Development is a continuous process which begins from conception and continues up till maturity. However, during this process several factors like genetic, environmental, nutritional and chronic diseases can have adverse effects of delay in milestone which can be evaluated using four domains of gross motor, fine motor and social and language skills [1]. Developmental delay is defined as significant delay (more than two standard deviations below the mean) in one or more developmental domains [2]. Though no accurate records are available, it is believed that patients presenting with development delay constitute nearly 5-10% of patients presenting as outpatients at various medical centers [3]. Developmental delay may become evident during infancy or early childhood but becomes more apparent & therefore more often diagnosed in early school years [4].
Developmental delay does not represent a diagnosis, but a term used in different clinical presentations and prognosis, which covers a wide range of aetiologies including genetic, metabolic, endocrine, vascular, malformation syndromes, traumatic, infections, toxins & environmental causes [1,5]. Careful evaluation and investigation can reveal a cause in 55-85% cases with developmental delay [1,3,6–9]. This wide variation could be attributed to patient selection criteria where high proportions are reported; some of the reported abnormalities are in children where diagnosis would be obvious clinically. The yield of useful diagnostic abnormalities is higher (more than 60%) using newer techniques and in a population selected for developmental delay with clinical features [9].
Brain MRI is one of the major investigation of these patients, and based on previous studies, about 60% of cases have abnormal brain MRI [1,2]. A complete study will provide important information about the patient, the rate and type of brain abnormalities. It helps to identify these diseases and their prognosis, preventing the recurrence and parent counseling. The present study was undertaken prospectively in 81 consecutive patients presenting to the Pediatric OPD of a tertiary hospital for evaluation of developmental delay. Radiological observations with specific reference to MRI study were made along with a review of literature.
Materials and Methods
Study Design
A prospective, observational & descriptive study of MRI of the Brain in 81 paediatric patients (46 Males and 35 Females) presenting with developmental delay in Deccan College of Medical Sciences, Hyderabad; over a period of three years (Sept 2011 to Sept 2014). Patients were categorized based on age group, anatomical structures involved and aetiology. The patients were further categorized into two groups based on the history and the clinical details reviewed from their MR referral sheets as having developmental delay only and those with additional features such as epilepsy, neurological deficits, etc as developmental delay plus.
Inclusion and Exclusion Criteria
Consecutive patients who were referred for brain MRI with developmental delay, aged between three months to 12 years, admitted for the first time to diagnose the cause of delay are included in the study. Patients with known Genetic Disorders such as Down syndrome, Turners Syndrome, Metabolic Disorders like Rickets and Scurvy, Protien Energy Malnutrition, Infections like Tonsilitis, Pneumonia or any other Communicable disease in active stage were excluded.
Neuroimaging was sorted as the choice of investigation, due to financial constraints & lack of availability of advanced metabolic and genetic tests. All children with developmental delay were investigated with MRI scans of the brain, on a 1.5T Siemens Magnetom Essenza (16 channel) & Magnetom C, 0.35T after making the child sleep or sedated. The sequences used were: Axial T1TSE, Axial T2TSE, Axial T2 FLAIR, Axial EP2D diffusion, Axial T2TIRM, Axial PDTSE, Axial 3D T2SWI, Coronal T1TIR, Coronal T2TSE, Sagittal T1TSE. Clinical and demographic details of enrolled patients were noted down in the predesigned performa.
Paediatric MRI Brain Protocol
Sedation
For optimal image quality enabling precise diagnosis patients have to remain motionless. Infants were examined unsedated & a very safe and simple “feed and scan” technique was used; in which the infants were fed and waited until they fell asleep, after which the scan was performed.
While the older children were either sedated by oral or IV drugs under the consent and presence of the pediatrician or sedated by using anesthetic drugs by the anesthetist in his presence. Consent of the parent and pediatrician were taken before the procedure. The children were generally given Syrup Pedicloryl (Triclofos Sodium) orally of a dosage of 25 mg/kg body weight/dose or Syrup Chloral Hydrate with a dosage of 5 to 10mg /kg. Short acting general anesthesia was given under supervision in children, who were not getting sedated by oral drugs.
