Objective: To identify the reported morbidity profile of people according to age, gender and organ system affected using International Classification of Diseases (ICD) coding, in a demographically defined area in Tamil Nadu in order to identify their health care needs and to plan appropriate interventions strategies.
Materials and Methods: This is a-cross sectional study using a convenience sample of 12308 persons sceened from the 41 panchayat units of the Kattankulathur block, comprising 90 villages with a population of about 2,00,890, over a period of one year. Diagnosis made were coded using ICD 10 version and data collected was analysed by appropriate statistical methods to explain the distribution of morbidity profile among the study population.
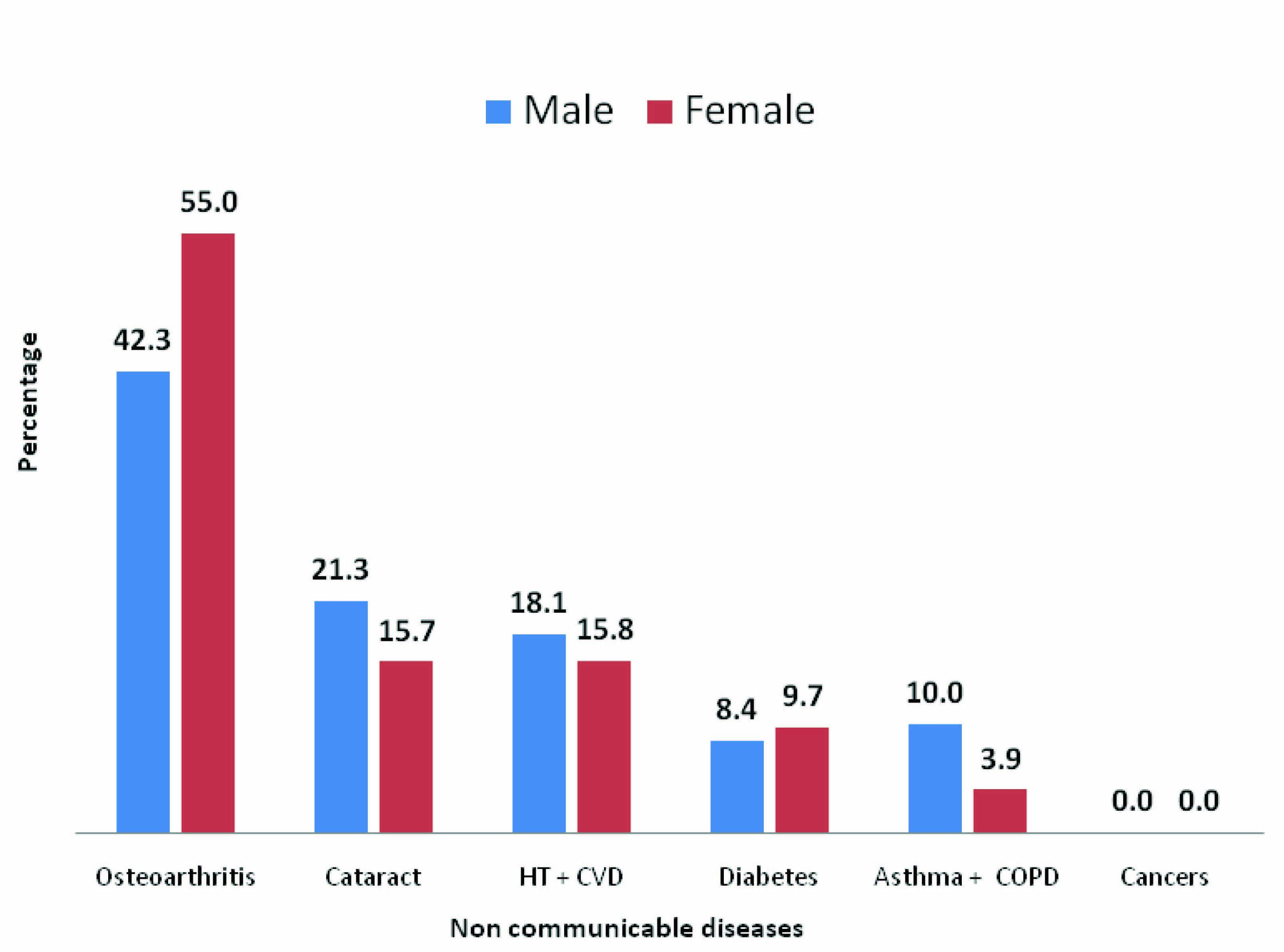
Result: Out of total, 38.1% screened were males and 61.9% were females. Underfives were 5.3%, school going children 43.3%, adults 39.2% and elderly 12.3%. Majority had illness affecting respiratory system (20%), ‘symptoms and signs’ (19%), musculo-skeletal system (16.1%) and digestive system(11.9%). ‘Symptoms and signs’ classification, is a group of conditions which is of nonspecific diseases, signs, symptoms, abnormal findings and complaints, apart from the system specific conditions diagnosed properly and not elsewhere classified, More males were affeced with respiratory, digestive and illnesses with ‘symptoms and signs’ while more women were affected with musculo-skeletal problems. Only 9.7 % of patients reported with non-communicable diseases. Among them, 55 % women and 42.3 % men had osteoarthritis and 15.7 % women and 21.3 % men had cataract. About 15.8 % women and 18.1 % men had hypertension and other heart diseases while 9.7 % women and 8.4 % men had diabetes and 10.0 % men and 3.9 % women had chronic respiratory diseases.
