Systematised Epidermal Nevus - A Case Report
Manoharan Dhanaraj1, Manoharan Ramalingam2
1Professor, Department of Dermatology,Sree Balaji Medical College & Hospital, Bharath University, Chennai, India.
2Consultant Dermatologisty, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Manoharan Dhanaraj, 11/2, Veeraperumal St, Triplicane, Chennai-600005, India.
E-mail: drmanomd@yahoo.co.in
A 20-year-old female presented with raised skin lesions all over the body since birth. Clinical examination revealed multiple pigmented macules and hyperkeratotic papules seen along Blaschko's lines over the face, neck, trunk and both lower limbs. Histopathological examination revealed hyperkeratosis with moderated acanthosis and uniform pigmentation over basal zone. Systemic examination was found to be normal. A diagnosis of systematised epidermal nevus in the absence of epidermal nevus syndrome was diagnosed and the patient was asked to undergo carbon dioxide laser mediated destruction of the skin lesions. The patient was also advised to be under surveillance for late onset neurological symptoms.
Epidermal naevus, Epidermolytic, Verrucous
Case Report
A 20-year-old female born to nonconsanguineous parents was seen in our outpatient department with complaints of raised skin lesions all over the body since birth. There was a history of darkening and thickening of the lesions with age. The growth and developmental history were normal and there was no history of seizures or learning difficulty, altered vision or difficulty in hearing.
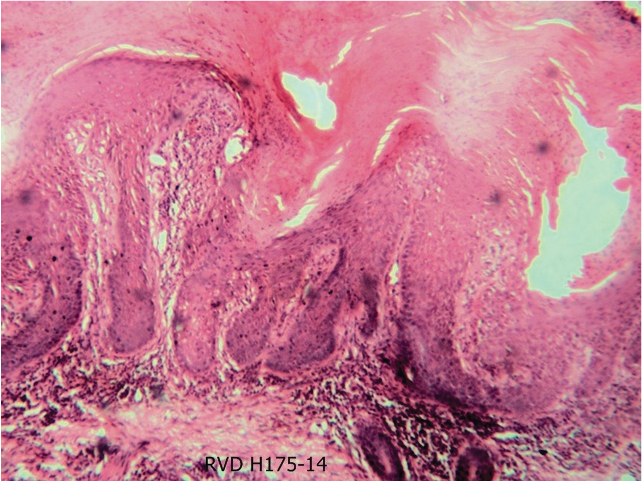
On examination there were multiple pigmented macules and hyperkeratotic papules arranged in streaks and whorls over the forehead, left side of face extending from the left lower eyelid upto mid face, as a linear streak from near the angle of mouth left side to the neck, as a linear streak over the temple and adjoining the upper eyelid and side of face on the right side. Similar lesions were seen as streaks on both sides of the neck [Table/Fig-1], as linear streaks extending from posterior aspect of neck to the upper back [Table/Fig-2], as whorls over sides of chest and abdomen and as linear streaks over both lower limbs. The oral and genital mucosa were found to be normal. Histopathology of the lesion taken from left leg revealed hyperkeratosis with moderate acanthosis [Table/Fig-3]. There was uniform pigmentation over the basal zone. In the dermis there were prominent hair follicles and sebaceous glands. The examination of other systems did not reveal any abnormality. There were no skeletal deformities. Examination of the nervous system was also observed to be normal. Magnetic resonance imaging (MRI)brain did not reveal any abnormality. IQ testing was done and the patient was found to be of normal intelligence.
With the above findings, we came to a conclusion of systematised epidermal naevus in the absence of epidermal naevus syndrome as described by Lever's classification. The patient was asked to undergo carbondioxide laser mediated destruction of the skin lesions and advised to follow up once every six months to check for neurological symptoms which may sometimes have a late onset.
Discussion
Epidermal naevi are rare hamartomas arising from the embryonic ectoderm. They are commonly seen as localized linear lesions occuring along the lines of Blashko. They are said to be systematized when they occur as more than one linear lesion as in Lever's classification of epidermal naevi. Around 30% of the epidermal naevi, especially the systematized ones are often associated with multisystem abnormalities especially of the central nervous system, eyes and skeleton. In such a case they are called epidermal nevus syndrome. In our case, it presented in a 20-year-old female patient without any evidence of systemic involvement. Epidermal naevi can be further subdivided into epidermolytic and nonepidermolytic. Nonepidermolytic verrucous epidermal naevi are considered to be heterogeneous and represent mosaicism for different yet unidentified mutations. Stosiek et al., identified chromosomal mosaicism in two male patients with non-epidermolytic verrucous epidermal naevi [1]. Our patient could be classified under the nonepidermolytic type. Non-epidermolytic verrucous epidermal naevi usually present at birth as like in our case. However, late onset lesions have also been reported [2]. At birth they have a whitish or macerated appearance and become slightly pink or as pigmented velvety streaks or plaques within a few days. Later with age, they darken and develop a warty surface. They may extend into the adjacent mucosal surface or nail fold. They may cause nail ridging, splitting, discolouration and dystrophy of the nail when involved. These lesions may be responsible for recurrent paronychia when they impinge on the nail fold. Over the flexures, these lesions may become macerated and foul smelling. Non-epidermolytic verrucous epidermal naevi have been associated with scalp (wooly hair naevi) [3]. Malignant degeneration has been reported to occur rarely within these lesions mostly over 40 y of age. A wide range of developmental abnormalities have been usually reported to occur in association with systematized non-epidermolytic epidermal naevi and include megalopinna, aplasia cutis of the scalp and syndromes such as epidermal naevus syndrome, Proteus syndrome, Klippel Trenaunay syndrome and McCune Albright syndrome [4]. In our case none of these associations were observed even though the lesions were observed to extend from head to foot, which could be considered a rare phenomenon. A similar case was reported by Loff et al., in which severe involvement of the eyelids led to trichiasis [5]. Only a few cases of nonepidermolytic systematized epidermal naevi without epidermal naevus syndrome have been reported in global literature and our case could be considered one amongst them.
Hyperkeratotic papules arranged in streaks on both sides of the neck

Linear streaks extending from posterior aspect of neck to the upper back

Histopathology of the lesion taken from left leg revealed hyperkeratosis with moderate acanthosis
Conclusion
Epidermal naevi can present in various forms and in association with a wide variety of disorders. Histopathology of these lesions is vital to differentiate epidermolytic forms from non epidermolytic lesions since each is known to have different associations. A thorough examination should be supplemented with observation for the entire lifetime as neurological manifestations may sometimes present late in adulthood.
[1]. N Stosiek, R Ulmer, P von drn Driesch, Chromosomal mosaicism in two patients with epidermal verrucous neviJ Am Acad Dermatol 1994 30:622-25. [Google Scholar]
[2]. BB Adams, DF Mutasim, Adult onset verrucous epidermal nevus J Am Acad Dermatol 1999 41:824-26. [Google Scholar]
[3]. S Wright, NR Lemoine, IM Leigh, Wooly hair nevi with systematized linear epidermal naevusClin Exp Dermatol 1986 11:179-82. [Google Scholar]
[4]. J Wikler, TM Starink, Acanthosis nigricans like epidermal naevus and Klippel Trenaunay syndromeBr J Dermatol 1990 123:539 [Google Scholar]
[5]. HJ Loff, DS Bardenstein, MR Levine, Systematized epidermal nevi: case report and review of clinical manifestationsOphthal Plast Reconstr Surg 1994 10(4):262-66. [Google Scholar]