Combined Gastric and Duodenal Perforation Through Blunt Abdominal Trauma
Bimaljot Singh1, Adarshpal Kaur2, Archan Lal Singla3, Ashwani Kumar4, Manish Yadav5
1 Junior Resident, Department of Surgery, Government Medical College and Rajindra Hospital, Patiala , Punjab, India.
2 Senior Resident, Department of Surgery, Government Medical College and Rajindra Hospital, Patiala , Punjab, India.
3 Assistant Professor, Department of Surgery, Government Medical College and Rajindra Hospital, Patiala , Punjab, India.
4 Professor, Department of Surgery, Government Medical College and Rajindra Hospital, Patiala , Punjab, India.
5 Junior Resident, Department of Surgery, Government Medical College and Rajindra Hospital, Patiala , Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Bimaljot Singh, H. No. 228/2, Chahal Street , Near Twakli Mour, Patiala, Punjab-147001, India.
E-mail: drbimal.undefined@gmail.com
Blunt abdominal traumas are uncommonly encountered despite their high prevalence, and injuries to the organ like duodenum are relatively uncommon (occurring in only 3%-5% of abdominal injuries) because of its retroperitoneal location. Duodenal injury combined with gastric perforation from a single abdominal trauma impact is rarely heard. The aim of this case report is to present a rare case of blunt abdominal trauma with combined gastric and duodenal injuries.
Blunt abdominal trauma, Feeding jejunostomy, Gastrojejunostomy, Tube duodenostomy
Case Report
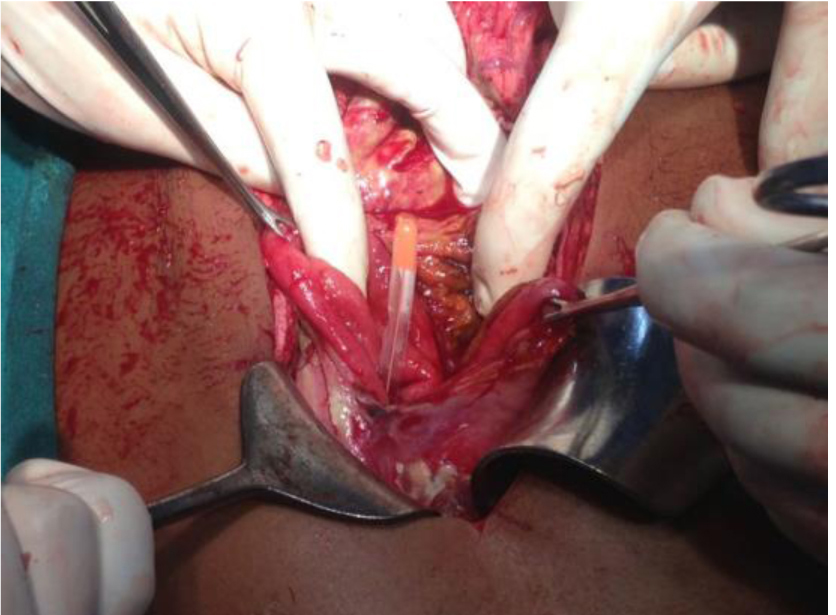
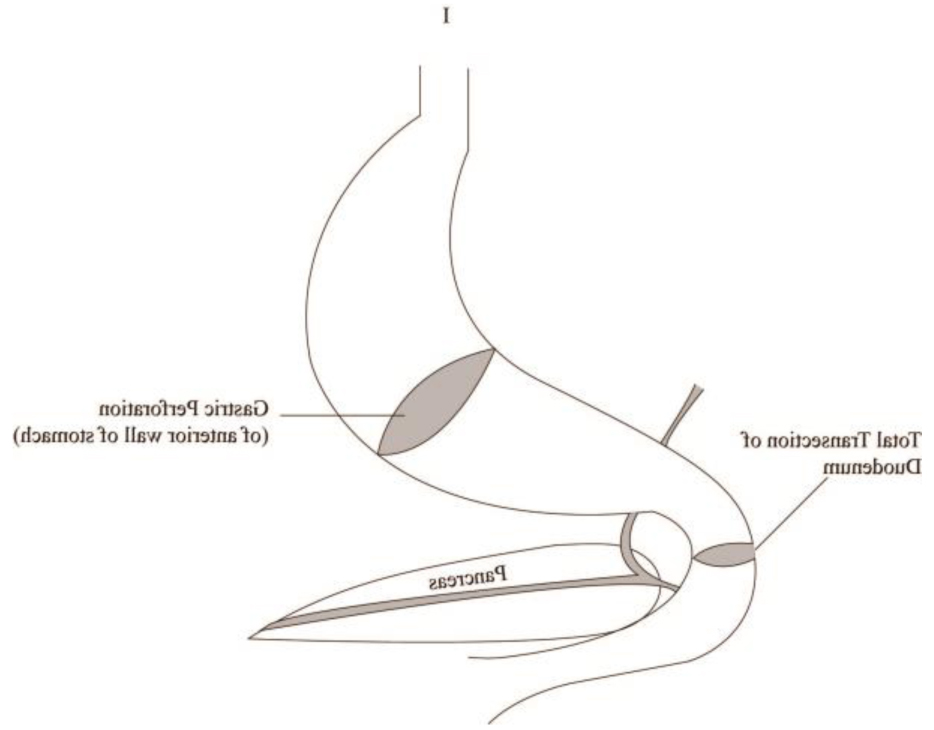
An 18-year-old man was brought to emergency surgery ward with a history of trauma two days back from a handcart taking bricks in a brickkiln factory. The patient was diagnosed as having a perforation, detected at some local hospital, from air under diaphragm. The patient could not be operated there because he was in shock for two days, for which he was resuscitated and an abdominal drain was put in right flank under local anesthesia. The patient presented to us in a dehydrated condition, conscious, with signs of peritonitis. Exploratory laparotomy was planned and