A Rare Case of Malignant Fibrous Histiocytoma/ Pleomorphic Undifferentiated Sarcoma of the Kidney
Gregory Pathrose1, Nirmal Thampi John2, Ramani Manojkumar3
1Senior Registrar, Department of Urology, Christian Medical College, Vellore, Tamil Nadu, India.
2Associate Professor, Department of Urology, Christian Medical College, Vellore, Tamil Nadu, India.
3Professor, Department of Pathology, Christian Medical College, Vellore, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Nirmal Thampi John, Associate Professor, Department of Urology, Unit 2, Christian Medical College, Vellore, Ida Scudder Road, Vellore-632004, Tamil Nadu, India.
E-mail: nirmaltj@gmail.com
Malignant Fibrous Histiocytoma (MFH) usually arises from the extremities with the retroperitoneum being the second most common site. We present the case report of a 58-year-old man presenting with fever and was detected to have a renal mass on evaluation. He underwent a radical nephrectomy with a preoperative diagnosis of renal cell carcinoma. But the final histopathological report was MFH. Primary renal MFH is extremely rare and is usually diagnosed on histopathology with the aid of immunohistochemistry.
CD 68, Kidney, Radical nephrectomy
Case Report
A 58-year-old gentleman presented with history of fever and left loin pain for three months. On physical examination, he was found to have a renal mass. On laboratory evaluation he was found to be anaemic (PCV 23.8) with thrombocytosis (7,25,000/mm3) and had an elevated ESR (77). His CT abdomen revealed an 11 x 13 cm heterogenously enhancing mass arising from the upper pole of left kidney [Table/Fig-1]. There was no involvement of the contiguous structures but superiorly, it was adherent to the spleen.
