An Unusual Presentation of Neurofibroma Masquerading as a Vascular Hamartoma, Post-Iatrogenic Intervention
Abhishek Mukesh Shah1, Siba Prasad Dash2, Subhabrata P Das3, Vasundhara S Rangan4, Subhash Chandra Bhartiya5
1Post Graduate Student, Department of General Surgery, M.K.C.G. Medical College, Brahmapur, Orissa, India.
2Associate Professor, Department of General Surgery, M.K.C.G. Medical College, Brahmapur, Orissa, India.
3Assistant Professor, Department of General Surgery, M.K.C.G. Medical College, Brahmapur, Orissa, India.
4Post Graduate Student, Department of General Surgery, M.K.C.G. Medical College, Brahmapur, Orissa, India.
5Post Graduate Student, Department of General Surgery, M.K.C.G. Medical College, Brahmapur, Orissa, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Abhishek Mukesh Shah, B-8, Manju Bunglows, 3rd Cross Lane, Andheri-West, Mumbai-400053, India.
E-mail: drabhishekmshah@gmail.com
Neurofibroma is a localized discrete mass of benign nerve sheath tumour in the peripheral nervous system. Mostly present as skin lesions. Solitary neurofibroma may occur in deep soft tissue or subcutaneous plane in rare cases associated with syndromes like NF1. The neurofibroma most commonly present as skin lesions as isolated soft papules or nodules arising in any cutaneous site. Present case depicts unusual presentation of a neurofibroma as a vascular hamartoma post an iatrogenic intervention.
Iatrogenic intervention, Neurofibroma, Post traumatic, Unusual presentation, Vascular hamartoma
Case Report
A 22-year-old female presented to Maharaja Krishna Chandra Gajapati (MKCG) Medical College & Hospital, Brahmapur, Ganjam, Odisha in the May 2012, with painless lump on right shoulder for the last two years. Two years back she took intramuscular injection, following which the region was painful for about one month, after which she noticed a small swelling for which she sought medical consultation in a peripheral health care centre. There, it was suspected to be an abscess and drainage was attempted three months back. The lump persisted and gradually increased in size since then. The sensations over the skin were found to be intact.
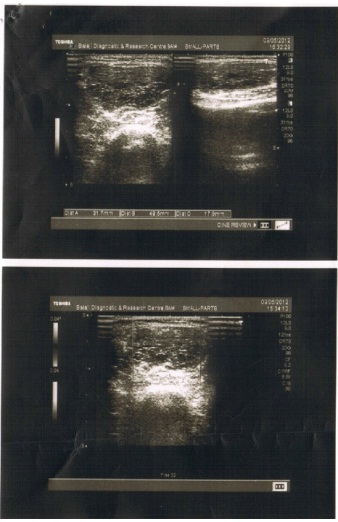
On Clinical examination, lump of 4cm x 5cm x 3cm was seen over right shoulder region, oval with smooth surface, soft, non-compressible, irreducible. [Table/Fig-1], indicating a solid swelling for which an X-ray shoulder region was advised. X-ray showed no bony involvement following which FNAC was advised.
FNAC impression was of a benign vascular hamartoma. As aspirate from the solid swelling showed altered blood, few endothelial cells and rbcs, with absence of malignant cells. Following this further ultrasonographic (USG) examination was done. Ultrasound showed heterogenous isoechoic lesion below subcutaneous layer [Table/Fig-2], with no evident flow, Differentials being- Lipoma / Hemangioma / Inflammatory.
As ultrasound Image showed a heterogenous isoechoic lesion in subcutaneous plane [Table/Fig-2], So decision to do an excisional biopsy of the mass was undertaken under general anaesthesia. In Bhartiya5the post-operative period, patient received 1 dose of intravenous diclofenac by infusion, and was started on oral liquids 6 hours postoperatively. Intraoperatively, solid swelling surrounded with small, non-capsulated cysts, filled with blood, were situated in the subcutaneous plane.
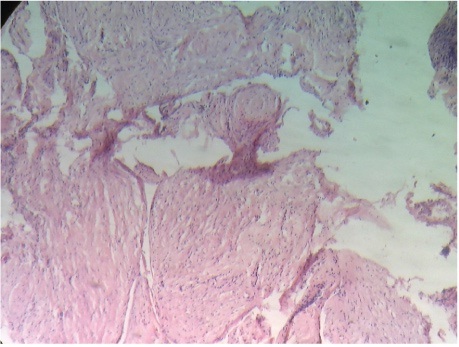
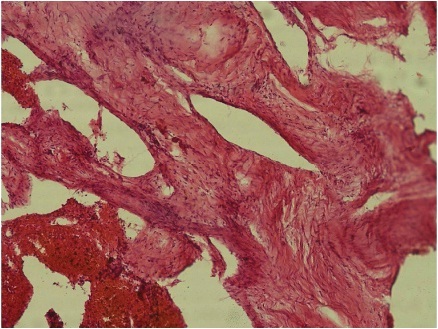
A section was done and examined with hematoxylin and eosin stain (H&E stain or HE stain) staining technique in which microsections showed organoid structures comprising of spindle shaped cells in a collagenous background without nuclear atypia which was consistent with neurofibroma [Table/Fig-3,4].
Patient was discharged the following morning. The stitched were removed seven days postoperatively. Follow up of the patient was uneventful for period of a month. The excisional biopsy, post histopathology reporting, was confirmed as therapeutic too.