Conclusion: School going children and adults have higher levels of morbidity when compared to elderly and under five children. More females reported with illness but morbidity was found to be higher among males. The burden of illness increased with age. Acute ailments were responsible for high morbidity among children, while chronic ailments caused high morbidity among the elderly.
Introduction
The health of an individual does have a direct relationship with human resources development and economic development of a nation. From the time of Alma Ata declaration to achieve "Health for All by 2000", lot of planning, effort and public expenditure had been devoted to improve the health of the people both in rural and urban areas in India. Further, the spread and accessibility of medical care has also improved substantially across the country. However, inspite of these efforts, India is one of the many developing countries, which have high levels of morbidity [1]. The current health scenario in India is often described as “dismal” or “disturbing”. Except a few states like Kerala, Goa and Tamil Nadu which have done relatively well, the situation in most parts of the country is a cause for worry. Going by present trends, India is in danger of missing the health targets set by the Millennium Development Goals [2].
However, India has made significant progress in improving the health conditions of its population. While there has been a general decrease in mortality leading to significant gains in life expectancy, what has happened to morbidity is yet to be assessed. Very little information is available about the disease profile of different population groups in India. The level and prevalent pattern of morbidity in the country show that India has entered into the fourth stage of health transition [3]. Due to industrialization and the persisting inequality in health status between and within States and Union Territories (due to varying economic, social and political reasons), India currently face a “Triple burden of diseases”, which are the unfinished agenda of communicable diseases, emerging non-communicable diseases related to lifestyles and emerging infectious diseases [4].
In the last decades, India has experienced improvements in the nutritional status, health infrastructure, social development and control of major killer diseases. But inter-state, urban-rural, male-female inequalities are clearly viewed as a major public health challenge in this country [5]. There is a wide variation in the morbidity profile of the people in different States as well as within the States. For example comparing reported morbidity in states like Kerala and Bihar and the all India statistics showed that the proportion reported as ailing was about 25% in Kerala, and a low of 5% in Bihar and about 9% at the all-India level. In Kerala, the level of morbidity was also high when copmared to other Indian States [6,7]. Another challenge is the inequitable distribution of the population between urban and rural areas. Over 68% of the population lives in rural areas. The target of “Better Health for all in the 21st century” is most difficult to achieve in the rural areas where the majority of the poor people live [8].
Tamil Nadu have done relatively well in planning, implementation and evaluation of Medical and Public Health intervention programs when compared to other States. This achievements are clearly visible from the reduced morbidity and mortality profile based on the reported 2011 census data for all vital events in the State [9]. Literature search about the morbidity profile / disease burden of varying population groups in Tamil Nadu shows very little information with specific morbidity profiling. Considering the diverse nature of the State, there are some limitations in arriving at the exact nature of the illness pattern in a specified geographical area.
An earlier study carried out to assess the morbidity pattern and nutritional status among elderly residing in the present study area and population showed that the burden of chronic diseases was high among them while communicable diseases burden was found to be low. Overweight and obesity were reported high among females and characteristically prevalence of underweight increases with the advancing age [10]. With these background, this study was planned with the main objective of identifying the reported morbidity profile of people, living in a demographically defined area of Kattankulathur block in Kancheepuram District of Tamil Nadu, India using the International Classification of Diseases [ICD] coding, according to age, gender and organ system affected, in order to identify the health care needs and also to plan appropriate interventions to supplement and strengthen the existing health care delivery system in the area.