He underwent a radical nephrectomy and splenectomy as the tumour was adherent to the spleen. His post operative period was uneventful.
Histopathology
Gross: A well-circumscribed tumour was seen arising from the upper and interpole of the kidney. The cut surface was grayish white, homogenous with focal areas of yellowish and myxoid change.
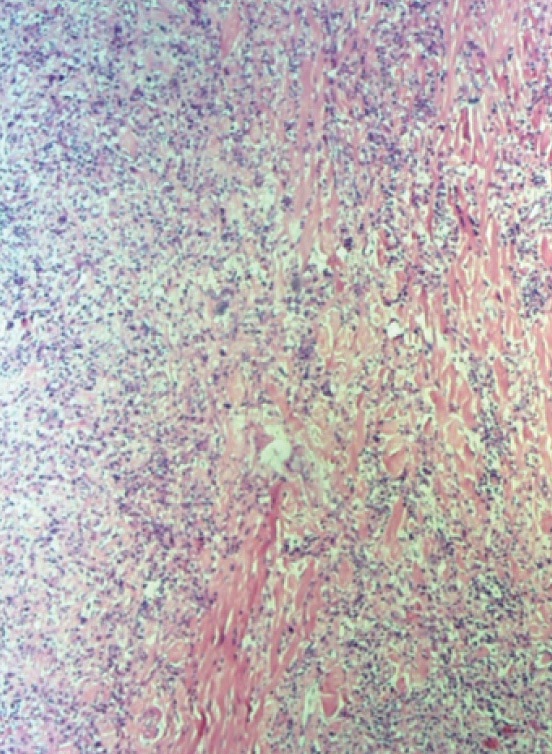
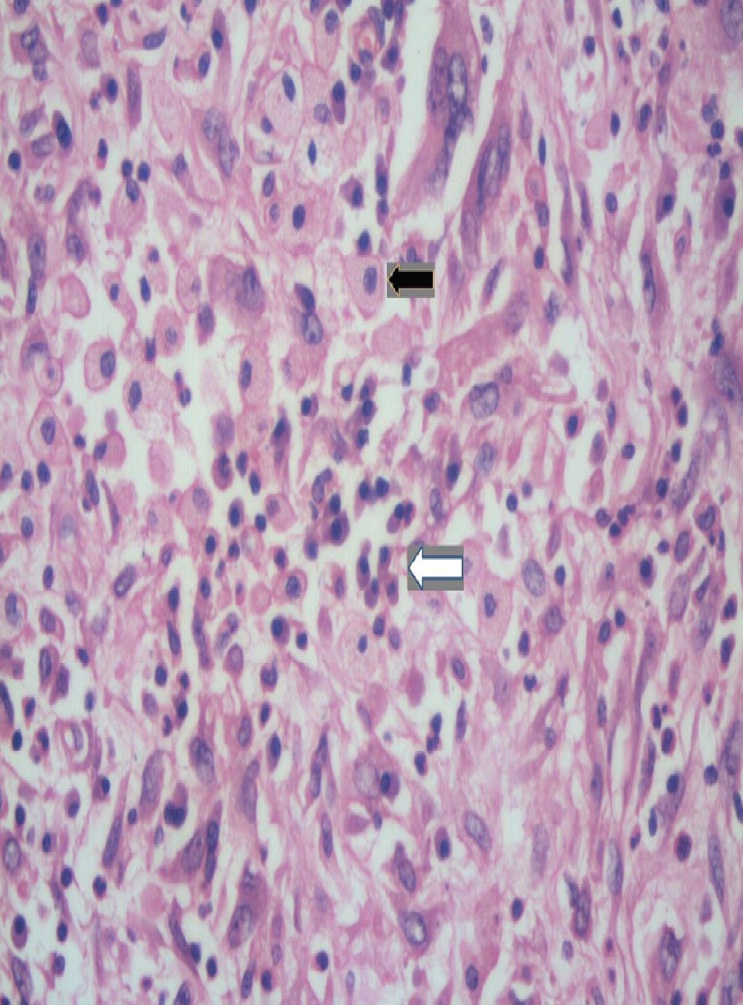
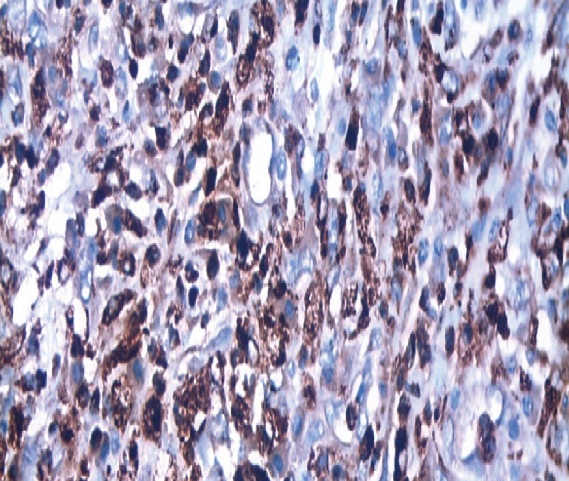
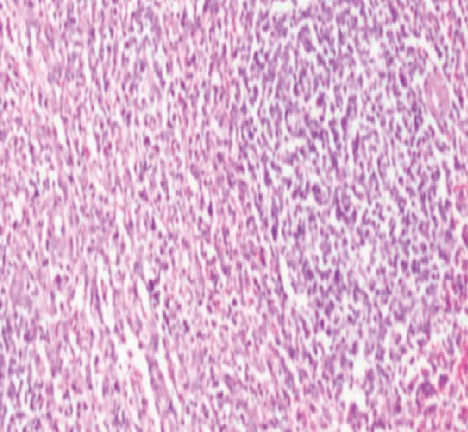
Microscopy: The renal parenchyma was infiltrated by a fairly circumscribed tumour [Table/Fig-2]; with clustered and scattered polygonal cells to spindle cells with markedly pleomorphic, vesicular nuclei and moderate amount of eosinophilic, cytoplasm. There were multinucleate giant cells, foamy macrophages and bizarre tumor cells. The intervening stroma showed many thick collagen bundle and dense infiltrates of lymphocytes, plasma cells, histiocytes, many neutrophils and eosinophils [Table/Fig-3]. There was focal hyalinization. There was no lymphovascular invasion or nodal involvement. The tumour cells were negative for desmin and myogenin but showed positive staining with CD68 [Table/Fig-4] on immunohistochemistry. These features were consistent with the diagnosis of inflammatory subtype of malignant fibrous histiocytoma. The tumour infiltrated the sinus fat with rest of the parenchyma being normal. Spleen showed features of congestive splenomegaly but was otherwise free of tumour [Table/Fig-5].
