Background: The global annual incidence of Tuberculosis (TB) is 9 million cases of which estimated 2.3 million cases occur in India. In many parts of India, the private sector has remained alienated from Directly Observed Treatment Short course (DOTS) implementation; hence, case detection has remained low.
The performance of Taluka Rahata in terms of TB control was poorest before the year 2000; RNTCP was started in Taluka Rahata on 24th March 2001. From 2001-2010, there was improvement in the performance but was not satisfactory.
Hence, present study is an attempt to devise strategy, to increase awareness and involvement of private practitioners in Revised National TB Control Programme in a rural area of Rahata Taluka.
Aim: To adopt strategies to improve the awareness and increase involvement of Private Practitioners about RNTCP in Rahata Taluka of Ahmednagar district.
Setting & Design: It is an Interventional study conducted in Rahata Taluka of District Ahmednagar from June to November by giving personal visits to all the Private Medical Practitioners of Rahata Taluka at their workplace.
Materials and Methods: Personal visit was given to 143 private medical practitioners at their workplace. Workshop used as the major strategy was arranged as per RNTCP guidelines. Health education material was distributed.
Results: Out of the 148 PMPs, 143 could be covered by giving personal visits to their clinic for pre-interventional assessment.110 (76.93%) were males while 33 (23.07%) were females. The mean age of PMPs was 41.60 y. Around 60 percentages of PMPs were non- allopathic practitioners. Sensitization workshop was attended by 132 PMPs. Though no significant difference was observed in their assessment regarding etiology about TB, a significant and highly significant value was obtained after assessing their KAP regarding their diagnosis & referral for sputum diagnosis, categorization and treatment, DOTS provider and TB case management.
Conclusion: The PMPs due to its non-involvement and non-reinforcement are lagging with the update knowledge. The PMPs who have attained their higher qualification before implementation of RNTCP (before year 2001) are in majority unaware of RNTCP
Recommendations: Public-Private partnership involving PMPs & private hospitals need to be strengthened by additional inputs in the form of incentives, free IEC materials and periodic modular training in RNTCP.
Introduction
The global annual incidence of Tuberculosis (TB) is 9 million cases of which estimated 2.3 million cases occur in India [1].
India has one of the largest private health care sectors in the world. This sector is often the first point of contact for a significant number of TB suspects and patients. The strengths of these sectors can be utilized to supplement the government effort to control TB [2].
Private medical practitioners of Allopathic, Ayurveda, Homeopathic, and other alternative systems of Medicine which are to be harnessed in the Programme are grouped under the private sector. The alternative systems of medicine as per planning commission of India also includes registered practitioners under Indian system of Medicine & Homeopathy (ISM&H) such as siddha, unani and therapies such as Yoga and Naturopathy [3,4].
In many parts of India, the private sector has remained alienated from Directly Observed Treatment Short course (DOTS) implementation; hence, case detection has remained low. The case finding and the case holding efficiency of these private medical practitioner agencies is generally poor. Treatment outcomes are also generally poor in this sector. To increase case detection rates, improve successful treatment rates, and reduce out-of-pocket expenditures by patients, it is necessary to involve the private sector in DOTS implementation. Despite the understandable fact that the gaps found between the knowledge & practices of this network of private practitioner have economic and other compulsions, there is a need to make them understand the TB control Programme which is already in vogue and to utilize it in the best interest of reducing the TB burden [5].
Village doctors, especially the private providers are popular because they live in and are a part of the community and are always available in the time of need. Village doctors offer advice that is in line with the cultural beliefs of their patients and, at the same time, prescribe drugs used in modern medicine. More importantly, their services are affordable even to the poor [6].
The private sector is an important source of care even where public services are available. Following issues are of concern in the private sector: Delay in diagnosis; over diagnosis of TB due to overdependence on X-Rays; Use of multiple non- standard regimens for inappropriate durations & Lack of mechanism to ensure the full course of treatment [7].
RNTCP has entered 12th five year plan (2012-2017) with the theme of “Universal access for quality diagnosis and treatment for all TB patients in the community” with a target of reaching the unreached [1].
The performance of Taluka Rahata in terms of TB control was poorest before the year 2000; RNTCP was started in Taluka Rahata on 24th March 2001. From 2001-2005 there was improvement in the performance but was not satisfactory.
Hence, present study is an attempt to devise strategy, to increase awareness and involvement of private practitioners in Revised National TB Control Programme in a rural area of Rahata Taluka.
Aim
To adopt strategies to improve the awareness and increase involvement of Private Practitioners about RNTCP in Rahata Taluka of Ahmednagar district.
Objectives
1. To assess knowledge, awareness and practice about RNTCP among PMPs in Taluka Rahata.
2. To increase awareness by imparting knowledge during sensitization workshop.
3. To assess the level of improvement of knowledge in RNTCP after sensitization workshop.
4. To assess output of sensitization in terms of sputum collection, default rate and cure rate.
5. To motivate practitioners to participate as DOTS providers.
6. To give recommendations to improve participation of Private Practitioners in RNTCP to supplement public private mix.
Materials and Methods
The study is approved by institutional Ethical and Research Committee. It is an interventional study conducted in Rahata Taluka from June to November 2012 by giving personal visits to the doctors of Rahata Taluka at their workplace. Purposive sampling technique was used for selection of Taluka Rahata due to its poor performance. There were 148 Private Practitioners practicing Allopathic, Ayurveda, Homeopathic, and other alternative systems of Medicine in Rahata Taluka.
