Unusual Ventriculoperitoneal (VP) Shunt Tube Extrusion through Anus in a Child with Dandy Walker Malformation: A Rare Case Report
Hanish Bansal1, Gulzar Gupta2, Mayank Gupta3, Rakesh Kaushal4
1Assistant Professor, Department of Neurosurgery, Dmc & H, Ludhiana, Punjab, India.
2Assistant Professor, Department of Neurosurgery, Dmc & H, Ludhiana, Punjab, India.
3Resident, Department of Surgery, Dmc & H, Ludhiana, Punjab, India.
4Professor & Head, Department of Neurosurgery, Dmc & H, Ludhiana, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr Hanish Bansal, 10 B Udham Singh Nagar, Civil Lines, Ludhiana, Punjab-141001, India.
E-mail: y2khanish@rediffmail.com
Aim of this paper is to report a case of extrusion of Ventriculo peritoneal shunt tube through anus in a one year female child ( k/c/o dandy walker malformation ) treated with placement of ventriculo peritoneal shunt for post operative hydrocephalus after excision of Subtorcular occipital meningocoel. The exact cause of such extrusion is not known. Unusual migration of distal catheter tip of VP shunt is a rare and bowel perforation is reported to occur between 0.1% and 0.7%. The possible factors responsible for this complication are thin bowel wall in children, sharp and stiff end of the VP shunt, use of trocar by some surgeons, chronic irritation by the shunt, previous surgery, infection and silicone allergy. In view of the potential for meningitis prompt and aggressive management is essential to avoid morbidity and mortality.
Extrusion through anus, Hydrocephalus, Meningocoel, Ventriculoperitoneal shunt
Case Report
We report a case of a one year female who presented to us with extrusion of ventriculoperitoneal (VP) shunt catheter through anus. The child was brought to us with complaint of swelling over nape of the neck at 12 days of life when she was diagnosed as a case of Dandy walker malformation with large subtorcular occipital meningocoel [Table/Fig-1] for which she went underwent excision. The child later developed hydrocephalus at six months of age for which a ventriculo peritoneal shunt was done and the child was discharged in a satisfactory condition.
Six months later the child was brought back to us with complaint of shunt tube protruding through anus and was draining clear cerebrospinal fluid [Table/Fig-2]. On admission, she was conscious, active, and neurologically normal, with depressed anterior fontanalle and without signs of meningitis. Her abdomen was soft without any abnormality.
The child was taken to operation theatre and the distal end of the catheter was pulled out through the rectum after division of the shunt just below the reservoir ( this was done to avoid catheter track contamination ) and the ventricular end was send for culture and sensitivity. This was followed by intravenous antibiotics in anti shuntmeningitic doses. The child was observed carefully and an external ventricular drain was put once the anterior fontanalle started bulging on second postoperative day despite anti oedema medication. The plan was to reinsert new VP shunt once the culture reports were obtained. The ventricular end was sterile on culture. But the child was discharged against medical advice and was lost to follow up.
Discussion
VP shunt is an established method of diverting CSF for the management of hydrocephalus [1]. The peritoneal end of the VP shunt has been associated with complications such as mechanical blockade by omentum leading to shunt failure, pseudocyst formation, intestinal volvulus, inguinal hernia, perforations of hollow viscus, penetration into solid organs & abdominal wall and protrusion outside body [2].
Shunt migration into stomach, bowel, liver, chest, jugular vein, anus, vagina, and scrotum has been reported previously. Migration of the lower end of the shunt catheter occurs without any recognizable cause. Distal shunt migration has been reported in as many 10% of these cases [3]. Three cases of vaginal perforation have been reported in literature. First case of vaginal perforation by a VP shunt catheter was described by DC Patel in 1973 [4].