Discussion
MFH is a pleomorphic sarcoma arising from fibroblasts and histiocytes and was first described by O’brien and Stout in 1964 [1]. It is an extremely rare neoplasm and only 51 cases were reported till 2002 [2]. A few more cases have been reported since and have been highlighted [Table/Fig-6] .
MFH presents in the 6-7th decades of life usually, with nonspecific symptoms like fever, weight loss and non specific abdominal pain [2]. The most frequent site is the extremities (49%) followed by the retroperitoneum (16%) [2]. The male to female preponderance 28least common is the inflammatory subtype [13,14]. The histology of this patient has been reported as inflammatory type of MFH. It contains both fibrous and histiocytic elements. They stain positive for CD68 and anti α1 antichymotrysin but do not stain for cytokeratins [4].
According the latest WHO update on renal sarcoma, MFH has been replaced with the term pleomorphic undifferentiated sarcoma after other forms of differentiation has been ruled out [15]. MFH is an aggressive tumour necessitating radical surgery with recurrence rates as high as 44%. It is associated metastases to lung (82%) and lymph nodes (32%) [13,16]. The major predictors of outcome are size, depth of involvment and inflammatory component of tumour [13]. They also require adjuvant chemotherapy usually with Ifosfamide and doxorubicin owing to the high rates of local recurrence and metastasis. Anecdotal reports of response to adjuvant radiotherapy to the tumour bed are also reported in literature [17]. Despite aggressive treatment, local recurrence was seen in the first two years and mortality rate was 66% within the first year of radical nephrectomy [6].
CT scan showing a heterogeneously enhancing mass arising from the upper pole of left kidney

H&E 5x, showing renal parenchyma infiltrated by tumour cells
H&E 40x, showing clusters of pleomorphic spindle cells, interspersed with foamy histiocytes (black arrow) and mixed inflammatory cells (white arrow)
CD68 400x, Cells showing positivity on immunohistochemistry with CD68
H&E 40x, congested spleen
Case reports of MFH from 2001-2014
| Author | Year | Pathology | Outcomes |
|---|
| Kitajima K et al., [3] | 2003 | MFH | Post radical nephrectomy, no adjuvant therapy. Follow up till 30 months, patient asymptomatic. |
| Chen CH et al., [4] | 2003 | Giant cell subtype MFH | Radical nephrectomy followed by 6 cycles of local irradiation and subsequent chemotherapy with doxorubicin and ifosfamide. Patient followed up for 12 months without evidence of tumour recurrence. |
| Erolu M et al., [5] | 2005 | MFH | Radical nephrectomy with adjuvant RT with 6,600 rads. No recurrence at 15 months. |
| Singh SK et al.,[6] | 2006 | MFH | Patient died after 1 month of radical nephrectomy. |
| Ishibiki Y et al., [7] | 2007 | storiform-pleomorphic MFH arising from perirenal tissue | Refused adjuvant therapy after radical nephrectomy. Died due recurrence after 21 months. |
| Gupta R et al., [8] | 2008 | MFH | Patient dies after 2 cylces of chemotherapy |
| Ghosh A et al., [9] | 2008 | Inflammatory subtype of MFH | No follow up. |
| Mellas S et al., [10] | 2012 | Pleomorphic undifferentiated sarcoma | Post nephroureterectomy, refused adjuvant therapy. Died after 10 months. |
| Matsushita M et al [11] | 2013 | MFH arising from renal capsule | Post radical nephrectomy, symptom free till 14 month post operatively |
Conclusion
Malignant fibrous histiocytoma, now referred as undifferentiated pleomorphic sarcoma is a highly aggressive rare neoplasm with difficult preoperative diagnosis. Complete excision offers the only possible chance of cure with majority of patients succumbing to the illness in the first two years. Adjuvant therapy is of little or no benefit.