Exclusion Criteria: PMPs working in collaboration with government service were excluded from the study. Those PMPs who could not be interviewed through personal visits and those who fail to attend the Workshop were excluded from analysis.
Data Collection
Informed consent was obtained from all the participants included in the study.
Pilot Study: A Pilot study was carried out using a pre-designed questionnaire among 23 Private Practitioners by personally interviewing them at their clinic and home and the proforma was thus finalised. Analysis is done in the form of tables, proportions, standard error of difference between two proportions.
Collection of list of Private Practitioners: A list of all the Private Practitioners with their village address was obtained from the Rahata Taluka Association members consisting of President, Vice-President, Secretary and Senior Doctor Members.
Personal visit was made to all the Private Practitioners and their awareness was assessed with the help of filled questionnaire. The Private Practitioner who were left out in a village were called at their contact number provided in the list and were then covered as per their convenient time.
After collecting the questionnaire filled, the Private Practitioner was given a Pamphlet describing the diagnosis and treatment in RNTCP and was briefed about it. Their role and benefit to them as DOTS provider and their patients in terms of TB treatment and control was explained. Their queries were solved in brief.
Total one hundred and forty three (143) Private Practitioners out of one hundred and forty eight (148) were covered through personal interview. It was not possible to include five (05) Private Practitioners, out of which two (02) Private Practitioners from a village did not cooperate in giving time & filling questionnaire even during the second visit, but were provided with an RNTCP pamphlet. One of the PMPs had DOTS Centre attached to his hospital under RNTCP – PPM and was thus excluded. While the remaining two (02) Private Practitioners did not have any contact number and were not having a regular practice, and were not traceable.
Taking into consideration communication, transport facility & availability of Practitioner the workshop place was finalized. The practitioners were busy in the morning hours so the afternoon time was finalized for the workshop. The Intervention was in the form of Workshop as per RNTCP guideline.
Workshop details were mailed to all the Private Practitioners and confirmed telephonically. The Private Practitioners were reminded in the form of telephonic communication and re-reminded through mobile message, a day prior to the workshop.
A one-day workshop was attended by one hundred and thirty two (132) Private Practitioners out of total one hundred and forty eight (143) practitioners practicing in Rahata Taluka.
All delegates were provided with kit containing RNTCP Public Private Mix (PPM) module, RNTCP diagnosis and treatment pamphlets and writing material.
Resource Persons: Speakers were principal investigator, Consultant from World Health Organization (WHO) in RNTCP, Senior faculty from the Department of Community Medicine, TB-Chest and Department of Medicine, District Tuberculosis Officer (DTO), District Health Officer (DHO) &Civil Surgeon (CS). In this way, all the project stake holders were involved.
Duration: The sensitization workshop was conducted for six hours as per RNTCP guidelines [7]. At the end, a half an hour session was kept for discussion.
Post-Intervention: Post-interventional forms were filled by the 132 Private practitioners after five months of workshop by giving personal visits to them at their workplace.
Results
The programme RNTCP in India in 1997 came into existence in Taluka Rahata in 2001, from [Table/Fig-1], it is evident that the PMPs aged more than 35 y have not undergone the course syllabus even among those attaining higher specialization.
Similar finding about the mean age of private GPs was seen in a study conducted by Abdullah A Al-Maniri et al., [8] showed average age of Private Practitioners of 41.3 y. In a study conducted by Uplekar M et al., [9] there were 122 Private Practitioners of which majority were males 95%. The mean age of PMPs in their study was 43 y in rural towns. Another finding observed in a study by Singh TB et al., [10] was that majority of the PPs were in the age group 30-50 y. In the present study there are 60% PMPs in the age group 30-50 y.