Abdominal complications account for about 25% of the complications caused by ventriculoperitoneal shunt insertion. Bowel perforation occurs between 0.1% and 0.7% of the times which may lead to significant morbidity and mortality due to peritonitis and/ or meningoventriculitis [5]. Thin bowel wall in children, sharp and stiff end of the VP shunt, use of trocar by some surgeons, chronic irritation by the shunt, previous surgery, infection and silicone allergy are some of the factors responsible for bowel perforation by ventriculoperitoneal shunt.
Catheter-induced gut perforations have been reported previously in the literature (at least 119 cases), with most common site being colon (70%), followed by the stomach (16%), and small bowel (14%). Factors like poor host immunity, bioreactivity of shunt components and superficial peritoneal shunt catheter placement may also contribute to shunt extrusion [6].
There is not an obvious relationship between the distal end length of the shunt and perforation rates. Vuyyuru et al., reported that malnutrition and a former abdominal surgery may increase the risk of migration due to adhesions arisen from infection [7].
Most patients with abdominal complications are asymptomatic. Fibrous tract formed at the perforated site usually seals the perforation, preventing spillage of faecal matter into the peritoneum, preventing peritonitis and delaying the correct diagnosis until a later stage at which ventriculitis or central nervous system infection has been fully established. In patients with the transanal protrusion of a VP shunt catheter, the diagnosis is obvious. The period between shunt placing and the protrusion of the catheter from the anus ranges from 2 to 20 months [8].
Management involves prompt removal of shunt, intravenous antibiotics, an adequate recovery gap so that cerebrospinal fluid culture is sterile and then followed by shunt replacement on opposite side. During the interval which is 3-4 week, the patient can be kept on cerebral dehydrants to limit the increasing hydrocephalus. In a patient with simple bowel perforation and no other complications, a formal laparotomy is not required while in patients with intraabdominal complications, urgent laparotomy should be undertaken.