Materials and Methods
Study design: This is a population based cross-sectional study and was conducted in the Kattankulathur block of Kancheepuram District of Tamil Nadu State, India. Health screening camps were conducted in all the 41 panchayaths units of the Kattankulathur block in Kancheepuram District of Tamil Nadu, India comprising 90 villages and covering about 2,00,890 population, over a period of one year (Jan 2011- Dec 2011). This study area and population comes under the field practice area of SRM Medical College Hospital and Research Centre. The study population identified was any male or female residing in the study area at the time of the study period. This cross-sectional study was carried out using the convenience sampling method. A total of 12308 persons (approximately 6.13% of the total population in the block) who attended the health checkup camps were screened during this one year period. Wide publicity was given in the camp area 2-3 days prior to the camp date to mobilize maximum people suffering from illnesses. All those individuals who attended the camps were interviewed in person with a structured interview schedule to elicit information on select socio-demographic variables, habits, dietary intake, and treatment history. Apart from this, those who attended the camps were screened, by doing necessary anthropometric and clinical assessment by the different specialists. Specialists from the hospital were part of the medical team which is supported by the necessary paramedical staff. Demographic information, clinical examination findings and anthropometric measurements were recorded for all persons and all the relevant findings are recorded in an index card. The provisional diagnosis made by clinicians was coded using International Classification of Diseases [10,11].
Statistical Analysis
Data collected were entered into Microsoft Excel spread sheet and analysed using SPSS version 17 software. Descriptive data tables were generated to elaborate the findings and appropriate statistical analysis was used to explain the distribution of morbidity profile among the study population.
Ethical and financial consideration: All the individuals who attended the camp were included in this study and were briefed about the purpose of data collection and written informed consent was obtained from them. The study was approved by the Institutional Ethics Committee. All the materials, man power and other resources needed for conducting the camps were provided by the Institution as part of the logistics support.
Results
The data collected were analysed for studying the morbidity profile of the 12308 population covered in the study area. On an average 300 persons were screened during each of the 41 camps conducted which is spread out to cover all the 41 panchayats in the Kattankulathur block of Kancheepuram district of Tamil Nadu. Among those screened, 38.1% were males and 61.9% were females, underfives were 5.3%, school going children were 43.3%, adults were 39.2% and the elderly were 12.3%.
The diseases diagnosed were classified as per the ICD 10 and were tabulated in [Table/Fig-1], based on the organ systems involved and in the order of illness burden. The result shows that majority of the people had illness affecting the respiratory system, ‘symptoms & signs’, musculo-skeletal system and digestive system in the order of the proportion affected. ‘Symptoms and Signs’ classification, is a group of conditions which is of nonspecific diseases, signs, symptoms, abnormal findings, complaints, social circumstances and external causes of injury or diseases, apart from the system specific conditions diagnosed properly and not elsewhere classified, (as per ICD-10: Chapter XVIII: R00-R69: Symptoms, signs and abnormal clinical and laboratory findings). More male patients were affeced with respiratory, digestive and illnesses with signs and symptoms category when compared to women, while more women were affected with musculo-skeletal problems when compared to males. The other significant systems involved in this study group were skin, infections, eye and genito urinary system. Nearly 10% of the persons screened were found to be apparently healthy. Nearly 19% of the people were found to be suffering from non-specific illnessess which were not been classified under any other system. They constituted a major proportion of the people reported with ‘signs and symptoms’ affecting different parts of the body which needs further evaluation or follow up to determine the causes.
The [Table/Fig-2] shows the System subgroup and sex wise distribution of morbidity pattern with details about the commonly occuring illnesses with which they came for the screening camp. In the respiratory system category, upper respiratory infections were the most commonly occuring problem where males and females were affected almost equally. Lower respiratory infections, asthma and chronic obstructive pulmonary diseases were the other major respiratory illnesses reported. In the signs and symptoms category, fever was found to be the major symptom with which the patients came followed by head ache. Males and females were equally found to be suffering from fever, while more females were suffering from headache when compared to males. Abdominal pain, giddiness and chest pain were also very frequently reported by both male and female patients.
In the musculo-skeletal system, myalgia was the most commonly reported problem among males and females alike. Osteoarthritis and low back pain were the other major reported problems followed by spondylitis and inter vertebral disc prolapse. Among the digestive system disorders, dental caries was the most commonly affected probem followed by acid peptic diseases and gingivitis. More males were affected with dental caries while more women were affected with acid peptic diseases. Under skin conditions, majority of the patients were found to be suffering from skin infections while other skin conditions were excema, dermatitis/urticaria, skin appendages and other dermatological conditions.
