Giant Submucosal Lipomatous Polyp Causing Perforation of Sigmoid Colon: A Case Report and Review of Literature
Lakshman Kumar1, Triza Kumar Laksman2
1Assistant Professor, Department of Surgery, DMWIMS, Wayanad, Kerala, India.
2Assistant Professor, Department of Obstetrics and Gyanecology, DMWIMS, Wayanad, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kumar Lakshman, #159, 4th Main, 3rd Block, 3rd Stage, Basaveshwarnagar, Bangalore-560079, India.
E-mail: drkumarlakshman@gmail.com ,drkumarlakshman@yahoo.co.in
Colonic lipomas are rare benign tumours that are usually asymptomatic. Large colonic lipomas can present with symptoms such as constipation, abdominal pain, bleeding per rectum, and intussusception. We report the case of an 82-year-old man presenting with sudden onset lower abdomen pain and features of peritonitis. An exploratory laparotomy revealed a perforation of sigmoid colon with a fleshy mass protruding through the perforation. No case of spontaneous perforated sigmoid colon by submucous giant lipoma is reported yet in the literature. We discuss the details of first such case, our management, the outcome and also briefly review the literature.
Giant colonic lipoma, Gastrointestinal lipomas, Limited resection anastomosis, Spontaneous perforation, Submucosal lipoma, Submucosal colonic lipoma, Sigmoid colon lipoma
Case Report
An 82-year-old man presented to the Emergency department of our hospital with chief complaints of severe lower abdomen pain, and fever since morning. He gave history of frequent bloating sensation of abdomen associated with constipation. The pain was sudden in onset following straining while defecating in the morning of the same day. On examination there was no icterus or pallor. Patient was very dehydrated, tachypnoeic with tachycardia. The abdomen was distended with diffuse abdominal guarding. Bowel sounds were absent. Patient was admitted and investigated with a provisional diagnosis of Hollow viscus perforation. Blood examination revealed counts to be elevated and chest X-ray showed gas under the diaphragm. After resuscitating the patient and correcting the metabolic derangements he was taken for exploratory laparotomy.
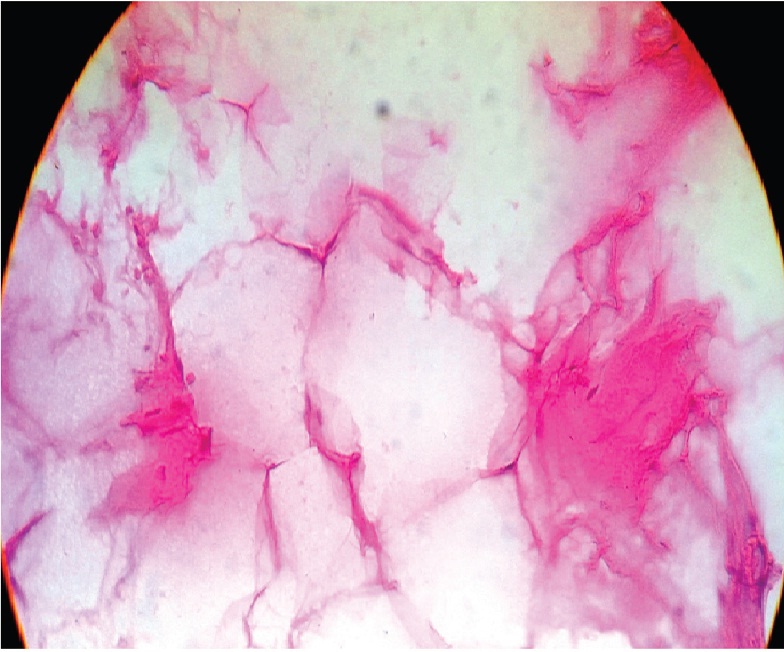
On opening the peritoneum, faecal peritonitis was evident. A thorough peritoneal wash was given and site of perforation was looked for. The small bowel was sequentially traced for a breach in the wall starting from the terminal ileum, but there was no breach in the wall. The large bowel was traced from ceacum distally. The sigmoid colon just proximal to recto sigmoid junction revealed the site of perforation of about 4cm transversely [Table/Fig-1]. Through the perforation a pedunculated smooth surfaced growth of about 5x6cm was protruding out through the tear in the sigmoid colon. The proximal colon was not dilated or thinned out as one would expect in chronic cases of obstruction. The rest of colon and liver was palpated for synchronous lesions/Secondaries and found to be absent. A limited resection of the sigmoid colon with primary resection anastomosis with transverse colon diversion colostomy was performed. The specimen was sent for HPR which was suggestive of an Intestinal submucosal lipomatous polyp [Table/Fig-2]. 10x view section shows normal mucosa with underlying adipocytes(arrow) within submucosa and muscular layer & [Table/Fig-3] 40x view of the lipocytes.