[1]. JE O’Brien, AP Stout, Malignant fibrous xanthomasCancer 1964 17:1445-56. [Google Scholar]
[2]. SJA Kim, BC Ahn, SR Kim, Primary malignant fibrous histiocytoma of the kidneyYosei Med J 2002 43(3):399-402. [Google Scholar]
[3]. K Kitajima, Y Kaji, M Morita, Y Okuda, K Sugimura, Malignant fibrous histiocytoma arising from the renal capsuleMagn Reson Med Sci 1970 2:99-202. [Google Scholar]
[4]. CH Chen, PS Lee, WJ Han, KH Shen, Primary giant cell malignant fibrous histiocytoma of the kidney with staghorn calculiJ Postgrad Med 2003 49(3):246-48. [Google Scholar]
[5]. M Erolu, H Bakirta, E Cimentepe, A Unsal, Malignant fibrous histiocytoma arising from the renal capsuleUrol Int 2005 75(4):368-70. [Google Scholar]
[6]. SK Singh, AK Mandal, MM Agarwal, A Das, Primary renal inflammatory malignant fibrous histiocytoma: A diagnostic challengeInt J Urol 2006 13:1000-02. [Google Scholar]
[7]. Y Ishibiki, T Matsumura, M Kawarai, Y Hukushi, Malignant fibrous histiocytoma arising from perirenal tissue: a case report Nihon Hinyokika Gakkai Zasshi 2007 98(4):638-42. [Google Scholar]
[8]. R Gupta, S Gupta, D Aggarwal, S Singh, Primary pleomorphic undifferentiated sarcoma of the kidney: A rare renal tomorIndian J Pathol Microbiol 2008 51(4):573-76. [Google Scholar]
[9]. A Ghosh, US Dwivedi, A Kumar, Inflammatory malignant fibrous histiocytoma of kidney: a case reportPathol R Pract 2008 204(11):857-61. [Google Scholar]
[10]. S Mellas, AA Bouchikhi, MF Tazi, A Khallouk, JE Elammari, MJ El Fassi, Primary Pleomorphic Undifferentiated Sarcoma—a Rare Renal Localization: A Case ReportCase Rep Urol 2012 2012:862493 [Google Scholar]
[11]. M Matsushita, T Okada, N Kawamura, T Ujike, M Nin, M Tsujihata, A case report of malignant fibrous histiocytoma arising from the renal capsuleHinyokika Kiyo 2013 59(11):733-36. [Google Scholar]
[12]. M Tarján, G Cserni, Z Szabó, Malignant fibrous histiocytoma of the kidneyScand J Urol Nephrol 2001 35:518-20. [Google Scholar]
[13]. SW Weiss, FM Enzinger, Myxoid variant of histiocytomaCancer 1977 39(4):1672-85. [Google Scholar]
[14]. J Rosai, Soft tissues. In: Ackerman’s Surgical Pathology 1996 8th EditionMosby, St Louis:2021-138. [Google Scholar]
[15]. CD Fletcher, The evolving classification of soft tissue tumors: An update based on the new WHO classificationHistopathology 2006 48:3-12. [Google Scholar]
[16]. TJ Joseph, DI Becker, AF Turton, Renal malignant fibrous histiocytomaUrology 1991 37:483-89. [Google Scholar]
[17]. R Marchese, P Bufo, G Carrieri, G Bove, Malignant fibrous histiocytoma of the kidney treated with nephrectomy and adjuvant radiotherapy: a case reportCase Rep Med 2010 2010 [Google Scholar]