Prerequisites for such anesthesia were fasting for four hours, intravenous access, vital signs monitoring, emergency equipment, and physicians who were trained in pediatric airway management. Premedication drugs like injection I.V Glycopyrilate 0.3mg/dose, injection Zofer (Ondansetron) 2mg/dose and I.V Propofol with a dosage of 1-2mg/kg bodyweight were used. All children were monitored with ECG and pulse oximetry and continuous oxygen inhalational was advocated during the entire scan. Strict vigilance was observed for two hours post procedure by the trained team.
The patients were placed in supine position & head was placed in a specifically designed 24cm split, clear receiver coil. Immobilization of the head was achieved by surrounding the head with an air-evacuated bag filled with polystyrene balls; following which the scan was performed under the review of Radiologists in the workstation.
The following structures were systematically evaluated following to Widjaja et al., [9] protocol.
Ventricles: Size and morphology.
Corpus callosum: Thickness and morphology.
Gray and white matter: The sulcation and gyration of the gray matter based on normal MR brain anatomy [10].
Basal ganglia: morphology.
Brain stem: morphology.
Cerebellum: morphology. The term cerebellar atrophy was used if the cerebellum was small with shrunken folia and large cerebellar fissures or if it had been shown to undergo progressive volume loss. A structure was considered dysplastic if disorganized in development, such as abnormal folial pattern or presence of heterotopic nodules of gray matter [10].
Assignment of anomalies: The MRI findings were divided into five groups as described by Williams [11]:
Normal.
Traumatic/Neurovascular Diseases.
Congenital & Developmental disorders.
Metabolic and neurodegenerative diseases.
Neoplastic diseases.
Nonspecific findings – includes ventriculomegaly, enlarged subarachnoid spaces and delayed myelination, etc.
Results
Normal MRI findings were seen in 32% (26 cases) of paediatric patients presenting with developmental delay. These children were advised further evaluation to diagnose the aaetiology of developmental delay. Abnormal morphological appearance was seen in the remaining 68% ( 55 cases) as shown in [Table/Fig-1]. Based on history and clinical details, it was seen that only 11% patients presented with only developmental delay rest 89% presented with developmental delay and additional features such as epilepsy, neurological deficits, abnormalities of head size, facial dysmorphism, cleft lip/palate, visual and auditory disturbances, gait disturbances, motor disturbances, social and cognitive problems, consanguinity or bad obstetric history. The yield was very high in children with developmental delay plus as compared to children with only developmental delay as depicted in [Table/Fig-2].
