Brachial plexus block has a long history existing till date, providing surgical anaesthesia and postoperative analgesia [1]. Bupivacaine is frequently used as the local anaesthetic for brachial plexus anaesthesia because it offers the advantage of providing a long duration of action and a favourable ratio of sensory to motor neural block [2,3]. Bupivacaine binds to the intracellular portion of sodium channels and blocks sodium influx into nerve cells, which prevents depolarization. Amide group local anaesthetics such as bupivacaine are metabolized primarily in the liver via conjugation with glucuronic acid. However, with clinical use, it was noted that using racemic mixture of bupivacaine resulted in cardiac and central nervous system toxicity in some patients [4–6].
Ropivacaine is a long-acting amide local anaesthetic with a potentially improved safety profile when compared to bupivacaine [7,8]. Ropivacaine is less lipophilic than bupivacaine and is less likely to penetrate large myelinated motor fibres, resulting in a relatively reduced motor blockade. Ropivacaine has a greater degree of motor sensory differentiation. It has selective action on the pain-transmitting A β and C nerves rather than Aβ fibres, which are involved in motor function. Numerous comparative studies between ropivacaine and bupivacaine suggested that ropivacaine produces less cardiac as well as central nervous system toxic effects, less motor block and a similar duration of action of sensory analgesia as bupivacaine [9,10].
Materials and Methods
The present study was carried out in Department of Anaesthesiology and Critical Care Of a tertiary care hospital, Era’s Lucknow Medical College and Hospital, Lucknow from January 2012 to June 2013. Total duration was 18 month. All the subjects undergoing surgery for upper extremity using brachial plexus block and fulfilling the following inclusion criteria were included as study subjects.
Inclusion Criteria
Adult patients aged between 18-55 y,
ASA grade1 and 2 physical status,
Scheduled for elective surgery under brachial plexus block,
No history of allergy or sensitivity to any of the studied local anaesthetics.
Exclusion criteria
Patients with significant cardiovascular disease, Hypertension, renal failure, hepatic dysfunction, Diabetes and chronic pulmonary disease.
Neuromuscular disorder,
Morbid obesity,
Bleeding disorders,
Infection at the local site,
Any patient on prolonged drug therapy,
Uncooperative patients.
The patients were randomly divided into two groups using computerized randomization table.
Group I (n=25): Patients proposed to undergo upper limb surgery under brachial plexus block using 30 ml of 0.5% bupivacaine.
Group II (n=25): Patients proposed to undergo upper limb surgery under brachial plexus block using 30 ml of 0.5% ropivacaine.
Informed consent was obtained from all the patients enrolled in the study. All the patients were asked to remain nil orally 6-8 h prior to surgery.
On the day of surgery patients were admitted to the monitored preoperative holding area and were premedicated with 2 mg of Midazolam intravenously. The operative arm was positioned to expose the axilla. The axilla was prepared using aseptic technique and then axillary artery was identified by palpation.
The skin was anaesthetized with 1ml of 1% lidocaine solution. A 11/4 inch 22 G needle was inserted through the area of anesthetized skin into and through the axillary artery until it is noted that no blood could be aspirated through the needle. This negative aspiration indicated that needle was positioned beyond the posterior wall of the artery and in the brachial plexus sheath, 1ml of test solution was injected to rule out possible intravascular placement of the needle. All subjects were observed for possible intravascular placement of the needle for approx. 1min following the injection of test solution and then the remaining 30ml of the solution was administered in 5ml increments following aspiration. The needle was removed and firm digital pressure with gauze piece was held at the site for 5min to assist in proximal spread of the anaesthetic solution.
Sensory and motor block were evaluated preoperatively to determine a baseline and every 5 min for 30 min or until onset of blockade was noted and thereafter every 60 min
Sensory block was assessed by the pinprick method (22G hypodermic needle). Assessment of sensory block was done in the dermatomal areas corresponding to median nerve, radial nerve, ulnar nerve and musculocutaneous nerve till complete sensory blockade was achieved. Sensory onset was considered when there was a dull sensation to pinprick along the distribution of any of the above-mentioned nerves. Complete sensory block was considered when there was complete loss of sensation to pinprick [11].
Sensory block was graded as-
Grade 0: Sharp pin felt
Grade 1: Analgesia, dull sensation felt
Grade 2: Anaesthesia, no sensation felt.
A modified Bromage Scale [12] for the upper extremity was used to assess motor function. This scale consists of the following four scores:
0 - able to raise the extended arm to 90o for a full 2 sec
1 - able to flex the elbow and move the fingers but unable to raise the extended arm.