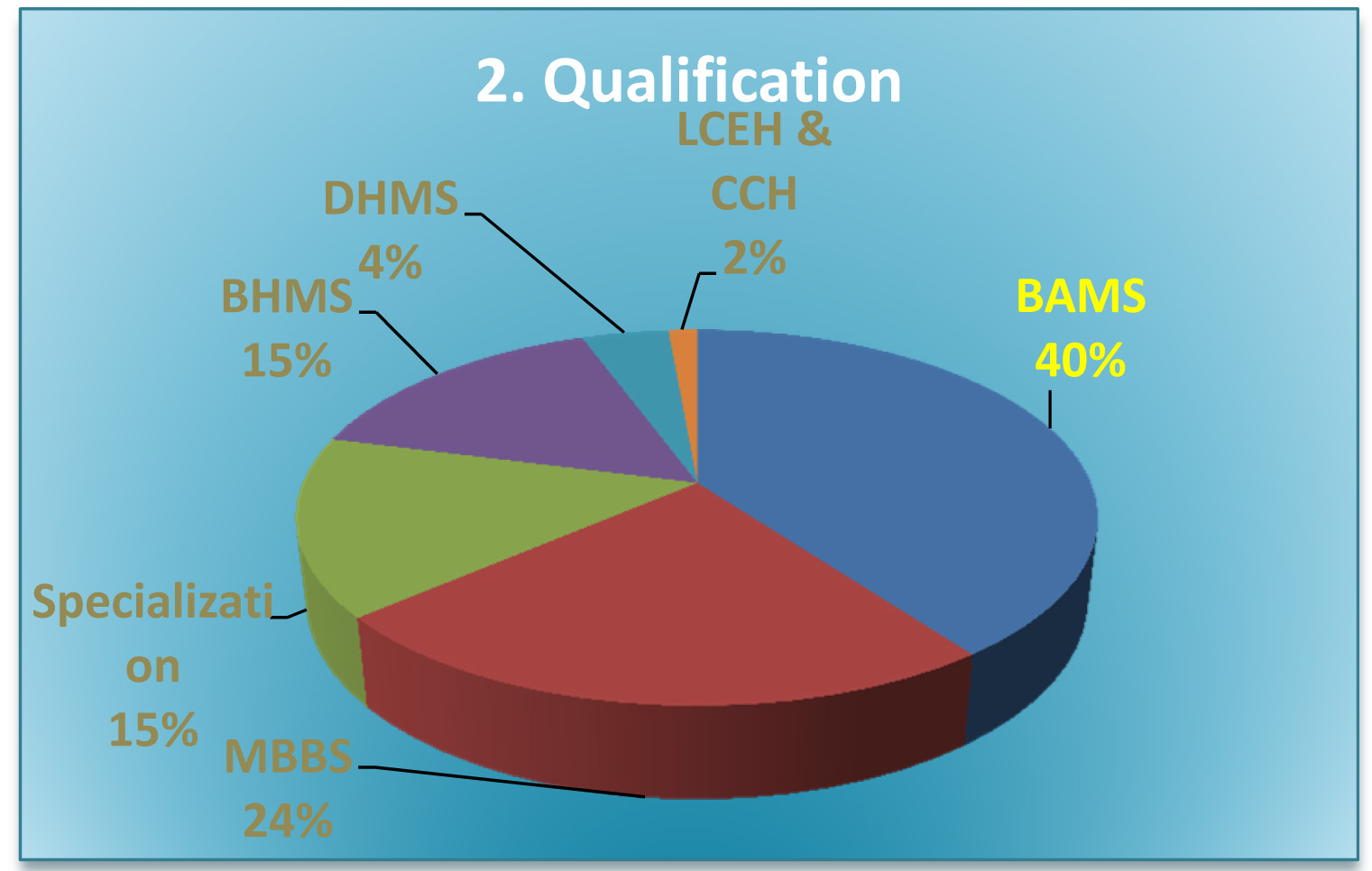
[Table/Fig-2] show that around 61% of PMPs were non- allopathic practitioners.
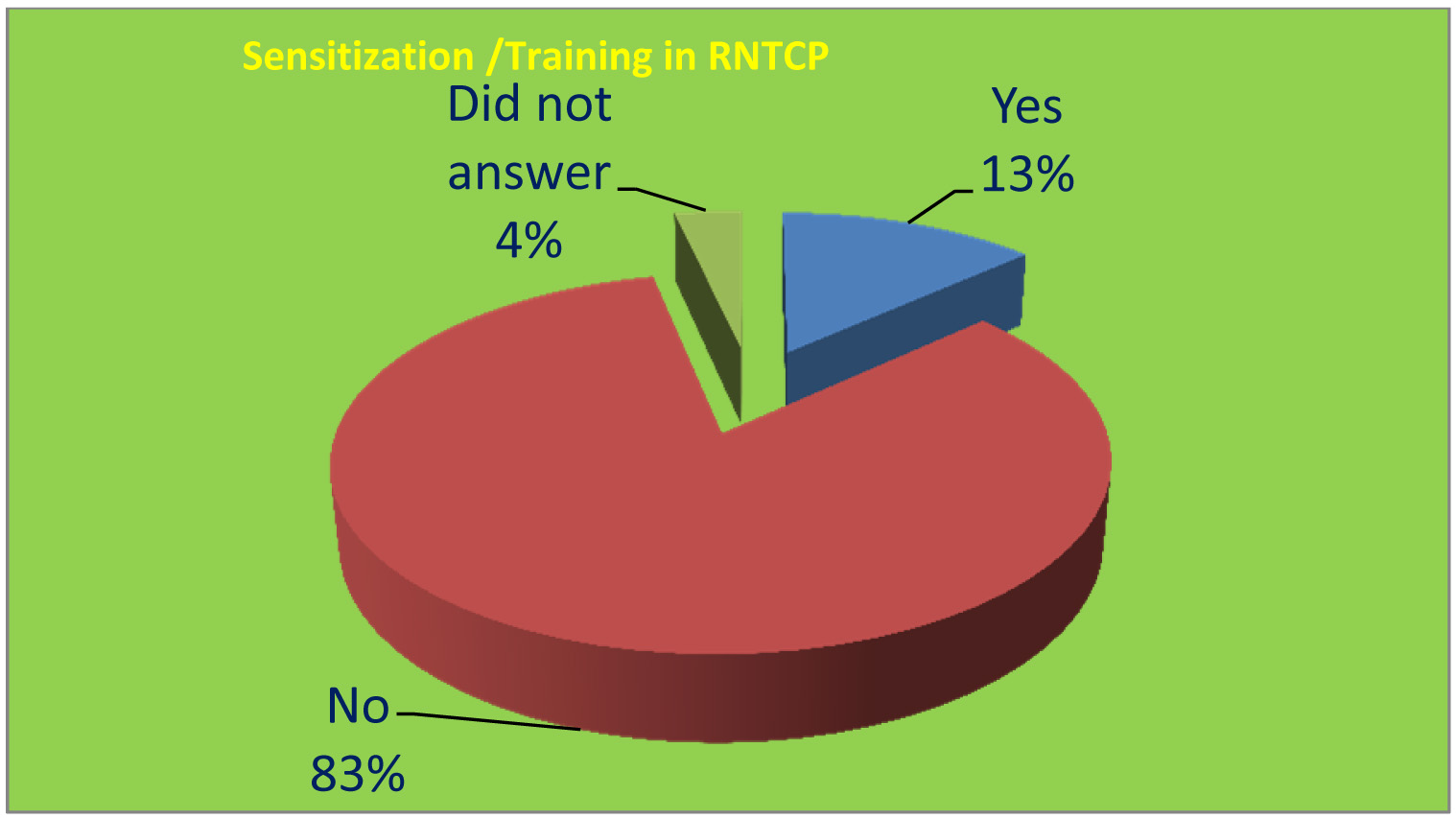
[Table/Fig-3] shows of the 143 PMPs, 19 (13.28%) said they were sensitized in RNTCP. Out of these 16 PMPs were briefed by the DTO during the visit but their sensitization was not as per RNTCP guidelines and remaining 3 PMPs mentioned yes and explained newspaper and TV as the reason for their sensitization.
