Fractures of the distal humerus account for approximately 2–6% of all fractures and about 30% of all elbow fractures [1]. Even with development of newer fixation techniques, the treatment of distal humerus fractures remains a challenge to every orthopaedic surgeon. Due to complex anatomy of elbow along with metaphyseal and articular comminution, good results are difficult to achieve [2]. To obtain good results, anatomical reduction with rigid fixation and early range of mobilization is required [3]. Due to the characteristic intra-articular involvement and poor control of fracture fragments with closed treatment these fractures are treated operatively to achieve anatomic reduction and stable fixation of the fractured fragments [4]. Double plate fixation is considered the correct treatment for a comminuted intra-articular fracture of the distal humerus [5–7]. We did a prospective study of parallel plate fixation of fractures of distal humerus in adults.
Materials and Methods
All fresh cases of distal humerus fracture reporting to us from January 2013 to May 2014 were included in this study. Informed written consent was taken from all. The study was approved by Institutional research cell and the Ethical committee. This prospective study included 23 patients. We included both closed and open fractures (Gustillo and Anderson Grade I) of distal end of Humerus in this study. Patient were excluded if they had pre-existing deformity, disability, infection, previous surgical intervention in the involved elbow, unfit for surgery or failure to give consent.
The patients were taken up for surgery after preoperative investigations and fitness for anaesthesia was assured. Digital pneumatic tourniquet was used in all. Intravenous antibiotics were given six hours before surgery and for next two days in postoperative period and further five days oral antibiotics were given. The patients were taken up for surgery after regional/general anaesthesia in lateral decubitus position with arm supported and forearm hanging. All grade I open wounds were debrided and closed. The limb was painted and draped again before proceeding for the exposure of the elbow. Elbow was exposed through standard midline posterior approach with incision beginning 5cm distal to the tip of the olecranon and extending proximally in the arm up to 8cm above the tip of the olecranon. Ulnar nerve was exposed and secured. A ‘V’ shaped Olecranon osteotomy was done to get better exposure of the articular surface in all cases. Bone fragments were reduced and held with ‘K’ wires. Fracture was then fixed with intercondylar screw and 3.5mm reconstruction plates which were placed parallel to each other on medial and lateral columns.
The stability of the internal fixation was tested by moving the elbow through full range of motion.The Olecranon osteotomy was then reduced under direct vision and fixed by figure of ‘8” tension band wiring. After fixation of the osteotomy the elbow was again put through the range of motion to test the stability of fixation.The tourniquet was released and hemostasis achieved over a negative suction drain and the wound was closed in layers. Pressure bandage was applied.
In the postoperative period the the limb was kept elevated. Active movement of fingers and elbow joint were encouraged on the heels of pain from second postoperative day. Suction drain was removed after 24 h. Wound was inspected after after 3-4 days postoperatively. Antibiotics and analgesics were given to the patient till the time of suture removal. Suture/staples were removed on the 14th postoperative day. Post-operative radiographs were obtained as soon as patient was comfortable. Elbow was mobilised through full range of movement atleast twice daily and patient was discharged on 14th postoperative day with instruction to carry out physiotherapy in the form of active flexion-extension and pronation-supination excercizes without loading.
Patient was assessed after 6 wk, 12 wk and 24 wk of surgery. At every follow up a detailed clinical examination was done and patient was assessed subjectively for the pain, swelling, range of joint motion and radiological union. The functional assessment of the patient was done according to Mayo elbow performance index and Quick DASH score.
Results
The present study was undertaken to assess functional outcome of fractures distal end Humerus treated with surgical management with parallel plating. For this purpose, a total of 23 patients were enrolled in the study. The age of patients ranged from 18 to 60 y (mean 39.1±11.5 years). Majority of patients (n=15; 65.2%) were aged above 35 y. There were 16(69.6%) male and 7(30.4%) female patients (M: F : 2.3:1).
The cause of injury was road side accident in 16 patients (69.6%), fall from height in 5(21.7%) patients. Mode of injury was direct in 18 (78.3%) patients and indirect injury in 5 (21.7%) patients. Right side was involved in 16 (69.6%) patients.