2 - unable to flex the elbow but able to move the fingers
3 - unable to move the arm, elbow or fingers
Onset of motor blockade was considered when there was Grade 1 motor blockade. Peak motor block was considered when there was Grade 3 motor blockade.
Block was considered to have failed when sensory anaesthesia was not achieved within 30 min. General anaesthesia was given subsequently to these patients who were then excluded from the study.
Haemodynamic parameters and vitals (Blood pressure, Heart rate, Respiratory rate and Oxygen saturation) were also monitored during the procedure.
Duration of analgesia was assessed by using a 10 point Visual Analogue Scale (VAS) [13] in which a score of “0” indicates “no pain” and a score of “10” “worst pain imaginable”. The VAS measurements were obtained every 60 mins till the score of 5. The rescue analgesia in the form of inj. Diclofenac sodium (1.5 mg/kg) intramuscularly was administered at the Visual Analogue Scale score of 6.
Duration of sensory block was determined by noting the time when there was return of dull sensation to pin prick and duration of motor blockade was determined by noting the time the patients could first move their fingers [10].
Side effects such as bradycardia, hypotension, headache and convulsions were looked for.
Constrain of study: Nonavailability of the nerve locator, the study was carried out with Nerve Block using the Paresthesia Technique.
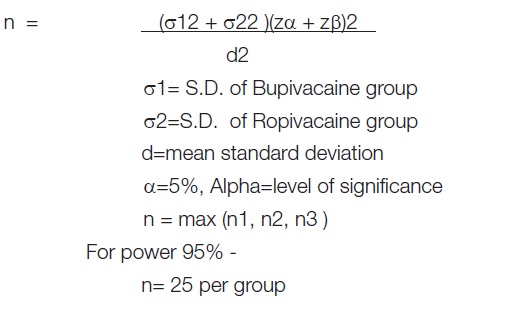
Sample size is calculated by using formula-
Results
The present study was undertaken with an aim to compare the efficacy of Bupivacaine and Ropivacaine for brachial plexus block among patients undergoing upper limb surgery. For this purpose a prospective randomized study was carried out. A total of 50 patients fulfilling the inclusion criteria as detailed in Materials and Method section of this work were enrolled in the study [Table/Fig-1].
Comparison of Demographic Variables between two groups
The two groups were matched for age, gender and body weight
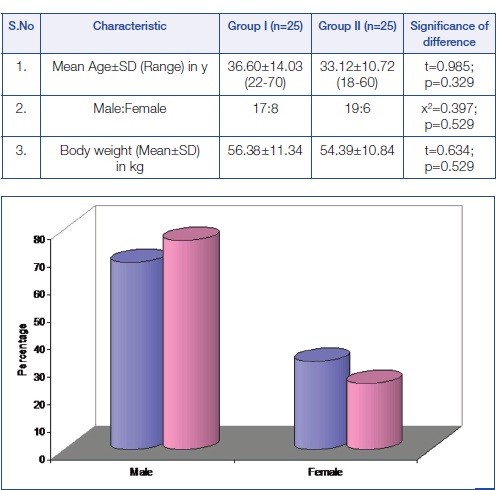
Onset of sensory blockade was started earlier in Group II (at 5 min itself) whereas in Group I it started from 10 min interval. In Group II median level of sensory blockade was 2 at 10 min as compared to 1 in Group I, thus showing a significant difference between two groups. In both the groups median level of sensory blockade remained at 2 from 15 min till 360 min interval, thus showing no significant difference in level of sensory blockade between two groups. At 420 min interval and 480 min interval, median level of sensory blockade in Group I was 2 and 1 respectively as compared to 1 and 0 respectively in Group II, thus showing a significant difference between two groups (p<0.05). At 540 min interval, in both the groups median level of sensory blockade was 0, thus showing no significant difference between two groups (p=0.077). Thus in Group II, both early achievement and early regression of sensory blockade was observed as compared to Group I [Table/Fig-2].
Comparison of Sensory Blockade at different time intervals
Mean onset time for initiation of block was significantly lower in Group II (8.88±1.74 min) as compared to Group I (12.04±2.57 min) (p<0.001). However, duration of block was significantly higher in Group I (450.40±54.50) as compared to Group II (421.20±38.33) (p=0.033) [Table/Fig-3].