Since 132 PMPs attended the training, hence further analysis is done excluding the remaining 11 PMPs who failed to attend the interventional RNTCP workshop.
From [Table/Fig-4], (1.51%) PMPs mentioned the cause to be genetic disorder.
In the post-interventional assessment of knowledge,132 (100%) of PMPs mentioned that TB is caused by the bacilli Mycobacterium Tuberculosis even though there was no statistical difference found in the knowledge after applying z test for standard error of difference between two proportions.
[Table/Fig-5]reveals that out of 132 PMPs only 19 (14.39 %) PMPs during the pre-interventional correctly answered the full form of DOTS. In the post- interventional assessment 116 (87.87%) of the PMPs correctly answered the full form of DOTS.
After applying z-test for standard error of difference between two proportions a highly significant association was found between the knowledge of PMPs about the full form of DOTS.
The above [Table/Fig-6] shows out of the 132 PMPs,121 (91.66%) of the PMPs during the pre-interventional assessment mentioned that TB can be treated by Allopathy. In the post-interventional assessment 129 (97.72%) of the PMPs out of 132 mentioned Allopathy as the system of medicine for treating TB. After applying z-test for standard error of difference between two proportions a significant difference was found between the knowledge of PMPs regarding the system of medicine used for treating TB.
Above [Table/Fig-7] shows out of 132 PMPs 71 (53.78%) PMPs suggested during pre-interventional finding that the duration of cough in a suspected pulmonary TB patient to be two weeks or more associated with or without sputum.
Post-interventional finding showed that out of 132 PMP 128 (96.96%) PMP correctly suggested the duration of cough. After applying z-test for standard error of difference between two proportions a highly significant difference was observed in the knowledge of PMPs according to the duration of cough in a suspected pulmonary TB patient both before and after intervention. Regarding the first investigation done in a suspected pulmonary TB patient, 48 (36.66 %) PMPs before attending the work shop mentioned chest X-ray thus denoting lack of update in their knowledge in RNTCP.
After applying z-test for standard error of difference between two proportions a highly significant difference was observed in the knowledge of PMPs according to first investigation advised in a suspected pulmonary TB patient.
Treatment wise distribution of PMPs: There was a highly significant difference found in the knowledge and practice of PMP regarding their assessment about the treatment wise distribution after a z-test for standard error of difference between two proportions was applied. Only 39 (29.54%) PMPs in pre-intervention knew about all the five first line drugs in RNTCP, the likely reason for small number of respondents may be the recall bias. Whereas in the post-intervention, 130 (98.48%) PMPs mentioned their names correctly. 43 (32.57 %) PMP mentioned the correct relation of meals for administering anti-TB drugs. All the PMP showed their willingness to use free Anti-TB drug supply from the government.
In the pre-workshop assessment, out of 132 PMP only 19 (14.39 %) PMP categorize their patients. Where as in the post- workshop assessment out of 132 PMP 112 (84.84%) PMP mentioned that they can now categorize the patients and a highly significant difference of gaining knowledge was observed after the workshop (z-value 17.07).
92 (69.69%) PMP in the pre-workshop mentioned that there is a need to hospitalize only seriously ill TB patients. Where as in the post-intervention, out of 132 PMP 121 (91.66%) PMP mentioned their need to hospitalize only seriously ill TB patients.
Only 49 (37.12%) of PMP mentioned that the TB treatment duration is 6 to 8 mnth. After five months of assessment, out of 132 PMP 129 (97.72%) PMP mentioned 6 to 8 mnth usual duration of TB treatment.
Distribution of PMP according to their knowledge about DOTS provider: Out of 132, 79 (59.84 %) PMPs knew about DOTS provider. (100%) mentioned about the DOTS provider information during their follow-up assessment. Z-value was 10.78.
Distribution of PMP in relation to their knowledge regarding Categorization in RNTCP: Seventy nine (59.84%) PMPs in pre-workshop assessment correctly mentioned the Cat-I regimen. Whereas during post-workshop assessment, out of 132 PMPs 126 (95.45%) PMPs mentioned about the regimen of Cat-I.