Under the Infection and parasitic diseases category, worm infestations were found to be the maximum followed by Gastro Intestinal Tract infections like diarrhoea, dysentery etc. Few of the patients were suffering from scabies and pulmonary tuberculosis. High worm infestation load is identified among the school going children between the age group of 5 y to leass than 15 y. Among diseases of the eye, refractive errors contributed to the majority of the problem followed by cataract. Both these conditions were almost equally distributed among males and females and was found to be highest among the elderly followed by the adult group.
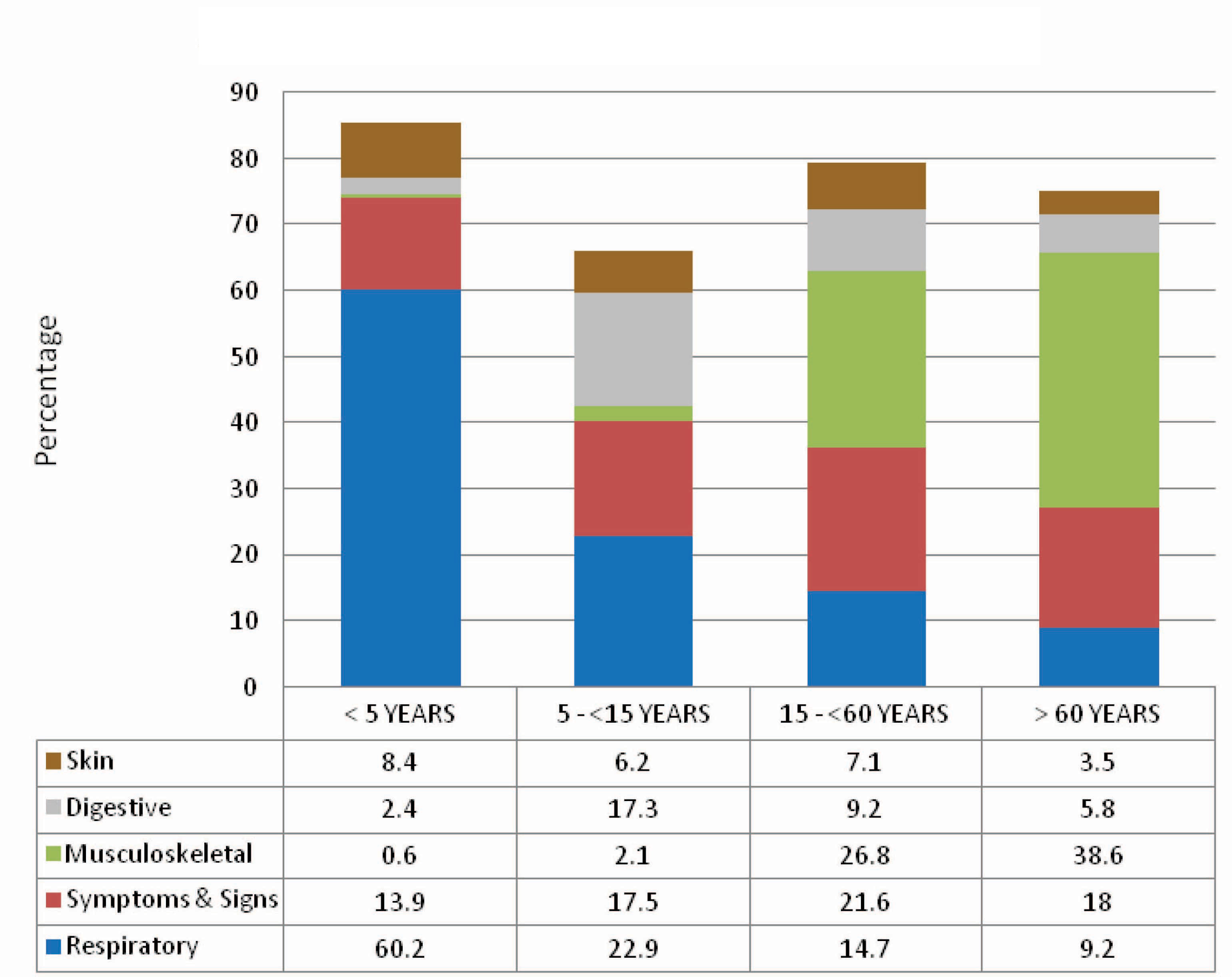
[Table/Fig-3] shows the system and age wise distribution of morbidity profile among the study population. The incidence of respiratory illness is mostly reported among the underfive age group and the incidence tapers as age advances and was less among the elderly people. In the category of patients grouped under ‘symptoms and signs’, the distribution was found to be with minimum difference among different age groups like adults, elderly, underfives and school going children.