All patients reported within one week of injury. Five patients had open fracture (Gustillo grade I).There was no case with neurovascular involvement. One patient had associated injuries (pelvic fracture, femoral shaft fracture). Two patients were unfit for anesthesia due to medical reasons hence operative procedure was done in 21 patients only. Fracture was metaphyseal type in 9 (42.9%) patients, V-type in 6 (28.6%) patients, T-type in 5 (23.8%) patients and Y type in 1 (4.8%) patients. The duration of surgery ranged from 150 to 180 min with a mean of 157.62±9.95 min.
All patients were followed up till one year. Two cases were lost to follow up after six months. At first follow up at three weeks, four (19%) patients showed some induration and oedema at suture line along with mild local increase in skin temperature. This was taken as sign of subclinical infection and treated with oral antibiotics and NSAID’s. The induration and oedema subsided within 10 d of treatment and did not recur later.
In the first week after the procedure the Mayo score was 5.00±01.26 which gradually increased to 96.32±04.96 by year end. DASH score was150±05.34 in first postoperative week and it decreased down to 31.42±2.04 by year end follow up. Similarly range of motion in first week follow up was 21.38±05.70 which improved to 116.1±7.92 by year end follow up [Table/Fig-1]. The improvement in range of motion, MAYO score and DASH score and their statistical significance is shown in [Table/Fig-2].
Showing comparative data of different clinical and functional parameters
| Time Interval | Range of Motion | Mayo score | DASH score |
|---|
| Mean (SD) | Mean (SD) | Mean (SD) |
|---|
| 1st Postop-erative week | (10-50) 21.38±05.70 | (02-08) 05.00±01.26 | (120-167) 150±05.34 |
| 3 weeks follow up | (10-95) 71.67±19.43 | (60-75) 66.43±04.20 | (70-80) 73.57±3.85 |
| 6 weeks follow up | (80-115) 98.33±08.85 | (70-90) 82.62±04.90 | (31-46) 38.14±4.60 |
| 3 months follow up | (95-120) 111.46±06.55 | (85-100) 90.79±04.17 | (30-37) 32.84±2.43 |
| 6 months follow up | (85-120) 115.0±08.50 | (85-100) 93.42±04.43 | (30-37) 31.63±2.06 |
| 1 year follow up | (85-120) 116.1±07.92 | (85-100) 96.32±04.96 | (30-37) 31.42±2.04 |
Showing comparison in changes in range of motion, mayo score and DASH scores