Dandy Walker malformation with suboccipital meningocoel
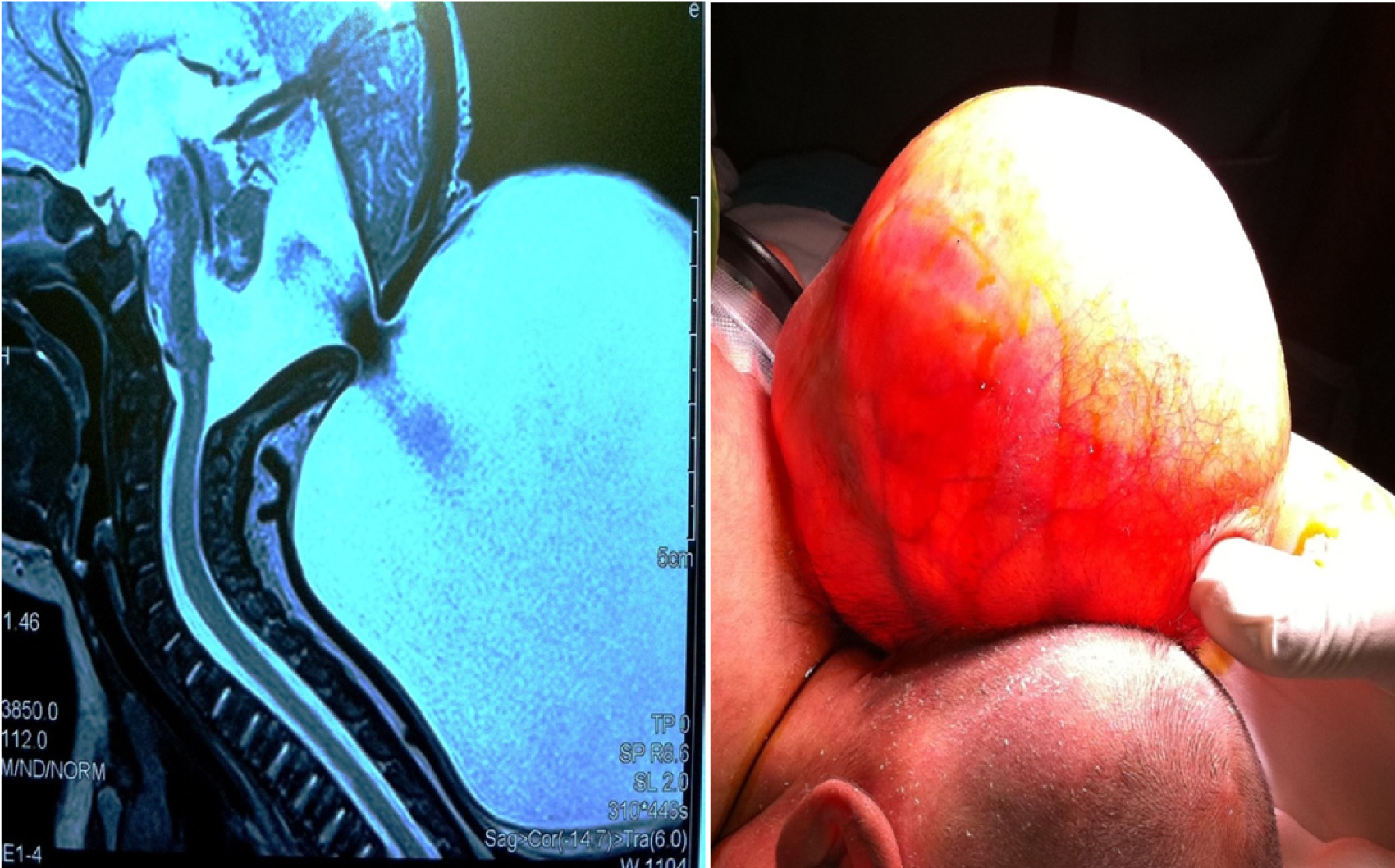
Picture depicting passage of shunt tube through anus

Conclusion
We report this rare case of extrusion of ventriculoperitoneal shunt through anus so as to add to the existing literature of this rare complication so that this complication is managed aggressively and rapidly to minimize morbidity and mortality.
[1]. R Kanojia, SK Sinha, J Rawat, A Wakhlu, S Kureel, R Tandon, Unusual ventriculoperitoneal shunt extrusion: experience with 5 cases and review of the literaturePediatr Neurosurg 2008 44(1):49-51. [Google Scholar]
[2]. A Hai, AZ Rab, I Ghani, MF Huda, AQ Quadir, Perforation into gut by ventriculoperitoneal shunts: A report of two cases and review of the literatureJ Indian Assoc Pediatr Surg 2011 16(1):31-33. [Google Scholar]
[3]. D Sarkar, S Sarkar, Ventriculoperitoneal shunt catheter migration through umbilicus, a rare complicationPediatric Oncall 2010 7(3) [Google Scholar]
[4]. M Altas, M Tutanc, M Aras, ZG Altas, A Arica, Vaginal perforation caused by distal tip of ventriculoperitoneal shunt: Report of a rare complicationPak J Med Sci 2012 28(3):550-51. [Google Scholar]
[5]. SW Low, L Sein, TT Yeo, N Chou, Migration of the abdominal catheter of a ventriculoperitoneal shunt into the mouth: A rare presentationMalays J Med Sci 2010 17:64-67. [Google Scholar]
[6]. A Dagtekin, H Karabag, E Avcı, A Naycı, C Bagdatoglu, A rare complication with ventriculoperitoneal shunt in pediatric casesEge Journal of Medicine 2011 50(1):65-68. [Google Scholar]
[7]. S Vuyyuru, SR Ravuri, VR Tandra, MK Panigrahi, Anal extrusion of ventriculoperitoneal shunt tube: Endoscopic removalJ Pediatr Neurosci 2009 4:124-26. [Google Scholar]
[8]. H Ozturk, M Kashyap, H Ozturk, A Kucuk, M Dosoglu, Transanal protrusion of a ventriculo peritoneal shunt catheterJ Coll Physicians Surg Pak 2012 22:733-34. [Google Scholar]