Age and sex distribution of study population with Normal and abnormal MRI
| Parameter | Abnormal (N=55) | Normal (N=26) |
|---|
| Age | Number | % | Number | % |
|---|
| 3 months – 1 y | 21 | 38.2 | 5 | 19.2 |
| 1-2 y | 13 | 23.6 | 7 | 26.9 |
| 2-5 y | 6 | 10.9 | 7 | 26.9 |
| 5-8 y | 8 | 14.5 | 4 | 15.5 |
| 8-12y | 7 | 12.8 | 3 | 11.5 |
| Sex |
| Males (n=46) | 31 | 56.4 | 15 | 57.7 |
| Females (n=35) | 24 | 43.6 | 11 | 42.3 |
The Clinical presentation of study population with normal and abnormal MRI
| Parameter | Abnormal (N=55) | Normal (N=26) |
|---|
| Clinical presentation | Number | % | Number | % |
| Only Developmental Delay | 6 | 11 | 2 | 7.7 |
| Developmental Delay Plus | 49 | 89 | 24 | 92.3 |
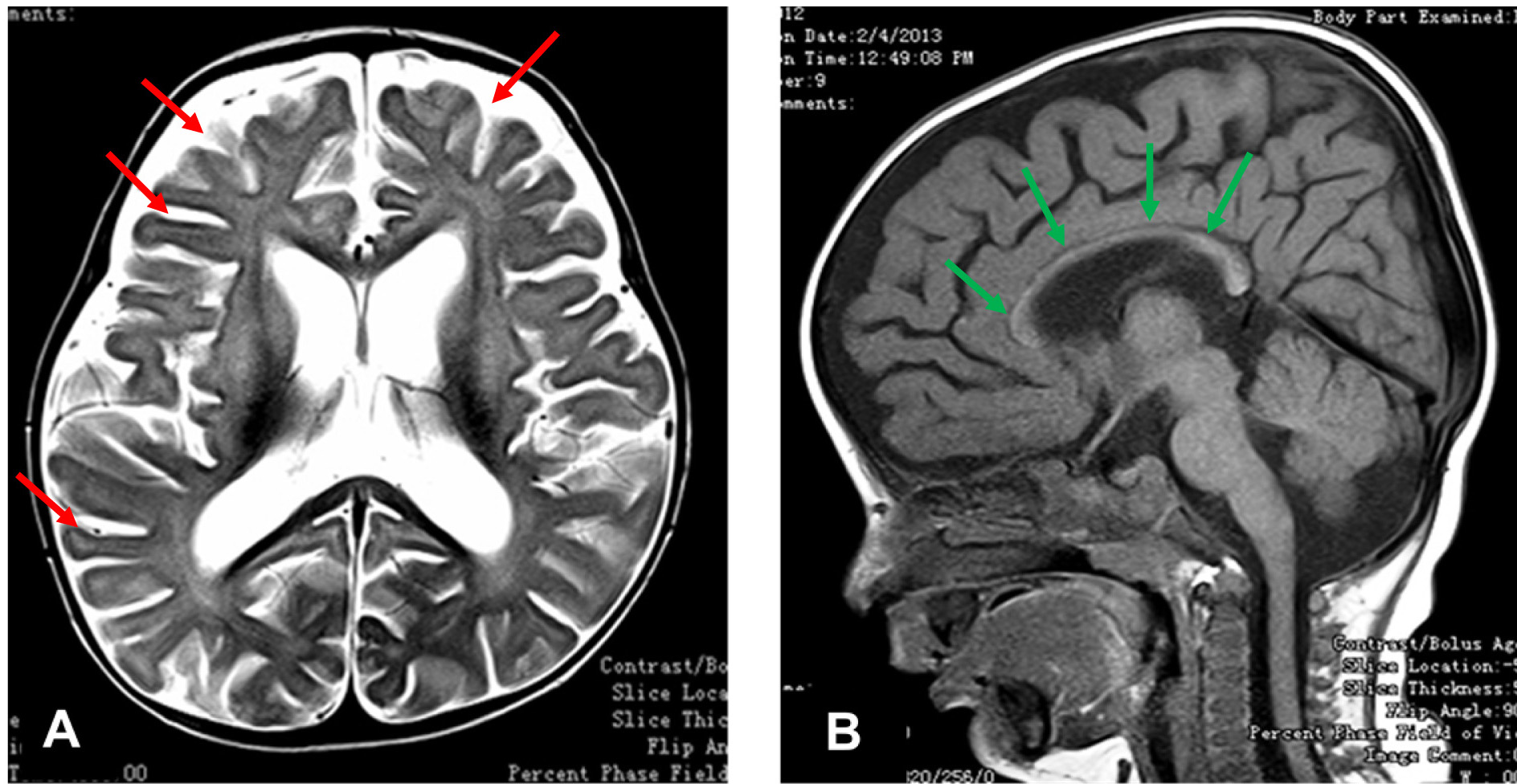
The distribution of affected anatomical structures in patients with abnormal MRI (55 cases) was analysed and is presented in [Table/Fig-3]. Abnormalities of ventricles and White matter mainly the corpus callosum were found to be most common; as seen in 62% and 