | 3.50 x 108 | 160.26 | -205832.9 | -57567.02 | 0.001 |
| METHOD 2 | 2.60 x 108 | 119.24 | -116182.9 | 32082.98 | .449 |
| METHOD 3 | 2.74 x 108 | 125.53 | -129932.9 | 18332.98 | .206 |
| INTERGROUP COMPARISON | | Mean difference ± SE |
| METHOD 1 | METHOD 2 METHOD 3 | | 89650±282§ 75900±283§ |
‡Significantly different from whole blood (p <0.05)
§Significantly different from method 1 (p <0.05)
Discussion
PRP has been used in recent times for management of intrabony defect [11], gingival recession [12], as a part of tissue engineering protocols [13]. A recent systematic review and meta analysis on the usefulness of autologous platelet concentrates on intrabony defect management revealed that PRP has a significant additive effect when used along with bone grafts for regeneration of intrabony defects [14]. This study was carried out to compare the percentage of platelet enrichment achieved in three PRP preparation protocols suggested by different authors.
The protocol given by Marx [6] achieved highest platelet yield of about 160% above the baseline value. As the centrifugation rate and time were increased as observed in methods suggested by Landesberg et al., [7] and Okuda et al., [8] the platelet yield reduces in a proportional manner. Therefore the results of our study suggest a lower centrifugation rate and time provides higher platelet yield. These findings are in agreement with the observations of Perez et al., [10], wherein the authors also reported lower centrifugation rates favored platelet separation and thereby enrichment. The plausible reason for the reduction in the platelet count at higher centrifugation rate and time would be due to clumping or disintegration of platelets. When such disintegration happens prior to PRP activation, the growth factors are released in an inactive state that may not influence the wound healing process. The enrichment percentage upto 160% was observed in our study, as compared to 200-300% in the previous studies [3,6]. This can be attributed to the fact that we used small volumes of blood (2mL) for each method as compared to the previous studies, where they had used 5 to 10mL of blood. Although several commercial systems are available such as Harvest Smart PReP, Magellan APS system a minimum of 30mL of blood is required for most of the chair side methods. The three methods tested here are widely used as inexpensive chair side methods of PRP preparation involving limited quantity of blood 3- 6mL.
To the best of our knowledge this is the first study comparing the platelet enrichment in the PRP using laboratory centrifuge. The limitation of this study was that the growth factors release was not quantified.
Conclusion
The centrifugation rate and time appear to be important parameters, which influence the platelet yield. This study result provides an insight for the clinicians regarding the platelet concentration achieved by three different techniques thereby allowing them to choose a better and a more reliable method.
‡Significantly different from whole blood (p <0.05)
§Significantly different from method 1 (p <0.05)
[1]. Diegelmann RF, Evans MC, Wound healing: an overview of acute, fibrotic and delayed healingFront Biosci 2004 9:283-89. [Google Scholar]
[2]. Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR, Platelet rich plasmaOral Surg Oral Med Oral Pathol 1998 85:638-46. [Google Scholar]
[3]. Fréchette JP, Martineau I, Gagnon G, Platelet-rich Plasmas: Growth Factor Content and Roles in Wound HealingJ Dent Res 2005 84:434-39. [Google Scholar]
[4]. Lacoste E, Martineau I, Gagnon G, Platelet concentrates effects of calcium and thrombin on endothelial cell proliferation and growth factor releaseJ Periodontol 2003 74:1498-507. [Google Scholar]
[5]. Antonino A, Maria EL, Bianca P, Giuseppina C, Platelet-rich plasma (PRP) in dental and oral surgery: from the wound healing to bone regenerationImmun Ageing 2013 10:23 [Google Scholar]
[6]. Marx RE, Platelet-rich plasma: A source of multiple autologous growth factors for bone graftsIn Tissue Engineering: Applications in Maxillofacial Surgery and Periodontics. Edited by Lynch SE, Genco RJ, Marx RE 1999 ChicagoQuintessence:71-82. [Google Scholar]
[7]. Landesberg R, Roy M, Glickman RS, Quantification of growth factors levels using a simplified method of platelet rich plasma gel preparationJ Oral Maxillofac Surg 2000 58:297-300. [Google Scholar]
[8]. Okuda K, Kawase T, Momose M, Murata M, Saito Y, Suzuki H, Wolff LF, Yoshie H, Platelet-rich plasma contains high levels of platelet derived growth factors and transforming growth factor-β and modulates the proliferation of periodontally related cells in vitroJ Periodontol 2003 74:849-57. [Google Scholar]
[9]. Marx RE, Platelet-rich plasma: evidence to support its useJ Oral Maxillofac Surg 2004 62:489-96. [Google Scholar]
[10]. Perez AG, Lana JF, Rodrigues AA, Luzo AC, Belangero WD, Santana MH, Relevant aspects of centrifugation step in the preparation of platelet-rich plasmaISRN Hematol 2014 2014:176060 [Google Scholar]
[11]. Gupta G, Clinical and radiographic evaluation of intra-bony defects in localized aggressive periodontitis patients with platelet rich plasma/hydroxyapatite graft: A comparative controlled clinical trialContemp Clin Dent 2014 5:445-51. [Google Scholar]
[12]. Naik AR, Ramesh AV, Dwarkanath CD, Naik MS, Chinnappa AB, Use of autologous platelet rich plasma to treat gingival recession in esthetic periodontal surgeryJ Indian Soc Periodontol 2013 17:345-53. [Google Scholar]
[13]. Xu Q, Li B, Yuan L, Dong Z, Zhang H, Wang H, Sun J, Ge S, Jin Y, Combination of platelet-rich plasma within periodontal ligament stem cell sheets enhances cell differentiation and matrix productionJ Tissue Eng Regen Med 2014 [Epub ahead of print] [Google Scholar]
[14]. Panda S, Doraiswamy J, Malaiappan S, Varghese SS, Del Fabbro M, Additive effect of autologous platelet concentrates in treatment of intrabony defects: a systematic review and meta-analysisJ Investig Clin Dent 2014 Jul 22 [Epub ahead of print] [Google Scholar]