Autoimmune Pancreatitis - A Case Report
Varuna Mallya1, KR Rathi2, Kavita Sahai3, CK Jakhmola4
1 Assistant Professor, Department of Pathology, Army College of Medical Sciences & Base Hospital, New Delhi, India.
2 Advisor, Department Pathology & Neuropathology, Army College of Medical Sciences & Base Hospital, New Delhi, India.
3 Professor & HOD, Department of Pathology, Army College of Medical Sciences & Base Hospital, New Delhi, India.
4 Senior Advisor, Department of G I Surgery, Army College of Medical Sciences & Base Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Varuna Mallya, Assistant Professor, Department of Pathology, Army College of Medical Sciences & Base Hospital, New Delhi, India. E-mail : varunamallya@gmail.com
Autoiommune pancreatitis (AIP) is a rare disease that has distinct histological, immunological, serological and radiological findings. It is characterised histologically by lymphoplasmacytic infiltrate, storiform fibrosis, obliterative phelibitis and presence of IgG4 positive plasma cells and lymphocytes. Elevated serum levels of IgG4 are also noted. It is usually misdiagnosed preoperatively as pancreatic cancer. It may involve extrapancreatic sites also and responds well to steroid therapy. Here, we share our experience of AIP in a 52-year-old male.
IgG4, Pancreatic adenocarcinoma, Pancreatitis
Case Report
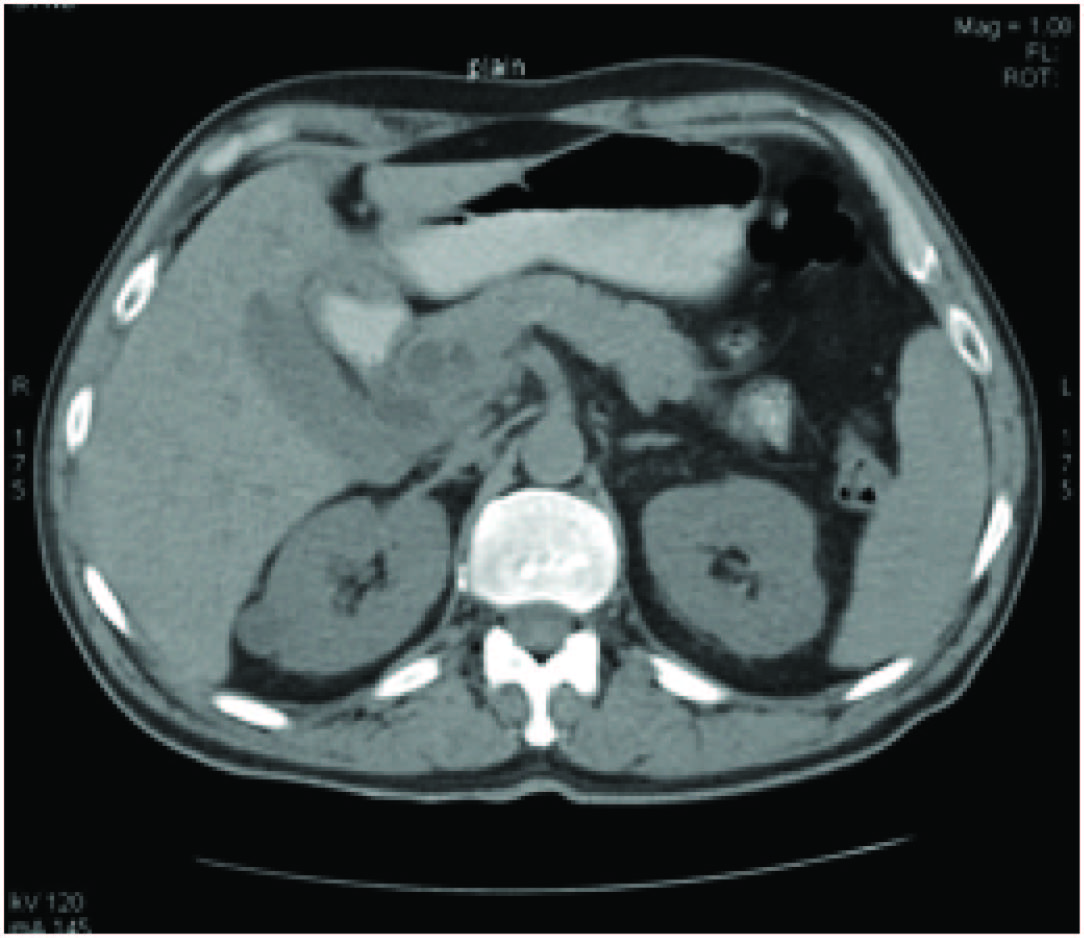
A 52-year-old non alcoholic male gave a history of diffuse abdominal pain since 1 year. His blood sugar and LFT's were all under normal limits. A CECT scan was done and a necrotic mass in the superior aspect of pancreatic head partially compressing the portal vein and common bile duct extending caudally with near circumferential encasement was noted. Pancreatic CBD at the midpancreatic level associated with hydrops gall bladder, dilated supraduodenal common bile duct was seen [Table/Fig-1] and a diagnosis of mitotic necrotic pancreatic lesion was given and the patient was taken for surgery and a Whipple's procedure was done.