| Time Interval | Change in ROM | Change in Mayo Score | Change in DASH Score |
|---|
| Mean (SD) | p-value | Mean(SD) | p-value | Mean(SD) | p-value |
|---|
| Post Op.-3 weeks | 71.67±19.43 | <0.001 | 61.43±4.23 | <0.001 | -76.43±3.85 | <0.001 |
| Post Op.-12 weeks | 111.46±6.55 | <0.001 | 77.62±4.90 | <0.001 | -117.16±2.43 | <0.001 |
| Post Op.-24 weeks | 115.0±8.50 | <0.001 | 85.79±4.17 | <0.001 | -118.37±2.06 | <0.001 |
| Post Op.-52 weeks | 116.1±7.92 | <0.001 | 88.42±4.43 | <0.001 | -118.58±2.04 | <0.001 |
| 3weeks-3 months | 39.76+19.44 | <0.001 | 91.32±4.96 | <0.001 | -40.68±2.96 | <0.001 |
| 3weeks - 6 months | 43.68+22.71 | <0.001 | 24.21±4.49 | <0.001 | -41.89±3.51 | <0.001 |
| 3weeks-1 year | 44.74+22.93 | <0.001 | 29.74±6.12 | <0.001 | -42.11±3.73 | <0.001 |
| 3 months-6 months | 3.42+10.01 | 0.154 | 2.63±3.06 | 0.001 | -1.21±1.75 | 0.007 |
| 3months-1 year | 4.47+10.39 | 0.077 | 5.53±4.97 | <0.001 | -1.42±1.89 | 0.004 |
| 6 months-1 year | 1.05+2.68 | 0.104 | 2.89±3.03 | 0.001 | -0.21±0.63 | 0.163 |
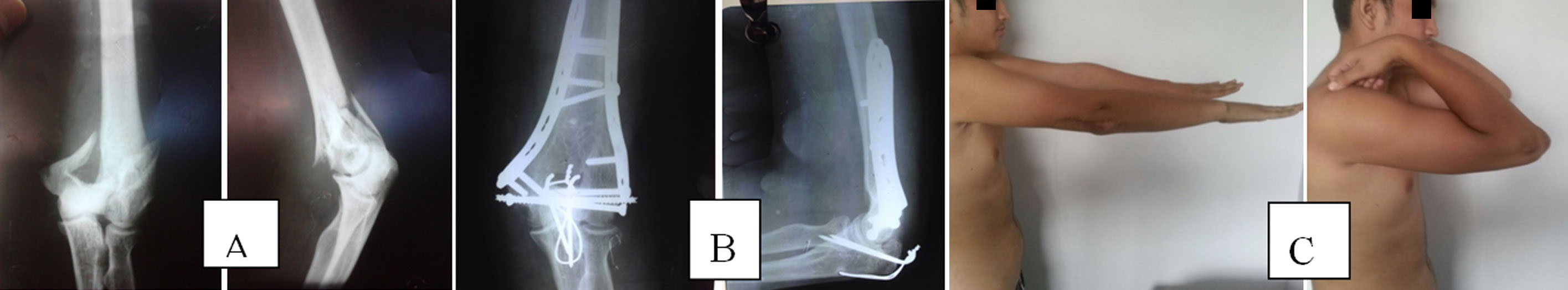
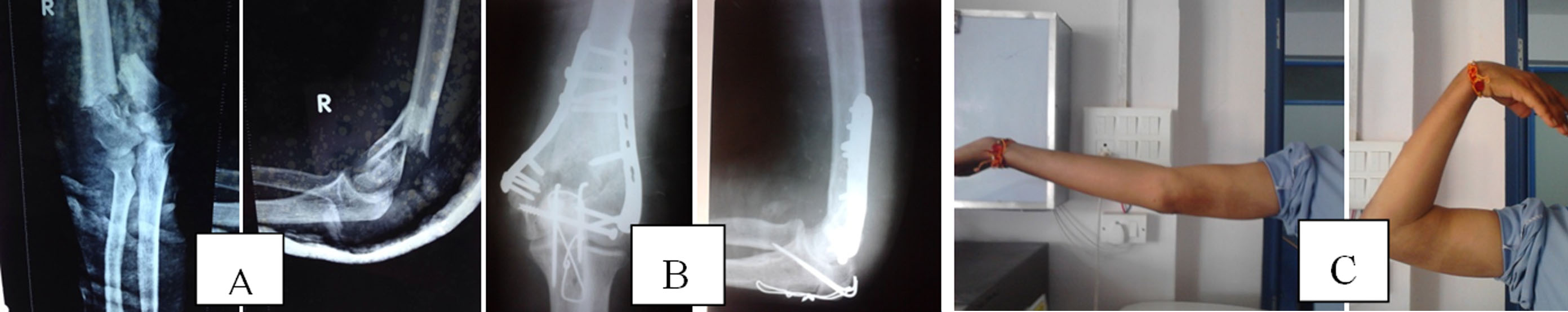
Final assessment showed attainment of full range of motion with united fracture and no angular or rotational deformity in 10 (52.6%) patients. Seven patients (36.8%) had 5o short of full extension with fracture union and no angular or rotational deformity and remaining two patients (10.5%) had 15o Short of full extension with united fracture and no angular deformity or rotation [Table/Fig-3,4].
Showing pre (A) & post operative (B) X-rays along with clinical images(C) showing range of motion
Showing pre (A) & post operative (B) X-rays along with clinical images (C) showing range of motion
Discussion
Both parallel and perpendicular (orthogonal) plating techniques have been advocated for the treatment of intercondylar fracture of humerus and there are several cadaveric biomechanical studies that would support the use of either [8–10]. The concept of parallel plating evolved as orthogonal plating did not provide adequate fixation and enough stability in high percentage of cases.
All our cases achieved union within four months. Nonunion or delayed union is not a problem in these fractures as shown by most of the studies [11–15] [Table/Fig-5].