Among those affected with musculo-skeletal system, there seems to be a progressive increase of illnesses as age advances. Digestive system disorders were reported more among the school going children while skin conditions affeced almost equally in all groups except in elderly which is slightly less when compared to other age groups. Eye problems were reported more among the elderly followed by the adult population. Refractive errors seems to be the major problem followed by cataract. Common infections and parasitic diseases were reported relatively more among the underfives and school children when compared to the adult and elderly population.
This study shows that only 9.7 % [1198] of the patients reported with non communicable diseases [Table/Fig-4]. Among them majority of the patients were affected with osteoarthritis, cataract, hypertension and other cardio vascular diseases, diabetes, chronic respiratory diseases like asthma and chronic obstructive pulmonary diseases. No cancer patients were seen in the screeening camps or any person suspected to be suffering from pre-cancerous conditions reported to the camps.
Discussion
The study conducted with the main objectives of identifying the reported morbidity profile of people living in the Kattankulathur Block have shown very interesting pattern of the reported illness burden of the area. There seems to be a predominatly female populations attending the camps as is evident from several other studies conducted in India as well as other countries. A study conducted to identify the morbidity patterns in Kerala showed higher levels of morbidity among females. Females are found to have higher risk for diseases of bones and joints, and hypertension than males; females being two times prone for these diseases when compared to the males [7]. In another study the proportion as ailing in Kerala varied from 16% in adolescents to 58% in the elderly and the risk of reporting as ill was only marginally higher in females than in males. A larger proportion of male children were falling sick than female children. Greater vulnerability to illness in women begin with the early-working-age group, peaked in the late working ages and diminished in older ages and health in females deteriorated earlier than in males. The likelihood of illness was 3.6 times more among the elderly than among children and gender differences were insignificant [6].
Regarding the age wise distribution of morbidity pattern, it is found that school going children in the age fgroup of 5 to 15 y have the highest diseease burden followed by the adults, elderly and the underfives. A Soweto study showed that the majority of patients were in the 20 to 50 year age group, followed by those under ten years of age [12]. Another study in Sousse, Tunisia showed that there was a predominance of females (62%) and a relatively young population attending the primary health care settings as 50% was aged less than 25 y [13].
This study result shows that majority of the people screened had illness affecting the respiratory system, symptoms and signs, musculo-skeletal system and digestive system in the order of the proportion affected. More male patients were affeced with respiratory, digestive illnesses and with signs and symptoms category when compared to women, while more women were affected with musculo-skeletal problems when compared to males. 19% of the people were found to be suffering from non-specific illnessess which were not been classified under any other system. An earlier study conducted in rural Karnataka showed that the level of morbidity is very high with fever of unknown origin, respiratory including ENT ailments and bronchial asthma, disorder of joints and bones, diarrhoea/dysentery and gastritis /gastric ulcer [1].
A study in Kerala showed that the major diseases prevalent were: diseases of bones and joints, hypertension, viral fever, diabetes, common cold, asthma, diseases of the nerve system, cardiovascular diseases, cough and acute bronchitis. These diseases account for about 75% of the total illness in the population [7]. A study in Ahmedabad city showed mainly 3 type of morbidity in the study population. They were musculoskeletal disorders, respiratory disorders and digestive disorders. Their contribution was more than 50 % of the reported morbidity [14].
The overall burden of diseases in Soweto showed that respiratory problems were significant in all age groups. Upper respiratory tract infections constituted 16% of the diagnoses. Digestive complaints were second most common reason and complaints of the musculo- skeletal system were frequent in older patients [12]. Morbidity and Mortality Report for the District Swat, Pakistan showed that upper respiratory tract infection was the most common cause of consultation. Acute diarrhea, lower respiratory tract infection, scabies, unexplained fever and bloody diarrhoea accounted for rest of the consultations [15].
The morbidity pattern study in Karachi, Pakistan using the ICD-10 coding for identifying the morbidity patterns presenting at the primary health centers showed that the most common diseases presented belonged to the respiratory system, disease of symptoms, signs and abnormal findings followed by infections or parasitic infestations, diseases of the reproductive system and disease of the musculoskeletal system and connective tissue [16]. The Tunisia study also found that respiratory diseases were the main problems managed in primary health care, followed by digestive, locomotive, cardiovascular affections and skin diseases. These five conditions alone constituted about 80% of the total cases [13]. In an Ahmedabad study the morbidity rate for both sexes was 30.8%. Anaemia was found in 19% of females of age group of 15-44 y. Respiratory tract infections and diarrhoea were present in 7.4% and 3.7% of studied population respectively. The incidence rates for respiratory tract infections and diarrhoea were found higher among 0-4 y age group children [17].