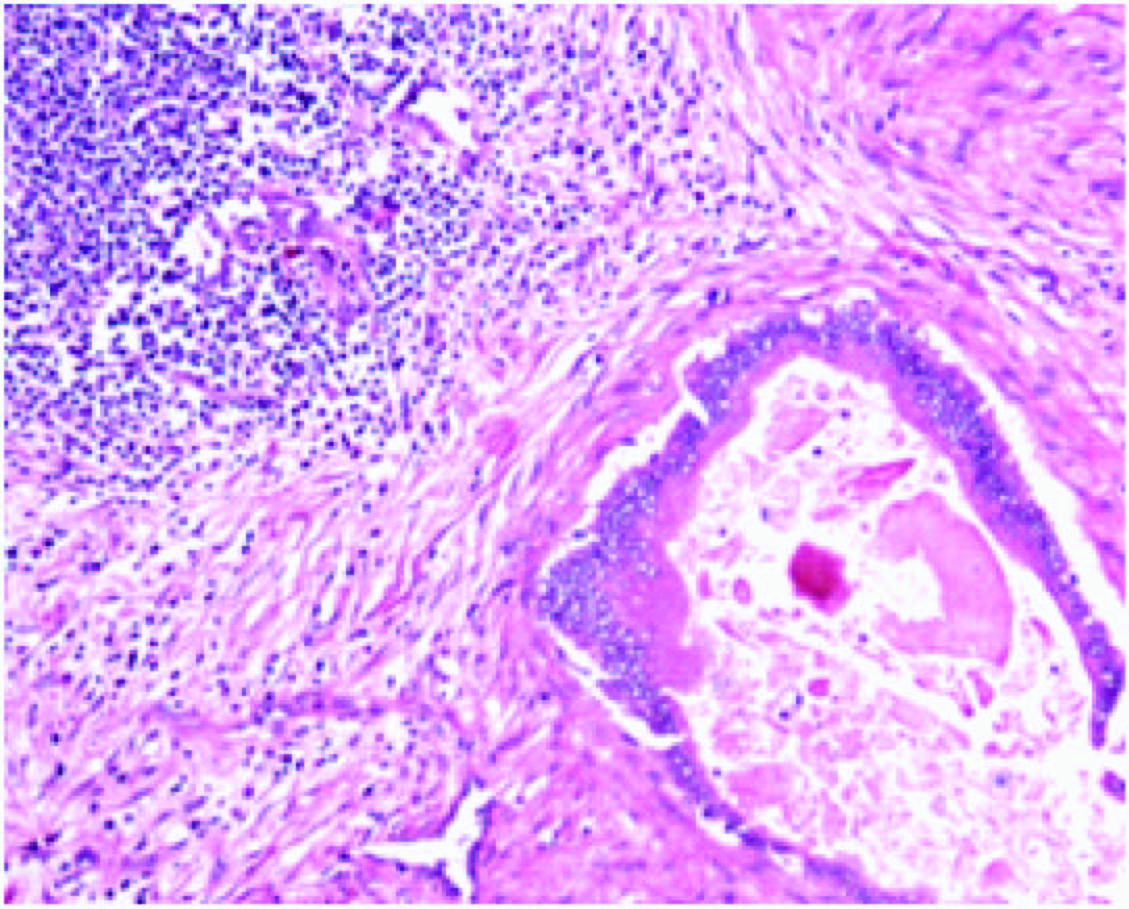
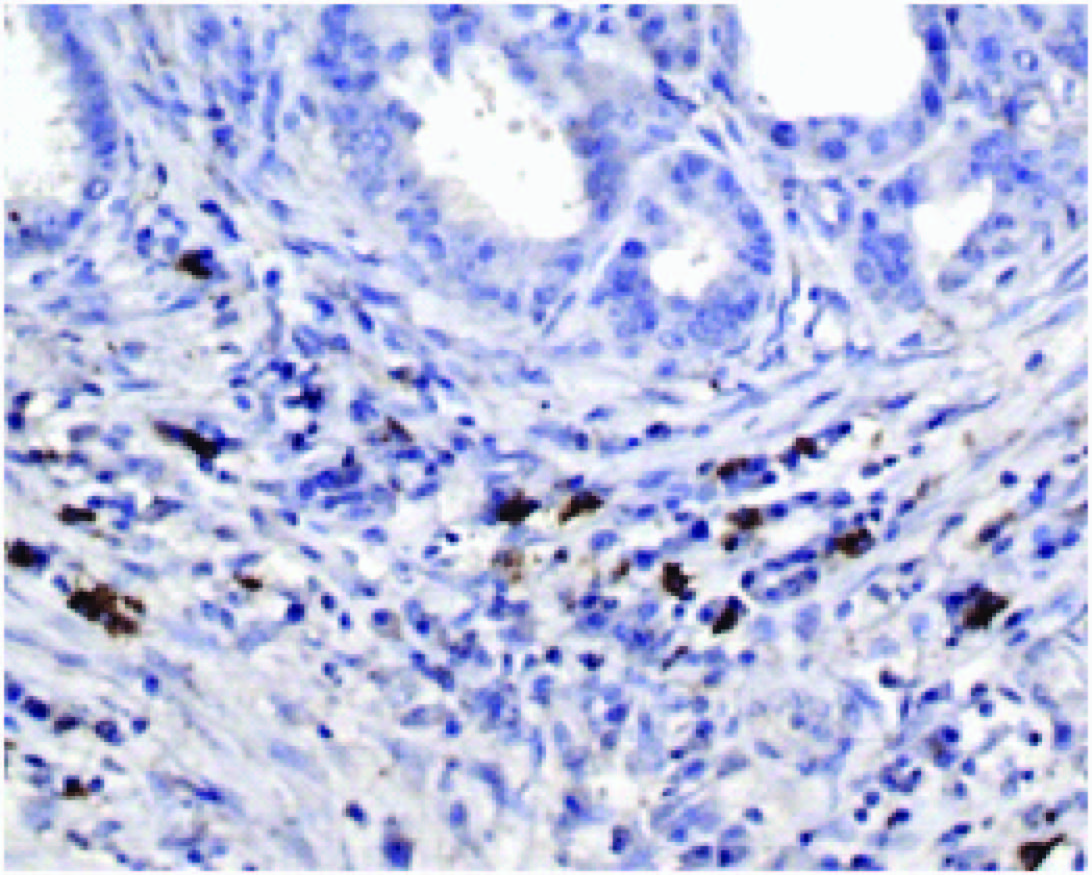
The specimen was received and histopathology slides were made. On H&E sections a dense lymphoplasmacytic infiltrate was seen in the pancreatic tissue. Obliterative phelibitis in the vessels was seen. There was dense storiform fibrosis seen in the stroma [Table/Fig-2]. Sections were taken for IHC. On IHC these cells were found to be IgG4 positive [Table/Fig-3]. Hence, based on the H&E and IHC sections a diagnosis of AIP was made.
IHC showing IgG4 positivity
Discussion
AIP is a very rare type of chronic pancreatitis that was first described in 1961 by Sarles et al., as primary inflammatory sclerosis of pancreas [1]. Various nomenclature were used to describe this disease. The term autoimmune pancreatitis (AIP) was coined by Yoshida et al., [2]. High serum IgG4 levels were noted in AIP patients [3] and this further led to the identification of infiltration of IgG4 positive cells in the pancreas and also extrapancreatic organs [4]. AIP is a very rare form of chronic pancreatitis and is described as a pancreatic manifestation of systemic fibroinflammatory disease. Seen predominantly in males over the age of 50 it is usually diagnosed in patients who undergo pancreatic resections for pancreatic cancers [5]. Various criteria were used to diagnose this entity with the Japanese Pancreatic Society