the patient was immediately shifted to Operation Theater. A midline laparotomy was carried out. On opening the peritoneal cavity, Ryle’s tube was seen coming out and a big gastric perforation was identified [Table/Fig-1]. On exploration, two perforations were suspected, which were made clear after kocherization of duodenum was performed. There was a big perforation of anterior wall of stomach extending from lesser curvature to greater curvature and another in the second part of duodenum—total transaction, just proximal to ampulla of Vater opening [Table/Fig-2].
Ryle’s tube seen out of perforated stomach
Showing sites of perforations
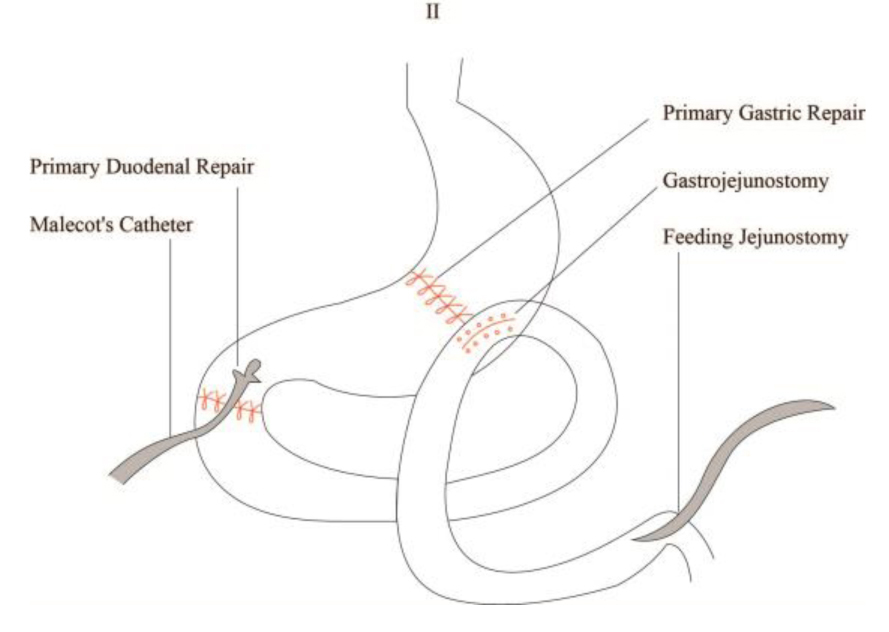
Primary repair of duodenal transaction over Malecot catheter (tube duodenostomy) was carried out. Laceration over anterior wall of stomach was repaired with gastrojejunostomy. Feeding jejunostomy was also performed [Table/Fig-3]. Two drains were kept, one in the Morrison’s pouch and another in the pelvic cavity. Postoperatively, the patient was kept in the intensive care unit for four days after which he was managed in ward. The patient did well and feeding Jejunostomy was started slowly over a period of time along with reinstallation of bile coming out of Malecot catheter drain mixed with milk through feeding jejunostomy. Contrast study was performed by injecting a radiopaque dye through Malecot catheter on 14th postoperative day, which showed no leakage from anywhere [Table/Fig-4]. Contrast-enhanced CT was also carried out for conformation, which again showed no leakage. Clear water was started orally and Malecot catheter was clamped. Then other liquids and semi solids were started, which patient tolerated well without any abdominal distension. During this period drain in the Morrison’s pouch showed minimal serous discharge, which was non-bilious, confirming no leakage from anywhere. Malecot’s catheter was removed on the 28th postoperative day, which did not increase any further discharge from Morrison’s drain [Table/Fig-5]. Morrison’s drain and feeding jejunostomy were removed on the 30th postoperative day.