Out of 132 PMPs 77 (58.33 %) PMPs mentioned about the action to be taken in patients on Cat-I who are found smear positive at the end of treatment should be to label them as a case of failure and put them on Cat-II. After the interventional sensitization 124 (93.93%) PMPs out of 132 mentioned about putting the patients on Cat-II after labelling the patients as failure. No other study was found for comparison. After applying z-test for standard error of difference between two proportions a highly significant difference was observed about the knowledge of PMPs regarding Category-I.
Regarding distribution of PMPs in relation to their knowledge about Cat-II, out of 132 PMPs 80 (60.60%) PMPs correctly mentioned about types of patient categorized in Cat-II. In the post-workshop of five months follow-up assessment, 126 (95.45%) PMPs responded by answering about smear positive relapse, failure and treatment after default patients to be categorized in Cat-II.
After applying z-test for standard error of difference between two proportions highly significant difference was observed in the knowledge of PMPs about the type of TB patient categorized in Cat-II (z-value = 8.74).
Distribution of PMP in relation to their attitude & practice about TB case management
Eighty nine (67.42%) PMPs in pre-workshop visit mentioned that sputum smear examination is done by Ziehl Neelson staining. In the post-workshop visit after five months, out of 132 PMPs 128 (96.96%) mentioned the statement to be false that smear examination is not done by ZN staining.