criteria being described in 2006 [6]. Chari et al., proposed the Mayo Clinic ( HISORt) criteria in 2006 which took into account the histology, imaging, serology, other organ involvement and response to therapy to reach a diagnosis of AIP [7]. Asian Diagnostic Criteria was proposed in 2008 [8]. Also known as lymphoplasmacytic sclerosing pancreatitis, chronic sclerosing pancreatitis, non alchololic duct destructive pancreatitis, granulocytic epithelial lesion (GEL) positive pancreatitis AIP is a widely accepted terminology because the clinical, serological, histological and immunohistochemical findings point towards an autoimmune etiology. AIP could also show involvement of other organs such as the bile duct, liver, gall bladder, GIT, salivary glands, lacrimal glands, kidneys, retroperitoneum, lung, mesentry, breast, thyroid and the lymph node [9]. Histologically characterized by lymphoplasmacytic infiltrate, obliterative phlebitis, interstitial fibrosis and presence of IgG4 positive lymphocytes and plasma cells, it responds well to steroid therapy [10]. Hamans et al., reported high serum IgG4 levels in patients of AIP. Intense inflammation of IgG4 positive cells was also noted in pancreas and a plethora of other organs by Kamisawa [4]. This was a turning point as it led to the conlusion that AIP was a part of systemic diseases known as IgG4 associated disease (ISD) [4].