The patient postoperatively developed septicaemia and needed prolonged ICU care. He was discharged on the 18th Post operative day.
Discussion
Lipomas of the colon are rare benign tumours with eextremely low malignant potential. They are the second most common benign colonic tumour after adenomatous polyps [1]. Colonic lipomas in life are usually asymptomatic and by autopsy prevalence reports they are again mostly incidental findings(0.2-0.5%) [2]. They account for 4% of all benign tumours of the gut [3]. The commonest site for large bowel lipomas are the ascending colon, ceacum, transverse colon(including both hepatic and splenic flexures), descending colon, sigmoid colon and the rectum and 90% of these are usually submucosal [4].
When symptomatic these present with pain, bleeding, intussuception or partial obstruction, perforation [5]. Even though perforation is a known complication, usually following endoscopic excision, no case of spontaneous perforation of colon by a submucosal lipoma has been reported.We report the first case of spontaneous perforation of sigmoid colon by a submucosal lipoma in literature.
In our patient the lipoma however manifested typically as an obstructive lesion which had totally obstructed and caused a perforation and the lesion was lying out through the tear in the sigmoid colon.Most Lipomas [<2cm in the largest diameter] are usually asymptomatic, and as the size exceeds 4 cm (Giant Lipomas>4cm) nearly 75 percent of these lipomas tend to become symptomatic, a vast majority of them presenting with intussusceptions [6-8]. Whether the lipoma caused the tear in the sigmoid colon or was it a mere coincidence that the tear occurred at some point and the lipoma just presented through it, is debatable. Reasons for the hypothesis of the colonic submucous lipoma causing the perforation is that there was no other local pathology that could have caused a perforation of the sigmoid colon and against this hypothesis is that the proximal colon didn’t show signs of long standing obstruction and thinning of the proximal colon which again points towards an acute insult.
Lipomas pathologically are well differentiated deposits of adipocytes in the connective tissue of the colon. Sarcomatous changes in these colonic lipomas have been reported only in a few cases [9]. Intermittent torsion and ischemia can give rise to an ulcerated fungating mass that may give a pseudomalignant appearance on colonoscopy [10]. The greatest clinical significance of submucosal lipomas lies in their potential to be confused with adenomatous polyps or other aggressive pathology [11]. Despite recent diagnostic innovations it has been reported that the preoperative diagnostic accuracy is only about 62% [12]. Hence, in most cases the final histopathological is arrived only after excision of the lipoma [1].
The management of these colonic submucosal lipomas starts with screening and these should start in fourth to sixth decades of life as these show peak incidence in this age group.The screening options include per rectal examination, stool occult blood, Barium studies, contrast enhanced computed tomography (CECT) and finally a biopsy through colonoscopy remains the gold standard to diagnose it.CECT are better for subserosal or extra mural lipomas [13] [Table/Fig-4].
For symptomatic lesions the best treatment option is still controversial and includes excision either via endoscopically or by Laparoscopic or open surgery. Endoscopic removal is preferable over surgical excision if it can be done safely without risking perforation. Surgical resection is an option in giant lipomas and for complications of the lipoma which include intussusceptions, bleeding, obstruction, perforation [1]. In cases like our patient, the only option was exploratory laparotomy.

Sigmoid lipomatous polyp labelled Microscopic 10xview

Sigmoid lipomatous polyp microscopic 40x view
Salient features of some symptomatic colonic submucous lipomas, their common presentation and treated modality reported in literature
| S. No. | Author | Year | Salient features of the case | Treatment approach |
|---|
| 1 | Creasy TS et al., [14] | 1987 | Obstruction & bleeding | Colonoscopic resection/ Colonic resection |
| 2 | Ryan J et al., [15] | 1989 | Abdominal pain & gastrointestinal bleeding | Limited colectomy as if for carcinoma or angiodysplasia |
| 3 | Rogy MA et al., [7] | 1991 | 13 of the 17 cases presented with colicky pain, abdominal discomfort, blood-stained feces / rectal bleeding and altered bowel habits and 4 cases were asymptomatic | Colonoscopic resection/ Colonic resection |
| 4 | Bahadursingh AM et al., [8] | 2003 | Abdominal pain, Intestinal obstruction | Laparotomy & Resection anastomosis |
| 5 | Ghidirim G et al., [16] | 2005 | Crampy right lower abdominal pain | Right hemicolectomy |
| 6 | Lin MW et al., [5] | 2007 | Right lower abdomen pain, obstruction | Laparascopic Assisted resection |
| 7 | Lazaraki G et al., [17] | 2008 | Lower abdominal pain | Failed Colonoscpoic resection |
| 8 | Mandal S et al., [2] | 2010 | Abdominal pain, Intestinal obstruction | Laparotomy & Resection anastomosis |
| 9 | Ongom PA et al., [13] | 2012 | Abdominal pain, Intestinal obstruction | Laparotomy & Resection anastomosis |
| 10 | Present Case | 2014 | Abdominal pain, peritonitis, hollow viscus perforation | Laparotomy & Limited resection anastomosis |
Conclusion
Submucosal lipomatous polyps are rare and due to lower incidence and atypical presentations they shall remain as diagnostic dilemmas. In cases of hollow viscus perforation causing faecal peritonitis, secondary to obstructive lesions apart from the common malignant lesions, among the benign lesions submucosal lipomatous polyps are to be considered.