58% cases respectively. The proportion of children with abnormal findings in cerebellum, gray matter and brainstem were 16%, 10% and 9% respectively. Nonspecific abnormalities were found in 22% of children; like Prominent Virchow-Robin spaces in six cases, abnormal basal ganglia in four cases and abnormal sulcation in two cases. Analysis of 81 cases based on the aetiological factors showed normal MR features in 26 cases (32%). 55 cases with abnormal MRI were further subgrouped; of which 25 cases (31%) had findings consistent with Traumatic/ Neurovascular Diseases. The proportion of children with Congenital & Developmental, Metabolic and Degenerative, neoplastic and non specific were 17%, 10%, 2.5% and 7.5% respectively as shown in [Table/Fig-4].The most common abnormality encountered in present study was Traumatic / Neurovascular Diseases like Hypoxic Ischemic Encephalopathy (HIE) depicted in [Table/Fig-5a,b]. Majority of these children belonged to four to 24 months of age group and 63% of them were males and 37% were female children. White matter, ventricles and corpus callosum were invariably affected in almost all the cases of HIE.
MRI findings in relation to anatomical structures (N=55)
| Anatomical structures | No. | % |
|---|
| Ventricles | 34 | 61.8 |
| White Matter | 32 | 58.2 |
| Cerebellum | 9 | 16.4 |
| Gray Matter | 6 | 10.9 |
| Brainstem | 5 | 9.1 |
| Nonspecific | 12 | 21.8 |
Aetiological classification based on MRI findings
| MRI Findings | Number | % |
|---|
| Normal study | 26 | 32 |
| Traumatic / Neurovascular Diseases | 25 | 31 |
| Congenital & Developmental | 14 | 17 |
| Metabolic and Degenerative | 8 | 10 |
| Neoplastic | 2 | 2.5 |
| Non Specific | 6 | 7.5 |
| Total | 81 | 100 |
Hypoxic ischemic encephalopathy in seven months male child presenting with developmental delay and microcephaly. A. T2W axial image showing mild loss of deep white matter volume evidenced by prominent sulcal spaces (red arrows) with mild prominence of ventricular system B. T1W midsaggittal image showing diffuse thinning of corpus callosum (green arrows)