Comparison of mean time for onset and duration of sensory blockade
| MRI pattern | Variable | Group I (n=25) | Group II (n=25) | Significance of difference |
|---|
| Mean | SD | Mean | SD | "t" | "p" |
|---|
| 1. | Onset time (min) | 12.04 | 2.57 | 8.88 | 1.74 | 5.086 | <0.001 (S) |
| 2. | Duration of block (min) | 450.40 | 54.50 | 421.20 | 38.33 | 2.191 | 0.033 (S) |
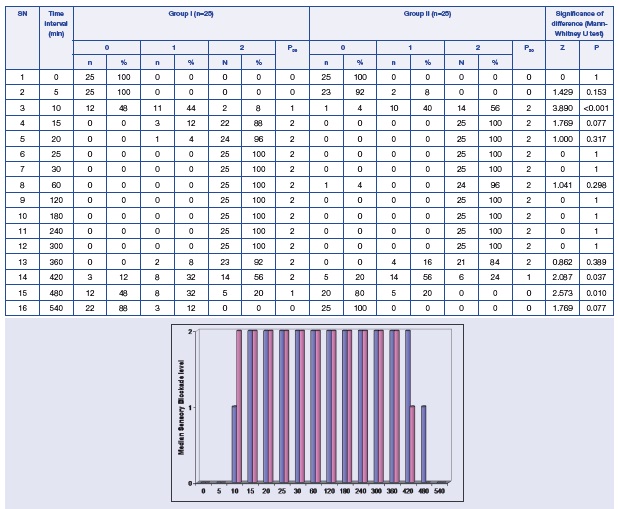
Comparision of motor blockade at different time intervals P50 = Median
Onset of motor block was observed to be initiating at 5 min interval itself in Group II whereas in Group I, onset of motor block was observed from 20 min interval onwards. In Group I, median motor blockade was 0 till 20 min interval whereas in Group II, median blockade was 2 at 10 min and 3 at subsequent time intervals. Statistically significant difference in motor blockade scores between two groups was observed from 10 min till 20 min intervals [Table/Fig-4].
In both the groups median motor blockade was observed to be 3 from 25 min interval till 300 min interval, thus showing no significant difference between two groups. Regression of motor blockade was found to be quicker in Group II as compared to Group I with median level of blockade in Group II being 2 at 360 min whereas in Group I it was 3, thus showing a significant intergroup difference (p=0.005). At 420 min interval too, there was a significant intergroup difference in level of motor blockade between two groups with Group I having median block level 2 as compared to 1 in Group II (p=0.018).
Mean onset time for initiation of block was significantly lower in Group II (14.88±3.35 min) as compared to Group I (22.92±3.79 min) (p<0.001). However, duration of block was significantly higher in Group I (408.40±50.39 min) as compared to Group II (365.60±34.29 min) (p=0.001) [Table/Fig-5].
Comparison of mean time for onset of block and duration of motor blockade
| MRI pattern | Variable | Group I (n=25) | Group II (n=25) | Significance of difference |
|---|
| Mean | SD | Mean | SD | "t" | "p" |
|---|
| 1. | Onset time (min) | 22.92 | 3.79 | 14.88 | 3.35 | 7.958 | <0.001 (S) |
| 2. | Duration of block (min) | 408.40 | 50.39 | 365.60 | 34.29 | 3.511 | 0.001 (S) |
Comparison of VAS scores at different post-operative time intervals
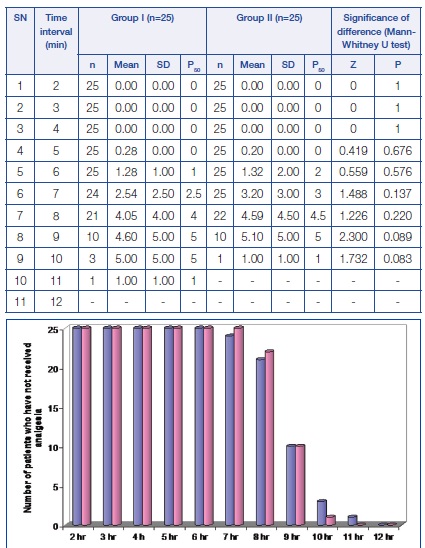
No significant difference in mean VAS scores of two groups was observed at any time interval. Need for rescue analgesia was observed to be starting from 7 h interval in Group I and from 8 h interval in Group II [Table/Fig-6,7].
Comparison of mean time for rescue analgesia (Time in hr),No significant difference in mean analgesic effect was observed between two groups (p=0.614, NS)
| SN | Time taken for | Group I (n=25) | Group II (n=25) | Significance of difference |
|---|
| Mean | SD | Mean | SD | "t" | "p" |
|---|
| 1. | Analgesic effect (hr) | 8.32 | 0.99 | 8.44 | 0.65 | -0.507 | 0.614 (NS) |
Mean heart rate was found to be higher in Group II as compared to Group I at all the time intervals yet the difference between two groups was not found to be significant statistically at any time interval (p>0.05) [Table/Fig-8].