Ninety eight (74.24%) PMPs correctly mentioned TB as an opportunistic infection in HIV/AIDS patients. Whereas, in the post-workshop all of the PMPs (100%) mentioned that TB is an opportunistic disease in HIV/AIDS patients. After applying z-test for standard error of difference between two proportions highly significant difference was observed in the distribution of PMP in relation to their attitude & practice about TB case management.
A highly significant difference was found after applying standard error of difference between two proportions to assess the knowledge regarding spread and need for hospitalization as follows. 96 (72.72%) PMPs during pre-intervention assessment mentioned about the type of TB infecting 10-15 persons per year as smear +ve pulmonary TB. In the post-intervention assessment, out of 132 PMPs 123 (93.18%) PMPs correctly mentioned smear positive pulmonary TB infecting 10-15 persons annually if left untreated.
Out of 132 PMPs 79 (59.84%) PMPs mentioned that hospitalization in a case of TB is required only for Pneumothorax. In the post-workshop follow-up visit, 123 (93.18%) PMPs from the given alternative correctly mentioned Pneumothorax as the cause for admission in a TB patient (z-value was 5.85).
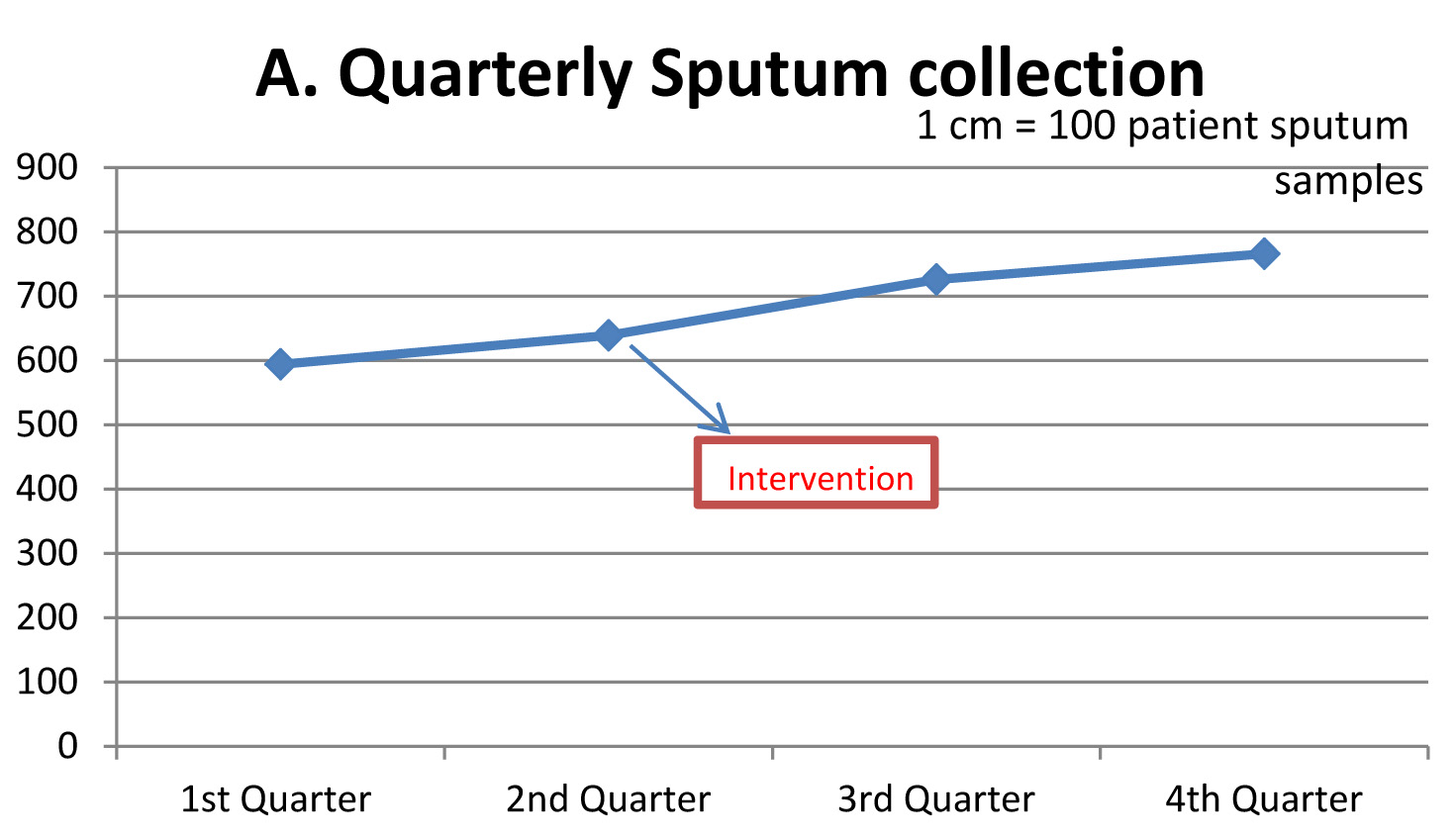
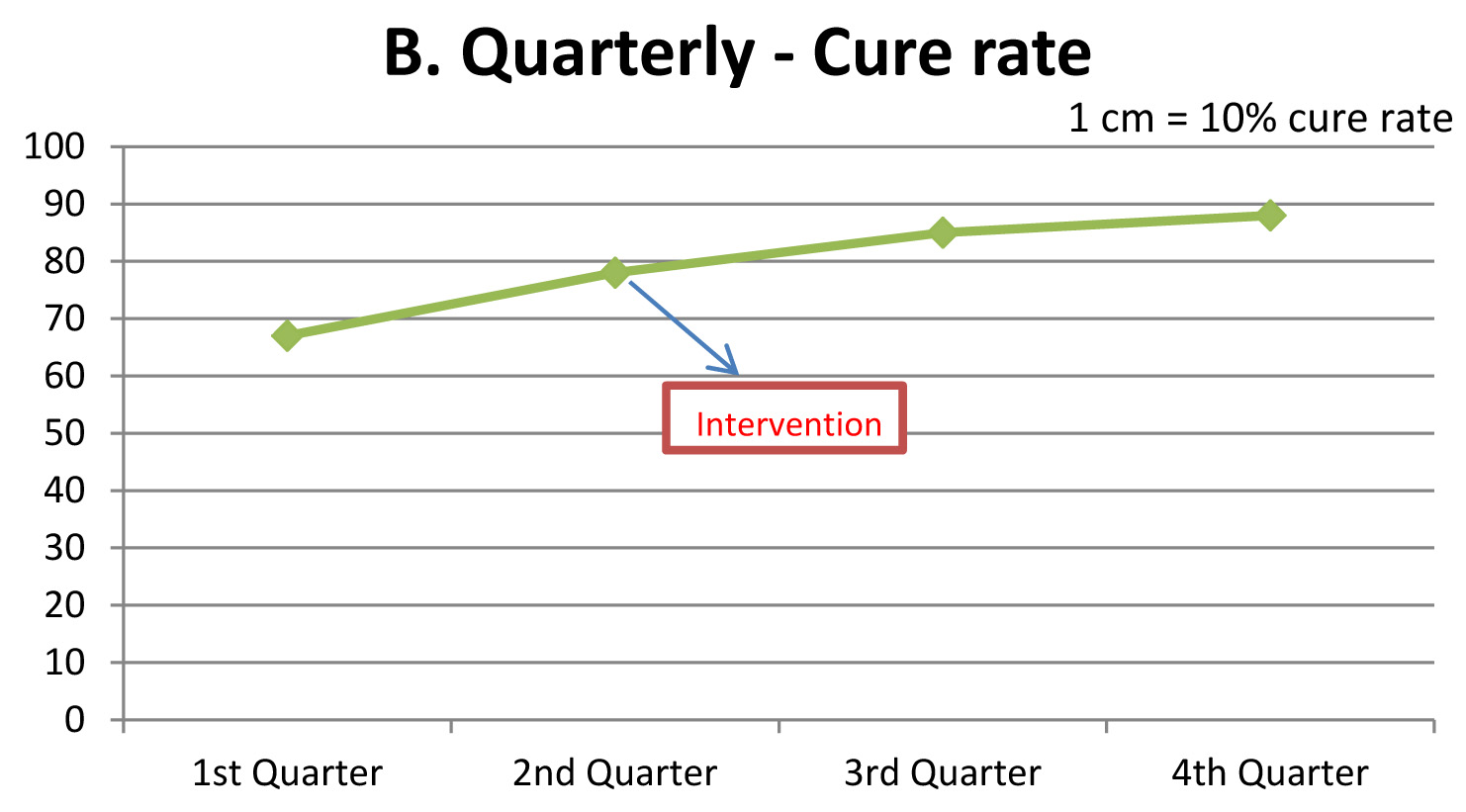
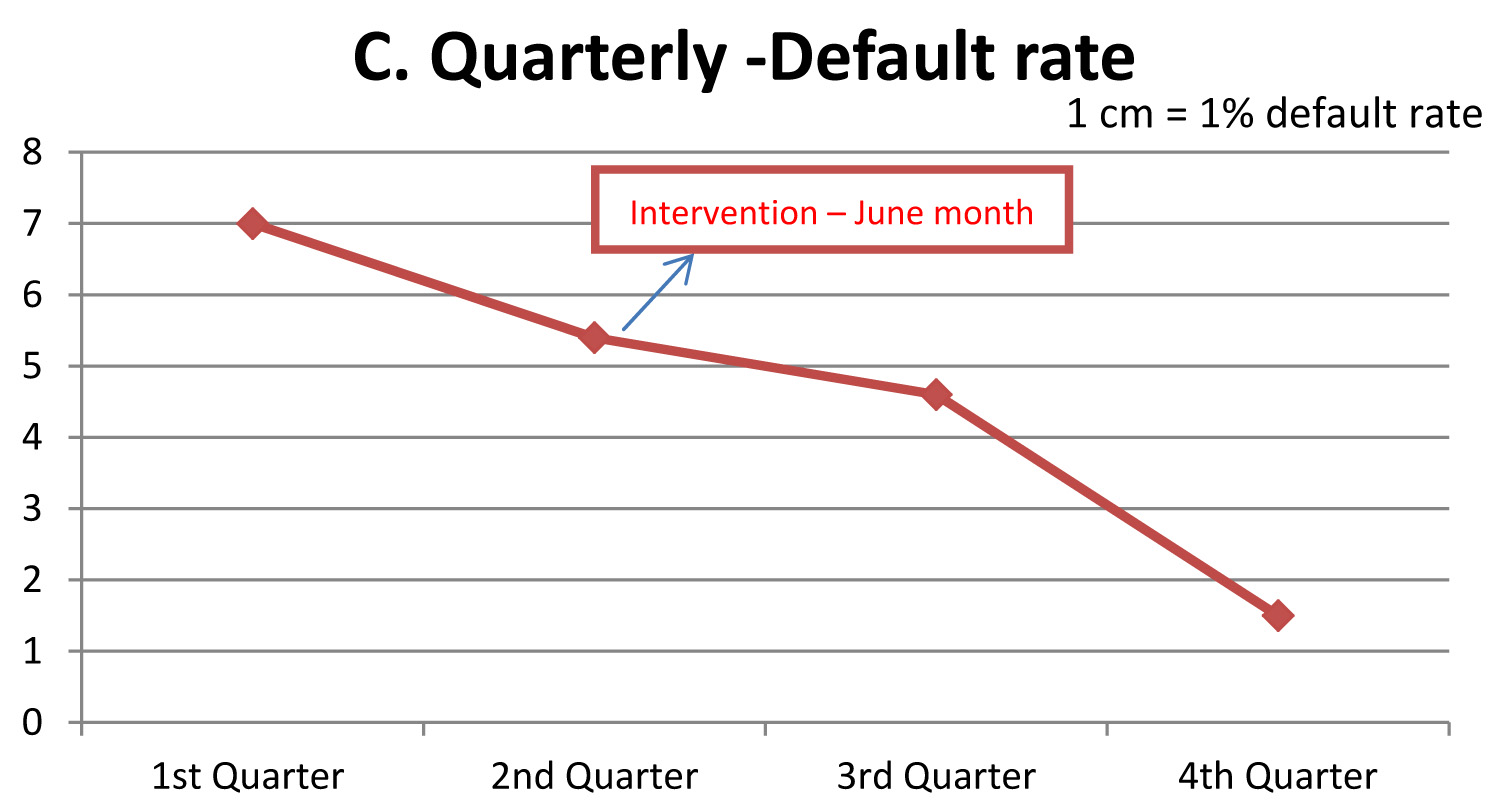