The Congenital and developmental abnormalities of the brain found in 14 cases had following syndrome complexes either as single entity or in combination.
Dandy-Walker Malformation (3 cases).
Holoprocencephaly.
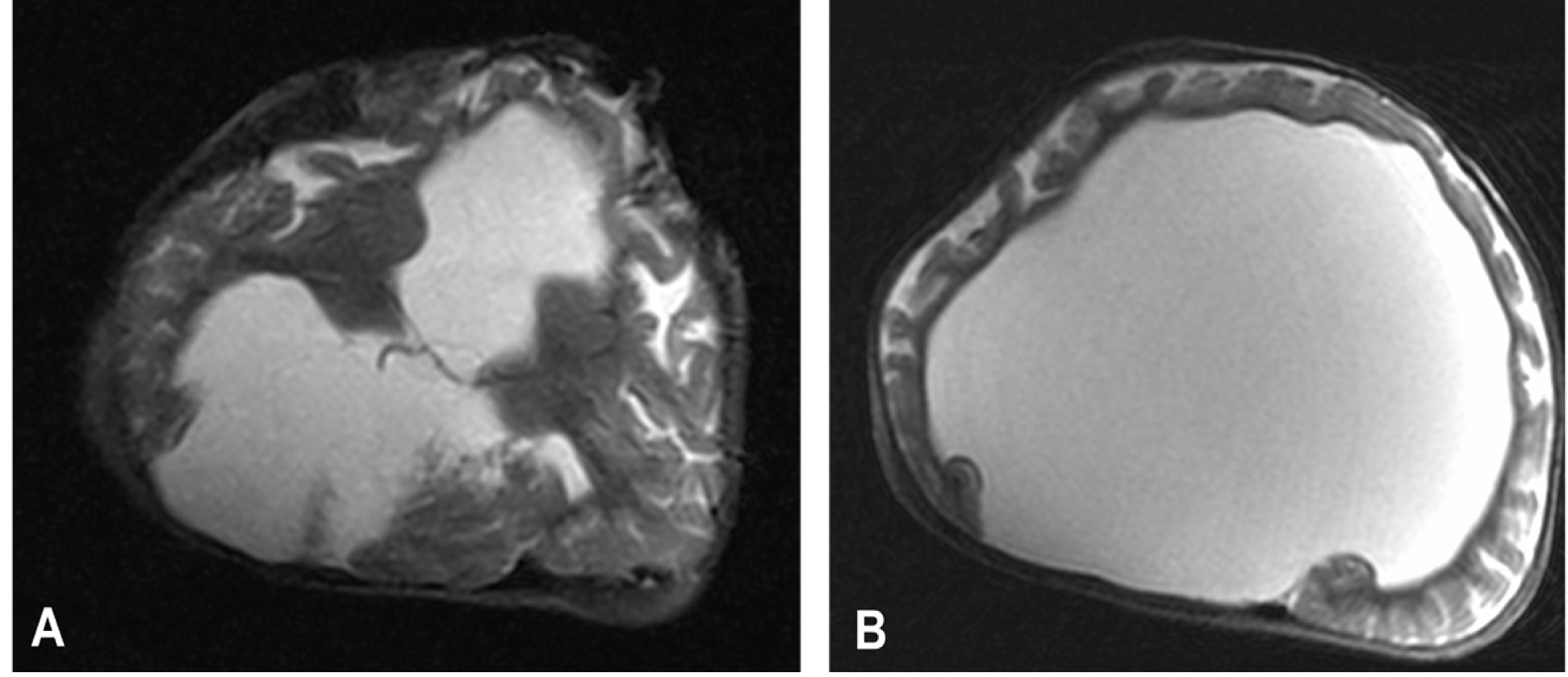
Alobar (1 case) shown in [Table/Fig-6a,b].
Semilobar (2 cases).
Lobar (2 cases).
Joubert syndrome (1 case).
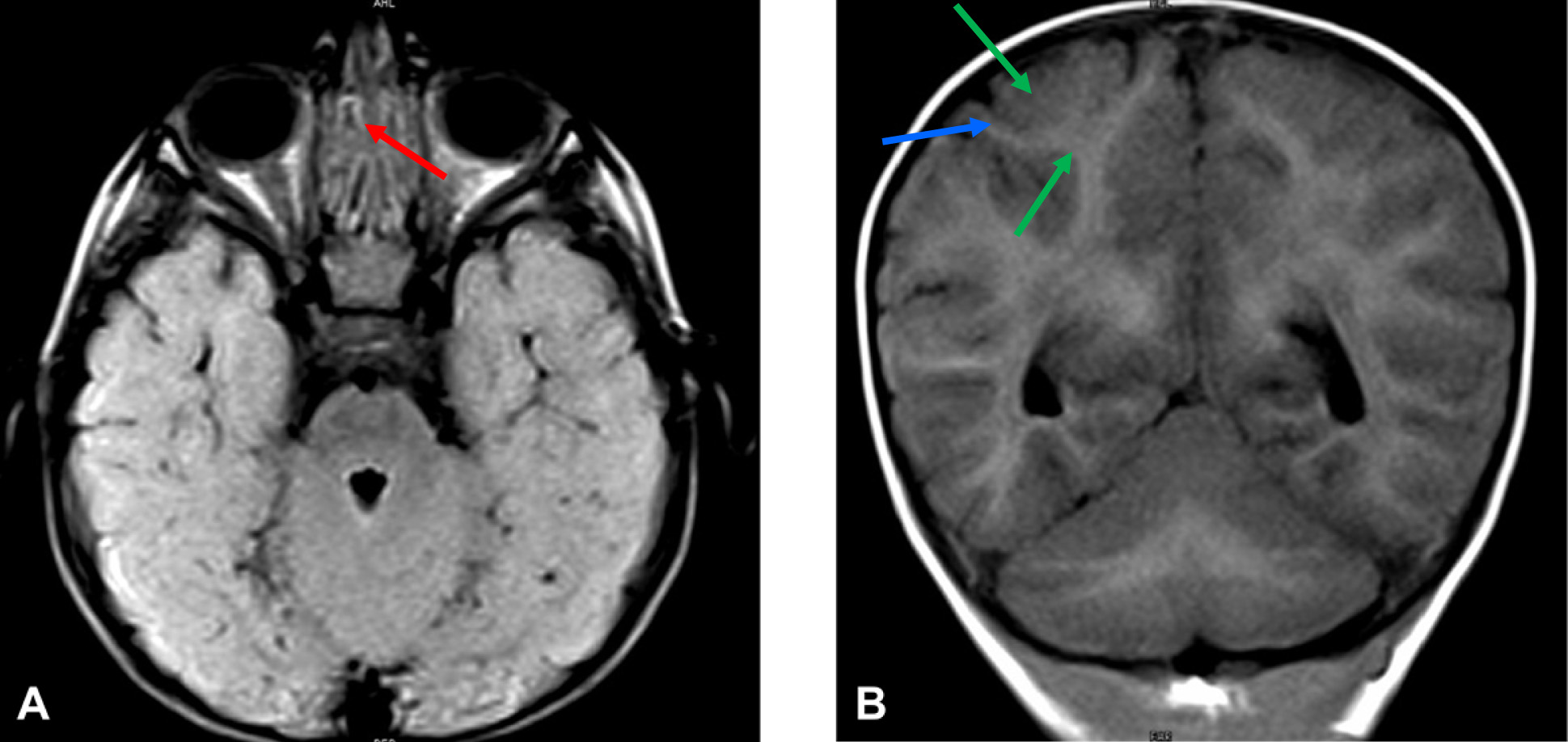
Rhombencephalosynapsis (1 case) shown in [Table/Fig-7a,b].
Aicardi syndrome (1 case).
Megelencephaly, Polymicrogyria, Polydactyly, Hydrocephalus Syndrome (MPPH) (1 case).
Hemimegalencephaly with cortical dysplasia (2 cases).
Microcephaly (1 case).
Lissencephaly (1 case).
Alobar holoprocencephaly in a four months female child presenting with microcephaly, cleft palate, dysmorphic features, severe failure to thrive, seizures and developmental delay. T2W Axial MR image showing A. absent midline structures like septum Pellucidum, corpus