Comparison of Heart rate in two groups at different time intervals

Mean SBP was found to be higher in Group II as compare to Group I at all time intervals except at 5 min interval, yet the difference between two groups was not found to be significant statistically at any time interval (p>0.05) [Table/Fig-9].
Comparison of SBP in two groups at different time intervals

Mean DBP in Group II was higher as compared to Group I at all the time intervals except at 5 min when both the groups had equal mean DBP. However, no significant difference was observed between two groups at any time interval (p>0.05) [Table/Fig-10].
Comparison of DBP in two groups at different time intervals

No side effects pertaining to either of the studied drugs were noted in the present study.
Discussion
Sessler et al., demonstrated that regional anaesthesia to upper extremity is a suitable alternative to general anaesthesia and confers significant benefit to patient improving safety [14,15]. It minimises the stress response, and avoids opioid-related complications.
Among various approaches to neural block of the upper extremity, axillary block is a common regional anaesthetic technique for arm, forearm and hand surgery. It is performed in a variety of orthopedic and soft tissue surgical procedures of the upper extremity [16].
Bupivacaine is frequently used as the local anaesthetic for brachial plexus anaesthesia because it offers the advantage of providing a long duration of action and a favourable ratio of sensory to motor neural block [2,3] however, its toxicity is a concerning issue especially when larger doses are used as with peripheral nerve blocks and/or prolonged infusions for postoperative analgesia.
The present study was performed to evaluate the efficacy of 0.5% Bupivacaine and 0.5% Ropivacaine in axillary brachial plexus block among patients undergoing upper limb surgeries with emphasis on comparison of onset, duration of sensory-motor block and to monitor the haemodynamic stability of two drugs. Monitoring for side effects during the procedure was also done.
Onset of motor block was observed from 5min in Ropivacaine group whereas in Bupivacaine group, onset of motor block was observed from 20 min onwards thus, showing an early onset of motor block in ropivacaine group. Klein et al., observed onset time of <6 min for both sensory and motor blockade in bupivacaine as well as ropivacaine groups among patients undergoing interscalene brachial plexus block [17]. The difference might be due to difference in approach used for the procedure.
The onset of sensory block was earlier in Ropivacaine group(5 mins) as compared to bupivacaine group(10mins), though the quality of block was superior in ropivacaine group as compared to bupivacaine group at 10 minute interval (p<0.001). These results are comparable to those obtained by Bertini et al., [1] who observed rate of complete sensory and motor block with ropivacaine group to be higher at 10, 15 and 20 min postinjection (p<0.001)1. In present study, patients in both the groups achieved peak block level by 25 min. However, mean onset time of block was found to be significantly lower in ropivacaine group (8.88±1.74 min) as compared to bupivacaine group (12.04±2.57 min).
Like motor blockade, for sensory blockade too there are variable reports dependent on selection of approach, type of surgery and patient characteristics, Mageswaran and Choy reported a mean onset time for sensory block to be 13.5±2.9 min in ropivacaine group as compared to 11.1±2.6 min in levobupivacaine group using infraclavicular approach among a mixed sample population in elective as well as emergency orthopaedic surgery patients [18] while Klein et al reported the mean onset time for both ropivacaine and bupivacaine groups to be <6 min among patients undergoing interscalene block for shoulder surgery [17]. Comparison of duration of motor and sensory blocks in present study showed the mean duration of motor and sensory blocks to be significantly longer in bupivacaine group as compared to ropivacaine group which is similar to the findings of Mc Glade et al., who found shorter duration of blockade in ropivacaine group as compared to bupivacaine group using axillary approach [9]. In present study, no difference in VAS scores between two groups was observed at any post-operative time interval. Similarly, no significant difference between two groups was observed for mean duration of analgesic effect. Thornton et al., and Mageswaran and Choy made Similar observations [10,18].
Both the groups had good hemodynamic control throughout the study duration and did not show a significant difference at any time interval. No adverse effects of the two drugs on hemodynamic has been reported at the dosages used in present study and our results are also in accordance with the findings reported.
Thus, in general, ropivacaine showed a better quality of analgesia with a shorter onset and recovery time for both sensory and motor blockade in comparision to bupivacaine.
Conclusion
On the basis of present study, conclusions were drawn that onset of action of sensory, motor block was early in Ropivacaine group with faster recovery of motor functions as compared to Bupivacaine group. No adverse effects were noted in either groups.
This study suggests that Ropivacaine is a suitable alternative to Bupivacaine for forearm surgeries under Brachial Plexus Block.