Showing Outcome in different studies assessing parallel plate fixation
| Sn | Author | Sample size | Follow up | Union | ROM | MEPS | DASH | Complication |
|---|
| 1 | Sanchez-Sotelo et al., [3] | 32 | 24 months | 81.3% | 990 | 85 | - | 18.7% |
| 2 | Athwal et al., [16] | 32 | 27 months | 100% | 970 | 82 | 24 | 53% |
| 3 | Theivendran et al., [17] | 16 | 35 months | 100% | 1030 | 72.3 | 46.1 | 12.5% |
| 4 | Atalar et al., [21] | 31 | 28 months | 100% | 90.20 | 86.1 | 7.6 | 29.0% |
| 5 | Rebuzzi et al., [18] | 7 (A) 6 (C) | 14.8 months 21.3 months | 100% 100% | 1200 1130 | 92.86 94.17 | - | 46.2% |
| 6 | Shin et al., [19] | 18 | - | 100% | Full | - | - | 44.4% |
| 7 | Lan et al., [12] | 21 | 16 months | 100% | 1010 | 86.1 | - | - |
| 8 | Lee et al., [11] | 33 | - | 100% | - | - | - | 6.0% |
| 9 | Flinkkilä et al., [20] | 47 | 3.9 Yrs | 93.6% | 1230 | 88 | - | 15% |
| 10 | Present study | 19 | 12 months | 100% | 1160 | 96.32 | 31.42 | 19.0% |
Mean range of motion (116.1±7.92) at final follow up in our series is greater than that reported by some authors [12,16,17]. But there are also reports which claim full or nearly full range of movement post-operatively [18–20]. Mayo score in different studies has been reported from 72.3 to 96.32. Mayo scores above 90 have been shown to be achieved in only one worker [18]. Higher scores in present study could be attributed partly to the younger age profile of our patients (age <60 y). DASH scores were available in only three other studies and the scores varied substantially. Only two studies showed better DASH scores than our study signifying functional improvement [16,21] [Table/Fig-5].
In the post-operative follow-up period all assessment parameters improved steadily up till the end of follow-up. But this improvement in clinical and functional parameters was significant only in first three postoperative months. In the later follow-up period though the clinical and functional parameters showed improvement but the changes were slow and gradual and statistically not significant (p > 0.001).This indicates that maximum benefit can be achieved with aggressive physiotherapy in first three months of surgery [Table/Fig-2]. This can only be achieved if anatomical rigid fixation is done. Complication rates vary from 6% to 44.4% in different studies. In present study, one deep infection, three superficial suture line infections occurred which resolved with a short course of antibiotics [Table/Fig-5].
Comparison of perpendicular and parallel plating in a single study was done by only one researcher [19]. Statistically no significant difference was found between the outcomes of parallel plating and perpendicular (Orthogonal) plating.
On the basis of results reported in literature, comparison of functional outcome of present study and Perpendicular studies in terms of union rate and functional outcome, range of motion, Mayo score, DASH score and complication was done [Table/Fig-6].
Showing functional outcome of present study and perpendicular plating
| SN | Author | Sample size | Follow up | Union | ROM | MEPS | DASH | Complication |
|---|
| 1 | Aslam et al.,[13] | 20 | 35 months | 100% | 1120 | - | - | 15.0% |
| 2 | Shin et al.,[19] | 17 | - | 88.2% | - | - | - | 35.3% |
| 3 | Tian et al.,[14] | 13 | 19.2 months | 100% | 1200 | 89.6 | - | 30.8% |
| 4 | Lan et al.,[12] | 24 | 16 months | 100% | 1010 | 85 | - | - |
| 5 | Lee et al., [11] | 34 | - | 100% | - | - | - | 8.8% |
| 6 | Leigey et al.,[15] | 15 | 77 days | 100% | 1050 | - | - | 20.0% |
| 7 | Present study | 19 | 12 months | 100% | 1160 | 96.32 | 31.42 | 19.0% |
A comparison of results of present study, and studies reporting results after perpendicular plating was done which shows no significant difference between two groups with respect to union time, mayo score and DASH score [Table/Fig-6]. None of the studies in perpendicular group had used DASH as the criteria for evaluation of outcome hence this comparison could not be made. Complication rates in perpendicular group seem to be slightly lower as compared to parallel group. This may be because some studies have reported both minor and major complications in their outcome while others have not included minor complications. Hence, no difference between the two could be observed based on this parameter.
The success rates were high while complications were lower in present study by fractional margins. However, with respect to range of motion, our results are relatively better. The Mayo Scores also indicated a better outcome in present study. In general our results are similar to those reported by others who did not find a significant difference between two techniques in terms of functional outcome [11,12,18].We achieved excellent union rate, range of motion and functional scores. The results of parallel plating are encouraging and we endorse this method based on the findings of present study.
Conclusion
All cases united within six months with good function hence we can conclude that Parallel plating for intercondylar fracture of humerus is an excellent method of fixation and results are similar to those treated with orthogonal plating.