Discussion
Injection nerve palsy (INP) is injury to the peripheral nerves from accidental injection of drugs and appears to be a common problem in developing countries because of indiscriminate use of intramascular injection (IMI) for treating common illnesses [1]. It is caused either by injection close to the nerve or by accumulation of the injected drug within the spaces where the nerves travels e.g. in case of Sciatic Nerve it is formed between the piriformis, gemellus, quadratus and obturator muscles. Other possible mechanisms are direct needle trauma, secondary compression by scar tissue and direct nerve fibre damage caused by neurotoxic chemicals in the injected drug [2]. This is the case of neurofibroma that appeared as painless lump following an intramuscular injection.
In this case, the neurofibroma, initially presenting with pain, may have been misdiagnosed as inflammatory or infective pathology due to the antecedent history of intramuscular injection which made the patient aware of it. The patient presented to our institution with a mass over shoulder. The USG findings and FNAC picture pivoted the diagnosis towards a vascular hamartoma. M Tsutsumi et al., too reported a similar case where spontaneous haemorrhage in scalp neurofibroma caused it to present as hypervascular rapidly expanding tumour [3].
Similarly D’Orazi reported the case of a patient who had severe foot pain, which progressively hampered her walking ability, erroneously attributed to recurrent Morton's neuroma. Diagnosis of plexiform neurofibroma of her right medial plantar nerve was made 15 y after the appearance of symptoms. Pain and function recovered after radical neurotomy of the medial plantar nerve [4]. Fariba et al., presented a case of laryngeal myxoid neurofibroma, which at first was misdiagnosed as myxoma in a 65-year-old Iranian male. The patient recovered after excisional biopsy where complete resection of tumour was perfomed [5].
Neurofibromas arise from the sheath of nerve fibers and are characterized by prominent collagen production and trapped nerve fibers [5]. Microscopic appearance of neurofibroma consists of scattered spindle shaped cells with buckled or S-shaped nuclei with a variable myxoid background. Scattered small vessels and mast cells are common [6,7]. The scattered blood vessels are the characteristic which differentiate it from other conditions with similar presentation (e.g., melanotic nevus/neurotised nevus). The vasculo-cystic component of neurofibroma in present case may be attributed to incision and failed drainage attempted three months before presenting to our institute causing haemorrhage in the swelling and its sudden increase in size post the attempt (incision scar seen in [Table/Fig-1]).
Pondering whether the trauma was an antecedent cause and the aetiology for the development of the neurofibroma would be ill founded as patient clearly had another neurofibroma in the flank too. The case was seen as traumatic neuroma in the differentials with the history but the histopathology confirmed it to be neurofibroma. Apart from this, traumatic neuromas are capsulated and pretty distinct from plain neurofibroma as in the present case. Da Rosa et al., too reported a rare case of solitary giant neurofibroma of a mental nerve whose aetiology was related to a local trauma [8]. Carpenter and Stickney too reported a case of 38-year-old female presented with extreme pain over her anterior leg secondary to a traumatic event [9]. TW Chi et al., reported a neurofibroma discovered incidentally in a woman who suffered trauma to her cheek. The lesion manifested on CT as a haematoma within a parotid tumour [10].

Ultrasound Image-heterogenous isoechoic lesion in subcutaneous plane,
Microscopic picture showing spindle cells in collagenous background(100x)
Microscopic picture showing dilated vascular elements with thrombi next to hypocellular area (400x)
Conclusion
The patient presented with mass following an intramuscular injection (may be the aetiological factor but few cases with post traumatic neurofibroma with circumstantial proof have been reported). The interesting component of the case being its presentation as vascular hamartoma in FNAC report as well as correlated by the Ultrasound study of the area but lack of clear clinical correlation as irreducible, non-compressible unlike in vascular swelling. The vascular cystic component may be iatrogenic in nature due to incision and drainage attempted three months before presenting to our centre.
[1]. A Kakati, D Bhat, BI Devi, D Shukla, Injection nerve palsyJ Neurosci Rural Pract 2013 4(1):13-18. [Google Scholar]
[2]. FJ Villarejo, AM Pascual, Injection injury of the sciatic nerve (370 cases)Childs Nerv Syst 1993 9:229-32. [Google Scholar]
[3]. M Tsutsumi, K Kazekawa, A Tanaka, Y Ueno, Y Nomoto, K Nii, Rapid expansion of benign scalp neurofibroma caused by massive intratumoural hemorrhage--case reportNeurol Med Chir 2002 42:338-40. [Google Scholar]
[4]. V D’Orazi, T Venditto, A Panunzi, S Anichini, GM Gi, A Tallarico, Misdiagnosis of plexiform neurofibroma of the medial plantar nerve: Case reportThe Foot 2014 24(3):143-45. [Google Scholar]
[5]. B Fariba, DM Hossein, R Yavar, S Haneyeh, Laryngeal myxoid neurofibroma misdiagnosed as myxoma: a case reportThe Chinese-German Journal of Clinical Oncology 2012 11(9):548-50. [Google Scholar]
[6]. SI Harkin, RJ Reed, Atlas of Tumour Pathology, series 2, fascicle 3 Tumours of the Peripheral Nervous System. Washington, DCArmed Forces Institute of Pathology 1969 [Google Scholar]
[7]. IM Ariel, Tumours of the Peripheral Nervous SystemCa-A Cancer J Clin 1983 33(5):282-99. [Google Scholar]
[8]. MR Da Rosa, AL Ribeiro, SA De Menezes, JJ Pinheiro, SM Alves-Junior, Solitary giant neurofibroma of the mental nerve: a trauma-related lesion?J Craniofac Surg 2013 24(3):e247-51. [Google Scholar]
[9]. B Carpenter, N Stickney, Neurofibroma of the Anterior Leg: A Case ReportThe Foot and Ankle Online Journal 2012 5(6):2 [Google Scholar]
[10]. TW Chi, JC Lin, SL Shih, Neurofibroma: an unusual presentationNeuroradiology 1993 35(8):614-15. [Google Scholar]