callosum, falx, interhemispheric fissure. B. unsegemented rim of brain tissue seen anteriorly (pan cake) surrounding a dilated and undifferentiated monoventricle
Rhombencephalosynapsis in a 14 months male child presenting with nystagmus, aggressive behavior and developmental delay. A. Axial MR image showing fusion of cerebellar hemispheres (red arrow) with absent vermis B. Coronal MR image showing transverse foliae (green arrows) & inter folial sulci (blue arrow)
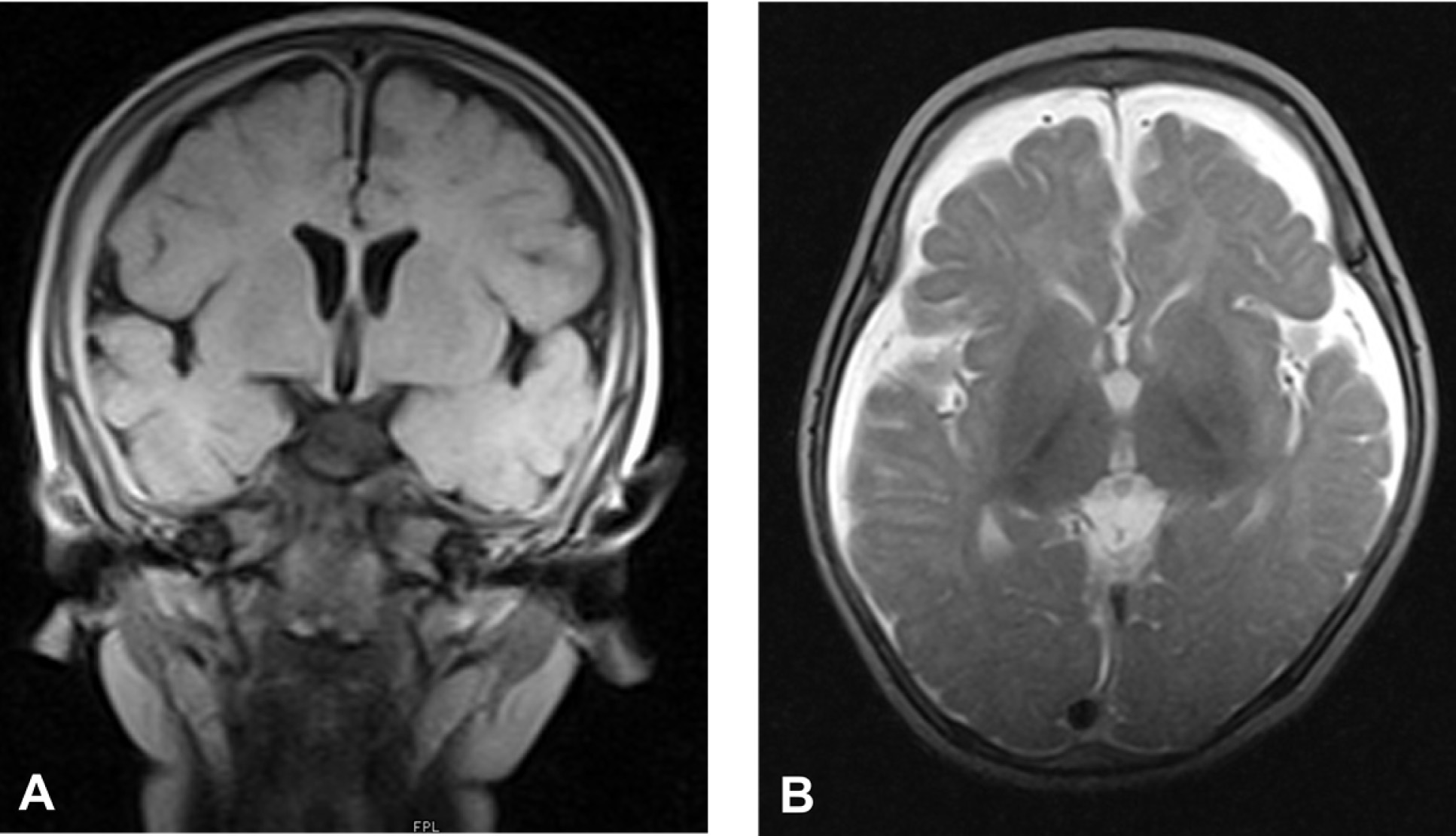
Metabolic and degenerative diseases were found in eight cases; all of which had white matter and ventricle related abnormalities as shown in [Table/Fig-8a,b]. Cerebral atrophy, basal ganglia and macrocephaly were present in 40% of the cases and cerebellum was involved in only 20% of the cases. Neoplasia was found in two cases; one case had teratoma and another one had medulloblasoma. Children with non-specific MRI findings had isolated ventriculomegaly in three cases and Delayed myelination in three cases.