Quarterly Report of Rahata Tuberculosis unit (TU) from 1st Quarter to 4th Quarter showing line diagram: A. Sputum collection B. Cure rate and C. Default rate [Table/Fig-8-10].
From the above [Table/Fig-8,Table/Fig-9,Table/Fig-10] information obtained from Rahata TB Unit (TU) & district TB centre, it is clear that there is a slight increase in sputum collection, cure rate and decrease in trend in the default rate in the 3rd and 4th quarter. The rise in sputum collection from 594 to 766 and cure rate from 67% to 88% and decrease in default rate from 7% to 1.5% in the 4th quarter reported after five months of intervention may be linked to the intervention in the form of workshop attended by the PMPs at the end of the 2nd quarter in the month of end of June. In the absence of intervention in the form of workshop the outcome expected would have been the same as in the 1st and 2nd quarters.
The PMPs among which more than 60% of doctors were non-allopathic working in rural villages of the Taluka were also told about their role as DOTS provider in the benefit of their patients by utilizing free Anti-TB treatment and their personal gain in terms of receiving incentive and achieving name behind the completion of each TB case treatment. All the PMPs including these non – allopathic practitioners had agreed to practice this through RNTCP. It is therefore an important part of the policy in the future to involve and bring all these non-allopathic doctors into the loop of RNTCP.