In a Chennai study, respiratory illness was present in 17.2% of the study population and 13.5% had other infections. Anaemia was significantly higher among females of all age groups. The prevalence of hypertension among the adults was 21.4%, and glucose intolerance was 8.6%. Hypertension and diabetes are considered lifestyle-related disorders but, they seem to be prevalent even among the poor. Eye disorders like defective vision, cataract, and uncorrected myopia together were present in 22.5% of the surveyed population [18]. In this study only about 10% of the patients reported with non-communicable diseases. An earlier study in the present study area showed that the burden of chronic diseases was high among the elderly while communicable diseases burden was found to be low [10].
The present study clearly shows that nearly 67% of the patients reported with problems affecting the four major systems; respiratory illnesses, complaints with ‘symptoms & signs’, musculo-skeletal and digestive diseases. While skin, eye, infection and parasitic diseases affected about 14.7% of the patients. Only 3.7% of the patients came with problems related to endocrine and nutrition, circulatory system, diseases of blood and nervous system. Respiratory illness affected nearly 60.7% of the under five children and its incidence tapers off as age advances to affecting only 9.2% of the elderly. 21.6% of the adults reported with ‘signs and symptoms’ while 13.9% underfives and 18% of the elderly reporting with non-specific complaints. Illness related to musculo-skeletal system affected mostly the elderly (38.6%) followed by the adult population (26.8%). More than double the number of females were affected with musculoskeletal problems when compared to males. Digestive system illness affected 17.3% of the school age children while 8.4% of the underfives were affected with skin problems. Eye problems affected the elderly most(13.2%) while Infection & parasitic diseases affected the children most (12.4%). The outcome of this reported mobidity profile shows that there are close similarities as well as variations when compared to the results of most of the studies conducted elsewhere within and outside India.
Future measures to be taken based on the study outcome
This study helps to explore the possibilities of identifying the advantages of the standard disease coding system in the primary care settings. The results enabled us to identify the main health problems which needs to be managed by the primary health care providers in the district of Kancheepuram. However, these results were mainly representative of morbidity pattern of the people who reported to the weekly screening camps conducted irrespective of the parallely existing health care providers in the area. Patients with acute and/or chronic or life threatening illnesses reported were conspicuously less.
Therefore, more well planned region wise morbidity profiling of population using ‘family folders’ maintained at the local health care facility is needed which will help to update and plan future strategies to combat the growing diseases burden in our country. Computerization is an important requirement for this program. This will also help to create a morbidity data base for the local administrative unit by combining the morbidity profile of various population groups in the region.
System and Sex wise distribution of morbidity profile
| S.no | System | Male | Female | Total |
|---|
| No | % | No | % | No | % |
|---|
| 1 | Respiratory | 1086 | 23.1 | 1379 | 18.1 | 2465 | 20.0 |
| 2 | Symptoms & Signs | 928 | 19.8 | 1406 | 18.5 | 2334 | 19.0 |
| 3 | Musculo- Skeletal | 443 | 9.4 | 1538 | 20.2 | 1981 | 16.1 |
| 4 | Digestive | 634 | 13.5 | 836 | 11.0 | 1470 | 11.9 |
| 5 | Skin | 356 | 7.6 | 422 | 5.5 | 778 | 6.3 |