Mucopolysaccharadosis Type1(Hurlers) in a one year male child presenting with developmental delay with seizures A. FLAIR Coronal image showing diffusely thickened meninges covering the cerebral hemispheres B. T2W Axial image shows moderate degree of cortical atrophy with poor gray white matter interface and altered signal of white matter
Discussion
Evaluation of developmental delay was done in 81 consecutive pediatric patients of age group three months to 12 years referred for MRI from our Pediatric ODP. The proportions of children having abnormal MRI findings in our study of 81 cases could get a definitive diagnostic yield of 68% (55 cases). Similar yield of MRI has been reported by Momen et al., [1], Shevell et al., [3], Pandey et al., [6], Koul et al., [7], Battaglia et al., [8] and Widjaja et al., [9] who had a yield of 58.6%, 65.5%, 63.8%, 71.8%, 80.8 and 84% respectively. Wide range of such yield could be due to the patient selection criteria and awareness about investigating such children in different population group. We had included all children referred to us with developmental delay, irrespective of their clinical features & its severity, whether they were syndromic or nonsyndromic.
Neuroimaging by MRI has an indispensable role in evaluating a child with developmental delay and the aetiological yield can be increased if other associated clinical & neurological signs and symptoms are taken into the inclusion Criteria [3,9].
Most of the children with abnormal MRI findings in our study were in age group of three to 12 months (38%) with the next peak at one to two years (24%). Males (57%) were slightly more in number than females (43%) although there is no considerable difference. Similar age of presentation and sex incidence was noted in the study performed by Momen et al., [1].
The 55 cases with abnormal MRI were evaluated for involvement of various anatomical structures. Abnormalities of ventricles and White matter mainly the corpus callosum were most common; seen in 62% and 58% cases respectively. Widjaja et al., [9] studied 90 such children and found that Ventricles (48%) and Corpus Callosum (44%) were the most commonly involved structures, while the other structures involved were almost similar to present study.
Based on the MRI findings, we have classified MR features into various aetiologies as described in [Table/Fig-4]. Momen et al., [1] has classified their MRI findings into aetiological categories; in which Traumatic/Neurovascular Diseases (Hypoxic Ischemic Brain Injury) ranked the highest while other categories were almost as similar to our study except for Congenital and Developmental Anomalies which is slightly lesser than what we have encountered.
The congenital and Developmental Anomalies have distinctive clinical and radiological findings, and their identification is very important in order to prevent recurrence and helps in parent counseling [12]. We have found 14 such cases (17%); which fit into this category; whereas Momen et al., [1] reported a slightly higher incidence which could be explained by the religious beliefs that these patients follow, of not terminating the pregnancy in antenatally diagnosed abnormality.
The present study had eight cases included in Degenerative/ Metabolic subgroup; of which one case of mucopolysacroidodis, one of Alexander’s disease, two cases of dysmyelination and four cases were of leucodystrophies. Two cases presenting with developmental delay had neoplastic origin. Six cases were nonspecific; of which Three had isolated ventriculomegaly and the other Three had delayed myelination. Moes et al., [13] also observed similar incidence of Degenerative/ Metabolic Diseases causing developmental delay.
MR imaging is an important part of the comprehensive evaluation of children with developmental delay, as many specific aetiologic and pathophysiologic conditions that lead to developmental delay can be detected easily [14–18].
Conclusion
Developmental delay presents with a wide spectrum of aetiologies, clinical findings and MRI features ranging from completely normal to abnormal. The present study could establish the various morphological appearances of developmental delay on MRI and further categorize them into various subgroups paving way for treating clinicians to plan proper management and parent counseling. Further serial and sequential MRI may be necessary to ascertain disease progression. Advances in MR Imaging technologies like Functional MRI, MR Spectroscopy, Diffusion Tensor Imaging & Tractography especially in structurally normal brain of such children, would provide more yielding information.