Age and sex wise distribution of Private Medical Practitioners (PMP) Mean age = 41.60 y
| Age (y) | Sex | Total No. Percentage (%) |
|---|
| Male | Female |
|---|
| 25-29 | 06 | 12 | 18 (12.58) |
| 30-34 | 22 | 13 | 35 (24.47) |
| 35-39 | 15 | 02 | 17 (11.88) |
| 40-44 | 17 | 02 | 19 (13.28) |
| 45-49 | 13 | 02 | 15 (10.48) |
| 50-54 | 14 | 02 | 16 (11.18) |
| 55-59 | 11 | 00 | 11 (7.69) |
| 60-64 | 09 | 00 | 09 (6.29) |
| 65-69 | 02 | 00 | 02 (1.39) |
| 70-74 | 01 | 00 | 01 (0.69) |
| TOTAL | 110 (76.93%) | 33 (23.07%) | 143 (100) |
Qualification wise distribution of Private Medical PractitionersNote: LCEH= licentiate in the court of examiners in homeopathy, CCH= certified in classical homeopathy
Distribution of Private Medical Practitioners according to their sensitization /Training in RNTCP
Distribution of PMP according to the Knowledge about aetiology of TB z value = 1.44
| Cause of TB | Pre-interventional assessment | Post- interventional assessment |
|---|
| No. % | No. % |
|---|
| Mycobacterium Tuberculi | 130 (98.48) | 132 (100) |
| Genetic disorder | 02 (1.51) | 00 (00) |
| Total | 132 (100) | 132 (100) |
Distribution of PMP according to their Knowledge about full form of DOTS
z value = 18.60
| Correct full form of DOTS | Pre-workshop assessment | Post- workshop assessment |
|---|
| NO % | NO % |
|---|
| Correct answer and answer signifying similar meaning | 19 (14.39) | 116 (87.87) |
| Incorrect answer | 68 (51.51) | 12 (9.09) |
| Did not answer | 45 (34.09) | 4 (3.03) |
| Total | 132 (100) | 132 (100) |
Distribution of PMP according to their knowledge and practice about system of medicine used for treating TB
z value = 2.33
| Pathy used for treating TB | Pre-interventional assessment | Post-interventional assessment |
|---|
| No. % | No. % |
|---|
| Allopathy | 121 (91.66) | 129 (97.72) |
| Both Ayurveda and Homeopathy | 06 (4.54) | 00 (00) |
| Both Allopathy and Ayurveda
| 01(0.75) | 00 (00) |
| Ayurveda | 02 (1.51) | 00 (00) |
| Homeopathy | 01 (0.75) | 00 (00) |
| Did not answer | 01 (0.75) | 03 (2.27) |
| Total | 132(100) | 132(100) |
Legalknowledgebasedonnursingqualification
| Sr No | Diagnosis and referral of TB patients/ suspects | Pre-interventional assessment | Post-interventional assessment | z value |
|---|
| No. (%) | No. (%) |
|---|
| 1 | Cough 2 or more weeks associated with/without sputum | 71 (53.78) | 128 (96.96) | 10.67 |
| 2 | First investigation advised in a suspected pulmonary TB patient in the form of sputum collection | 84 (58.74) | 132 (100) | 10.03 |
| 3 | Collect sputum samples in a suspected TB patient |
| a. Yes | 54 (40.90) | 111 (84.09) | 8.89 |
| b. No | 66 (50) | 17 (12.87) | |
| c. did not answer | 12 (9.09) | 04 (3.03) | |
| 4 | Number of sputum samples collected for examination |
| One | 09 (6.81) | 00 (00) | |
| Two | 43 (32.57) | 125 (94.69) | 15.03 |
| Three | 71 (53.78) | 128 (96.96) | |
| Four | 02 (1.51) | 00 (00) | |
| Did not answer | 07 (5.30) | 04 (3.03) | |
| 5 | No. of PMPs advising suspected pulmonary TB sputum samples to be examined at other laboratories |
| Govt. health care facility (PHC, RH), tertiary insti. | 111 (84.09) | 129 (97.72) | 5.41 |
| Private practitioner | 03 (2.27) | 03 (2.27) | |
| Do not refer | 13 (9.84) | 00 (00) | |
| Continue with Anti-TB treatment | 02 (1.51) | 00 (00) | |
| Did not answer | 03 (2.27) | 01 (0.75) | |
Quarterly sputum collection (A)
Quarterly Default rate (C)
Conclusion
Unlike the practitioner in Public health sector or under Ministry of health at state government, the PMPs due to its non-involvement and non-reinforcement is lagging with the update knowledge. The PMPs who have attained their higher qualification before implementation of RNTCP are in majority unaware of updates in TB case management and the RNTCP.
Recommendations
Public-Private partnership involving PMPs & private hospitals need to be strengthened by additional inputs in the form of incentives, free IEC materials and periodic modular training in RNTCP.
RNTCP must be an integral part of undergraduate and postgraduate curriculum for MBBS, Nursing and Non-allopathic fields such as BAMS & BHMS as this is an important public health problem. This decision has to be taken at health university level.
During internship training programme interns must be oriented and trained in RNTCP. Regular CMEs & Workshops must be organized for PMPs of all system of medicines involving local IMA branches.
It is also essential to observe ethical principles of medical practice since there are lucrative offers by pharmaceutical companies in view of reduced sale of Anti-TB drugs due to successful implementation of RNTCP.
Practitioners who completed their graduation before 2000 are less likely to have knowledge about RNTCP and DOTS; therefore all such practitioners need to be sensitized.
Intensive IEC activities for general population & private practitioners with mass media like print and electronic about free availability of DOTS and diagnostic facilities all over the country and the sites where these facilities are available.