For our patient follow up colonoscopy was normal. The transverse diversion colostomy was closed after 3 months.The patient was free of symptoms at 4 month follow up.
[1]. Lazaraki Georgia, Tzilves D, Tragiannidia D, Patakiouta Frideriki, Pilpilidis I, Giant lipoma of the Sigmoid colon:Spontaneous expulsion 12 days after failure of endoscopic resection.Report of a case and review of literatureAnn of Gastroenterology 2008 21(1):55-58. [Google Scholar]
[2]. S Mandal, V Kawatra, KK Dinghra, P Gupta, N Khurana, Lipomatous Polyp presenting with intestinal intussuception in adults:report of four casesGastroenterology Research 2010 3(5):229-31. [Google Scholar]
[3]. G Nallamothu, DG Alder, Review Large Colonic LipomasGastrenterology & Hepatology 2011 7(7):490-92. [Google Scholar]
[4]. B Marra, Intestinal occlusion due to a colonic lipoma. Apropos 2 casesMinerva Chir 1993 48(18):1035-39. [Google Scholar]
[5]. MW Lin, KH Chen, HF Lin, HA Chen, JM Wu, SH Huang, Laparoscopy- assisted resectionofileoilealintussuception caused by intestinal lipomaJ Laparoendosc Adv Surg Tech A 2007 17(6):789-92. [Google Scholar]
[6]. K Kitamra, S Kitagaw, M Mori, Y Haraguchi, Endoscopic correction of intussusceptions and removal of acoloniclipomaGastrintest Endosc 1990 36:509-10. [Google Scholar]
[7]. MA Rogy, D Mirza, G Berlakovich, F Winkelbauer, R Rauhs, Submucous large bowel lipomas-presentation and management. An 18 year studyEur J Surg 1991 157:51-55. [Google Scholar]
[8]. AM Bahadursingh, PL Robbins, WE Lango, Giant submucosal sigmoid colon lipomaAm J Surg 2003 186:81-82. [Google Scholar]
[9]. E Gutsu, G Ghidirim, I Gagauz, I Mishin, I Iakovleva, Liposarcoma of the colon: A case report and review of literatureJ Gastrointest Surg 2006 10:652-56. [Google Scholar]
[10]. P Martin, B Sklow, Adler Large colonic lipoma mimicking colon cancer and causing colonic intussusceptionDig Dis Sci 2008 53:2826-7. [Google Scholar]
[11]. SA Pfeil, MG Weaver, FW Karim, P Yang, Colonic Lipomas:outcome of endoscopic removalGastrointest Endosc 1990 36:435-38. [Google Scholar]
[12]. M Bardajv, F Roset, R Caps, MF Sant, J Fernandez Layos, Symptomatic colonic lipoma:differentialdiagnoss of large bowel tumorsInt J Colorect Dis 1998 13:1-2. [Google Scholar]
[13]. PA Ongom, H Wabinga, RL Lukande, A giant intraluminal lipoma presenting with intussusceptions in an adult: a case reportJ Med Case Rep 2012 6:370-73. [Google Scholar]
[14]. TS Creasy, AR Baker, IC Talbot, PS Veitch, Symptomatic submucosallipoma of the large bowelBr J Surg 1987 74(11):984-86. [Google Scholar]
[15]. J Ryan, JE Martin, DJ Pollock, Fatty tumours of the large intestine: a clinicopathological review of 13 casesBr J Surg 1989 76(8):793-96. [Google Scholar]
[16]. G Ghidirim, I Mishin, E Gutsu, I Gagauz, A Danch, S Russu, Giant submucosallipoma of the cecum: report of a case and review of literatureRomanian J Gastroenterol 2005 14(4):393-96. [Google Scholar]
[17]. G Lazaraki, D Tzilves, D Tragiannidis, F Patakiouta, I Pilpilidis, A Gatopoulou, “Giant” lipoma of the sigmoid colon: spontaneous expulsion 12 days after failure of endoscopic resection. Report of a case and review of the literatureAnn Gastroenterol 2008 21(1):55-58. [Google Scholar]