| 6 | Eye | 220 | 4.7 | 366 | 4.8 | 586 | 4.8 |
| 7 | Infection & parasitic diseases | 181 | 3.9 | 261 | 3.4 | 442 | 3.6 |
| 8 | Genito Urinary | 17 | 0.4 | 249 | 3.3 | 266 | 2.2 |
| 9 | Endocrine & Nutrition | 63 | 1.3 | 146 | 1.9 | 209 | 1.7 |
| 10 | Ear | 94 | 2.0 | 101 | 1.3 | 195 | 1.6 |
| 11 | Circulatory | 57 | 1.2 | 74 | 1.0 | 131 | 1.1 |
| 12 | Diseases of Blood | 12 | 0.3 | 55 | 0.7 | 67 | 0.5 |
| 13 | Nervous system | 18 | 0.4 | 38 | 0.5 | 56 | 0.4 |
| 14 | Injury | 32 | 0.7 | 20 | 0.3 | 52 | 0.4 |
| 15 | Antenatal | 0 | 0.0 | 47 | 0.6 | 47 | 0.4 |
| 16 | Normal | 551 | 11.7 | 678 | 8.9 | 1229 | 10.0 |
| Total | 4694 | 38.1 | 7614 | 61.9 | 12308 | 100.0 |
System subgroup and sex wise distribution of morbidity profile
| System Subgroups | Male | Female | Total |
|---|
| No | % | No | % | No | % |
|---|
| 1 | Respiratory |
| URI | 940 | 86.6 | 1224 | 88.8 | 2164 | 87.8 |
| LRI | 108 | 9.9 | 123 | 8.9 | 231 | 9.4 |
| Asthma | 18 | 1.7 | 25 | 1.8 | 43 | 1.7 |
| COPD | 20 | 1.8 | 7 | 0.5 | 27 | 1.1 |
| 2 | Symptoms & Signs |
| Fever | 245 | 26.5 | 378 | 26.9 | 623 | 26.7 |
| Head ache | 218 | 23.5 | 370 | 26.3 | 588 | 25.2 |
| Abdominal pain | 156 | 16.8 | 223 | 15.9 | 379 | 16.2 |
| Giddiness | 154 | 16.6 | 223 | 15.9 | 377 | 16.2 |
| Chest pain | 155 | 16.7 | 212 | 15.1 | 367 | 15.7 |
| 3 | Musculo- Skeletal |
| Myalgia | 208 | 47.0 | 765 | 49.7 | 973 | 49.1 |
| Osteoarthritis | 161 | 36.3 | 449 | 29.2 | 610 | 30.8 |
| Low back ache | 51 | 11.5 | 237 | 15.4 | 288 | 14.6 |
| Spondylosis | 21 | 4.7 | 69 | 4.5 | 90 | 4.5 |
| Inter vertebral disc prolapse | 2 | 0.5 | 18 | 1.2 | 20 | 1.0 |
| 4 | Digestive |
| Dental caries | 466 | 73.5 | 443 | 53.0 | 909 | 61.8 |
| Acid peptic disease | 139 | 21.9 | 353 | 42.2 | 492 | 33.5 |
| Gingivitis | 29 | 4.6 | 40 | 4.8 | 69 | 4.7 |
| 5 | Skin |
| Skin infections | 187 | 52.5 | 156 | 37.0 | 343 | 44.1 |
| Excema / Dermatitis / Urticaria | 91 | 25.6 | 139 | 32.9 | 230 | 29.5 |
| Skin Appendages | 31 | 8.7 | 52 | 12.3 | 83 | 10.7 |
| Skin others | 47 | 13.2 | 75 | 17.8 | 122 | 15.7 |
| 6 | Infection & parasitic diseases |
| Worm infestations | 162 | 89.5 | 238 | 91.2 | 400 | 90.5 |
| GIT Infections | 12 | 6.6 | 18 | 6.9 | 30 | 6.8 |
| Scabies | 5 | 2.8 | 3 | 1.1 | 8 | 1.8 |
| Tuberculosis | 2 | 1.1 | 2 | 0.8 | 4 | 0.9 |
| 7 | Eye |
| Refractive errors | 139 | 63.2 | 238 | 65.0 | 377 | 64.3 |
| Cataract | 81 | 36.8 | 128 | 35.0 | 209 | 35.7 |
System and Age group wise distribution of common morbidities
Percentage of non communicable diseases burden among the study group
Conclusion
Studying the morbidity pattern in a defined geographical area should prove more useful to local health authorities and public health researchers about the exisitng disease burden in that area rather than the very broad patterns of country/state wide data. Knowing morbidity patterns at a small-area level will be useful for morbidity analysis and prevention program planning. To achieve the target of “Health for all in the 21st century” it is required to understand the patterns of morbidity by different strata, demographic, socioeconomic, and household environment characteristics in rural area which will inturn help the planners and policy makers while implimanting appropriate health programmes to reduce morbidity.
The National Health Programs are implemented in our country to reduce the morbidity and mortality due to specific diseases. Even though mortality rates have started coming down, the morbidity due to commonly occuring communicable diseases is very high with increasing burden of chronic / noncommunicable illness and emerging infectious diseases among the population. With this “triple burden of diseases”, it seems the target of achieving “Better Health for all in the 21st century” is still a long way to go.