Showing no leakage after injecting Radioopaque contrast through Malecot ’s catheter

Showing Malecot’s catheter, Morrison’s drain, and feeding jejunostomy in situ

Discussion
Isolated duodenal rupture following blunt abdominal trauma is rare. It is seen in approximately 2%–20% of patients with blunt abdominal injury and often results in after blows to the upper abdomen, or abdominal compression due to the common mechanism of high-riding seat belts [1–5].The management of duodenal injuries is still controversial, and there is a lack of consensus on the optimal treatment. In approximately 70%-85% cases, all duodenal injuries can be treated safely by primary repair. Duodenal injuries can be serious when the total amount of fluid passing through the duodenum exceeds 6 L per day [5]. Serious fluid and electrolyte imbalance can also be caused by a fistula present in this region. Complications may become life-threatening if a large amount of activated enzymes gets liberated into retroperitoneal space and peritoneal cavity [5].
If the disruption is less than 50% of the circumference, with regular injury border, adequate blood supply and without serious peritoneum pollution, the duodenum injury could be closed transversely and jejunostomy can be opted for decompression of duodenum. In 75%-85% of cases, duodenum injury could be closed primarily, and chances of duodenal fistula are less than 10% [6].
However, if the disruption is more than 50% of the circumference or there is a possibility that primary closure of the defect may narrow the lumen of the bowel or result in undue tension and subsequent breakdown of the suture lines, we may advise segmental resection and primary end-to-end duodenoduodenostomy, especially in case of injury of the first, second, or third part of the duodenum [7]. Suture of two ends without causing undue tension on the suture line is impossible if a large part of duodenum is lost. Surgeries of duodenal diverticulization, which include closure of the duodenal injury, gastric antrectomy with end-to-side gastrojejunostomy, tube duodenostomy, and generous drainage in the region of the duodenal repair, should be performed if a large tissue of the first part of duodenum is lost [8]. As duodenal diverticulization is a time-consuming process, it is not recommended in hemodynamically unstable patients or when there are several accompanied injuries. Closure of distal duodenum and Roux-en-Y duodenojejunostomy is an appropriate choice if the injury is distal to the ampulla of Vater. If the second part of the duodenum is injured, a direct anastomosis of Roux-en-Y over the injury in an end-to-side manner is appropriate because of the limited mobilization of this part. In case primary anastomosis is not possible, this procedure can be also applied to other parts [9].
There are also other concomitant surgically important intra-abdominal injuries in 40% of patients with duodenal injury and these are hepatic (38%) or pancreatic (28%) injuries [10]. But combined gastric and duodenal perforation is rare and its documentation in literature is not available. A preoperative diagnosis of the perforations present is difficult to make, and surgeon is always in dilemma of choosing between several preoperative investigations and surgical procedures.
Theoretically, duodenal perforation is associated with a leak of amylase and other digestive enzymes and determination of serum amylase concentration may be helpful in diagnosis [5,11]. However, the tests lack sensitivity [12,13]. Although the specifics of the grading system are useful for research purposes, they are less important than several simple aspects of the duodenal injury [5]:
The anatomical relation to the ampulla of Vater.
The characteristics of injury (simple laceration versus destruction of duodenal wall).
The involved circumference of duodenum.
The injury associated to stomach, biliary tract, pancreas, and major vessels.
As in our case, duodenal injury was associated with stomach injury due to direct trauma to abdomen. The number of such injuries has increased because of frequent automobile accidents and violent events [14].
Abdominal plain films, ultrasonic test, and CT scan can also help in diagnosis. Free air under diaphragm, retroperitoneal air, obliteration of Psoas muscle shadow, and scoliosis of lumbar vertebrae can give clue to injury [15]. In case of absence of positive signs, air or water-soluble radio-opaque contrast can be injected through nasogastric tube and its leakage can be easily detected. Barium is not used as it is difficult to clear up during surgery and may lead to infection postoperatively. Although routine preoperative laboratory tests are not helpful in diagnosis but some authors find that serum amylase is an important marker. Serum amylase level is found to be raised in 50% cases of upper gastrointestinal or duodenal injury [16].