Seen mostly in males in the fourth and fifth decade, with abdominal pain, weight loss and jaundice being the clinical symptoms they mimic pancreatic cancers radiologically [9] and are diagnosed in patients on postoperatively on biopsy who have undergone pancreatoduodenectomy for suspected pancreatic cancers [5]. Our case was a 52-year-old male whose chief-complaint was a vague abdominal pain since one year. On CT scan a diagnosis of pancreatic cancer was made and he was taken up for resection. On H&E there was a dense lymphoplasmacytic infiltrate, obliterative phlebitis and storiform fibrosis. His H&E findings were classical of those seen in AIP [9]. To reinforce our diagnosis IgG4 staining was done and IgG4 positive lymphocytes and plasma cells were seen. A serum IgG4 could not be done as a preoperative differential of AIP was not considered. HISORt criteria was applied [7]. Since our case showed lymphoplasmacytic sclerosing pancreatitis (LPSP) with more than 10 IgG4 positive cell / hpf the group A histology criteria of HISORt was fulfilled and a diagnosis of AIP was made. Hence AIP is a form of chronic pancreatitis seen in males above the age of 50. It is a diagnostic challenge and it mimics pancreatic cancer. It forms a part of IgG4 related systemic diseases [4].
Conclusion
Our aim was to make the pathologist, radiologist and the surgeon aware of this rare entity as it shows a dramatic response to steroid therapy and saves the patient from the unnecessary morbidity and mortality of pancreatic resections.
[1]. Sarles H, Sarles JC, Muratore R, Guien C, Chronic inflammatory sclerosis of the pancreasan autonomous pancreatic disease?Am J Dig Dis 1961 6:688-98. [Google Scholar]
[2]. Yoshida K, Toki F, Takeuchi T, Watanabe S, Shiratori K, Hayashi N, Chronic pancreatitis caused by an autoimmune abnormality. Proposal of the concept of autoimmune pancreatitisDig Dis Sci 1995 40:1561-68. [Google Scholar]
[3]. Hamano H, Kawa S, Horiuchi A, Unno H, Furuya N, Akamatsu T, High serum IgG4 concentrations in patients with sclerosing pancreatitisN. Engl. J. Med 2001 344(10):732-38. [Google Scholar]
[4]. Kamisawa T, IgG4-related sclerosing diseaseIntern. Med 2006 45(3):125-126. [Google Scholar]
[5]. Hardacre JM, Iacobuzio-Donahue CA, Sohn TA, Abraham SC, Yeo CJ, Lillemoe KD, Results of pancreati-coduodenectomy for lymphoplasmacytic sclerosing pancreatitisAnn Surg 2003 237:853-58. [Google Scholar]
[6]. Okazaki K, Kawa S, Kamisawa T, Naruse S, Tanaka S, Nishimori I, Clinical diagnostic criteria of autoimmune pancreatitis: revised proposalJ. Gastroenterol 2006 41(7):626-31. [Google Scholar]
[7]. Chari ST, Smyrk TC, Levy MJ, Topazian MD, Takahashi N, Zhang L, Diagnosis of autoimmune pancreatitis: the Mayo Clinic experienceClin Gastroenterol Hepatol 2006 4(8):1010-16. [Google Scholar]
[8]. Otsuki M, Chung JB, Okazaki K, Kim MH, Kamisawa T, Kawa S, Asian diagnostic criteria for autoimmune pancreatitis: consensus of the Japan-Korea Symposium on Autoimmune PancreatitisJ. Gastroenterol 2008 43(6):403-08. [Google Scholar]
[9]. Zhang L, Smyrk TC, Autoimmune pancreatitis and IgG4-related systemic diseasesInt J Clin Exp Pathol 2010 3(5):491-504. [Google Scholar]
[10]. Zamboni G, Luttges J, Capelli P, Frulloni L, Cavallini G, Pederzoli P, Histopathological features of diagnostic and clinical relevance in autoimmune pancreatitis: a study on 53 resection specimens and 9 biopsy specimensVirchows Arch 2004 445:552-63. [Google Scholar]