[1]. RV Deshpande, Morbidity Differentials in Rural KarnatakaThe Journal of Family Welfare 1998 4:9-14. [Google Scholar]
[2]. AN Mukherjee, K Karmakar, Untreated Morbidity and Demand for Healthcare in India: an analysis of National Sample Survey DataEconomic & Political Weekly 2008 43(46):71-77. [Google Scholar]
[3]. S Ghosh, P Arokiasamy, Morbidity in India; Trends, Patterns and DifferentialsJournal of Health Studies 2009 2:136-4. [Google Scholar]
[4]. Report of the Working Group on Disease Burden for the 12th Five Year Plan WG3 (1): Communicable Diseases. Report (30-07-2011) Government of India Planningn Commission. http://planningcommission.nic.in/aboutus/committee/wrkgrp12/health/WG_3_1communicable.pdf Available from: [cited 2014 May10] [Google Scholar]
[5]. C Aparajita, AV Ramanakumar, Burden of Disease in Rural India: An Analysis Through Cause Of DeathThe Internet Journal of Third World Medicine 2005 2(2):43-48. [Google Scholar]
[6]. TR Dilip, Age-Specific Analysis of Reported Morbidity in Kerala, India. World Health & PopulationTetracyclineTeratology 2007 9(4):98-108.http://www.longwoods.com/content/19527 [cited 2013 May 14]. Available from: [Google Scholar]
[7]. K Navaneetham, M Kabir, CS Krishnakumar, Morbidity Patterns in Kerala: Levels and Determinants (April 1, 2009). CDS Working Paper No.411. [cited 2013 May 14]. Available at SSRN: http://ssrn.com/abstract=1629544 [Google Scholar]
[8]. He Gu, Morbidity Differentials among the Adult Population in Rural Kanchanaburi. DSS. A Thesis Submitted in Partial Fulfillment of the Requirements for the Degree of Master of Arts. Faculty Of Graduate Studies. Mahidol University 2004. [cited 2014 May 16]. Avaialble from: http://ipsr.healthrepository.org/bitstream/123456789/114/2/THCT2004_Gu%20He_eng.pdf [Google Scholar]
[9]. Census 2011; Tamil Nadu Provisional Population Totals March 2011. Director of Census Operations Tamil Nadu Ministry of Home Affairs [cited 2014 Iune 10]. Available from: http://www.tnebes.org/aroundus/pub/census2011_tn.pdf [Google Scholar]
[10]. K Ajitha, S Gopalakrishnan, P Ganeshkumar, AV Christopher, KJ Ranjit, M Suresh, Morbidity Pattern and Nutritional Status of Elderly Population in Rural Tamil NaduJournal of The Indian Academy of Geriatrics 2011 7:159-62. [Google Scholar]
[11]. ICD-10 Version 2010. http://apps.who.int/classifications/icd10/browse/2010/en#/XVIII [Google Scholar]
[12]. R Hoosain, The morbidity patterns of patients attending general practices in Soweto. WITS Universitie's Digital Materials 2009.[cited 2014 June11]. Available from: http://hdl.handle.net/10539/6343 [Google Scholar]
[13]. R Gataa, TN Ajmi, I Bougmiza, A Mtiraoui, Morbidity patterns in general practice settings of the province of Sousse, Tunisia. Pan African Medical Journal 2009;3:11. [cited 2014 June 21]. Available from: http://www.panafrican-medjournal.com/content/article/3/11/full [Google Scholar]
[14]. M Rajesh, P Niraj, P Reena, Morbidity profile of Brick Kiln workers around Ahmedabad city, GujaratHealthline 2010 1(1):41-44.[cited 2014 June 17]. Available from http://iapsmgc.org/oa7.pdf [Google Scholar]
[15]. Morbidity and Mortality Report. District Swat DoH NWFP, Pakistan. WEEK 49, 2009 World Health Organization Pakistan. Emergency Preparedness & Humanitarian Action (EHA) Islamabad – Pakistan [Google Scholar]
[16]. Q Anjum, E Alam, R Rizvi, J Usman, S Shaikh, Y Ahmed, Morbidity pattern and utilization of a primary health care centre in a low socioeconomic area of KarachiJ Pak Med Assoc 2006 56(1):13-16.[cied 2014 May 12]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16454128 [Google Scholar]
[17]. G Mihir, K Geeta, Socio-demographic and morbidity profile of slum area in Ahmedabad, IndiaNational Journal of Community Medicine 2010 1(2):106-10.[cited 2014 May12]. Available from: http://www.njcmindia.org/home/abstrct/53/ [Google Scholar]
[18]. V Viswanathan, S Tharkar, Can the divide be bridged: Overview of life in urban slums in IndiaIndian J Community Med [serial online] 2010 35:198-9.[cited 2014 May 13]. Available from: http://www.ijcm.org.in/text.asp?2010/35/1/198/62562 [Google Scholar]