If there is a high degree of suspicion, exploratory laparotomy is the ultimate diagnostic test. The explorative procedures need to be careful, comprehensive, accurate, and quick. Blocksom and co-workers [17] reported that if systolic blood pressure is lower than 90 mm Hg before surgery, the mortality can reach 46%, and if a patient needs transfusion more than 1000 ml, his/her hospital stay will be apparently longer. So, we should pay attention to controlling bleeding, correcting shock, and preventing infection during early hours of treatment. At the same time, surgery should be planned, and depending on the injuries found, meticulous repair should be carried out by experts. In our case, gastric perforation was dealt with primary repair by gastrojejunostomy, with duodenal repair over Malecot catheter with feeding jejunostomy for nutritional supplementation as nutritional supplementation through a jejunostomy tube is beneficial [17].
Conclusion
Combined gastric and duodenal perforation is rare. Delay in diagnosis and planning surgery can prove fatal for the patient. Early detection, early diagnosis, and early treatment of injuries has shown good prognosis. The surgical repair (that is exploratory laparotomy) is a safe and effective therapy for suspected gastrointestinal perforation. Meticulous repair by experienced surgeon, either in case of isolated gastric or duodenal or in case of combined gastric and duodenal perforation, done timely can significantly affect the outcome.
[1]. Weigelt JA, Duodenal injuriesSurg Clin North Am 1990 70(3):529-39. [Google Scholar]
[2]. Asensio JA, Feliciano DV, Britt LD, Kerstein MD, Management of duodenal injuriesCurr Probl Surg 1993 30(11):1023-93. [Google Scholar]
[3]. Fraga GP, Biazotto G, Villaça MP, Andreollo NA, Mantovani M, Trauma de duodeno: análise de fatoresrelacionados à morbimortalidade. [Duodenal trauma: factors related to morbimortality]Rev Col Bras Cir 2008 35(2):94-102. [Google Scholar]
[4]. Yutan E, Waitches GM, Karmy-Jones R, Blunt duodenal rupture: complementary roles of sonography and CTAm J Roentgenol 2000 175:1600 [Google Scholar]
[5]. Degiannis E, Boffard K, Duodenal injuriesBr J Surg 2000 87:1473-79. [Google Scholar]
[6]. Asensio JA, Petrone P, Roldan G, Pak-art R, Salim A, Pancreatic and duodenal injuries. Complex and lethalScand J Surg 2002 91(1):81-86. [Google Scholar]
[7]. Timaran CH, Martinez O, Ospina JA, Prognostic factors and management of civilian penetrating duodenal traumaJ Trauma 1999 47(2):330-35. [Google Scholar]
[8]. Ginzburg E, Carrillo EH, Sosa JL, Hertz J, Nir I, Martin LC, Pyloric exclusion in the management of duodenal trauma: is concomitant gastrojejunostomy necessary?Am Surg 1997 63(11):964-66. [Google Scholar]
[9]. Chen G, Yang H, Management of duodenal traumaChinese J Traumatol 2011 14(1):61-64. [Google Scholar]
[10]. Jurkovich GI, Injury to the duodenum and pancreas. In: Feiciano DV, Moore EE, Mattox KL, editorsTrauma 1996 3rd edStamford, CTAppleton & Lange:573-694. [Google Scholar]
[11]. Champault A, Roudie J, Smadja C, Traumatic duodenal necrosis with peri-ampullary duodenal detachmentJ Pediatr Surg 2004 39:1136-37. [Google Scholar]
[12]. Fang JF, Chen RJ, Lin BC, Hsu YB, Kao JL, Kao YC, Retroperitoneal laparostomy: an effective treatment of extensive intractable retroperitoneal abscess after blunt abdominal traumaJ Trauma 1999 46:652-55. [Google Scholar]
[13]. Fang JF, Chen RJ, Lin BC, Surgical treatment and outcome after delayed diagnosis of blunt duodenal injuryEur J Surg 1999 165:133-39. [Google Scholar]
[14]. Ivatury RR, Duodenal injuries: small but lethal lesionsCirujano Gen 2003 25(1):59-65. [Google Scholar]
[15]. Jayaraman MV, Mayo-Smith WW, Movson JS, Dupuy DE, Wallach MT, CT of the duodenum: an overlooked segment gets its dueRadiographics 2001 21:S147-60. [Google Scholar]
[16]. Asensio JA, Demetriades D, Hanpeter DE, Gambaro E, Chahwan S, Management of pancreatic injuriesCurr Probl Surg 1999 36(5):325-419. [Google Scholar]
[17]. Blocksom JM, Tyburski JG, Sohn RL, Williams M, Harvey E, Steffes CP, Prognostic determinants in duodenal injuriesAm Surg 2004 70(3):248-55.discussion 255 [Google Scholar]