Intracranial Fungal Granulomas Mimicking High Grade Gliomas. A Decisive Role of Squash Cytology (SC): A Report of Two Cases
Parth A. Desai1, Ronak K. Patel2, Nita Khurana3, P.N. Pandey4
1 Post Graduate Resident, Department of Pathology, Maulana Azad Medical College, New Delhi, India.
2 Senior Resident, Department of Radiodiagnosis, Maulana Azad Medical College, New Delhi, India.
3 Professor, Department of Pathology, Maulana Azad Medical College, New Delhi, India.
4 Consultant, Department of Neurosurgery, Maulana Azad Medical College, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Parth A Desai, A/9, Mehali Apartments, Near Gokulam Dairy, Athwalines, Surat, Gujarat-395001, India.
E-mail: Parth1410@gmail.com
Intracranial fungal granulomas can be misdiagnosed clinically and radiologically as neoplastic lesions. They also rarely occur without any history of immunodeficiency or diabetes. We report two such cases of fungal granulomas that were unsuspected clinically and radiologically but were detected on intraoperative squash cytology (SC) and later confirmed on histopathology. Timely intervention was hence possible and patient was saved from the hazards of unnecessary removal of eloquent areas of brain and was shifted on proper medical management. SC remains an indispensible tool for the neurosurgeon to get a provisional intraoperative diagnosis and in such surprising scenarios, change the surgical management of the patient, save the resection of eloquent brain areas and begin immediate postoperative medical management. These cases are being presented for their rarity and for highlighting the importance of SC as a regular tool for intraoperative neurosurgical consultation of intracranial mass lesions.
Fungal mass lesions, Granuloma, Intraoperative cytology, Neurosurgery, Squash cytology
Case Report
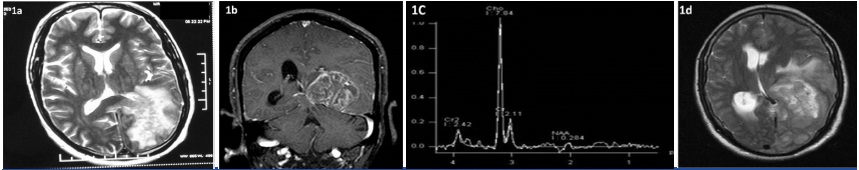
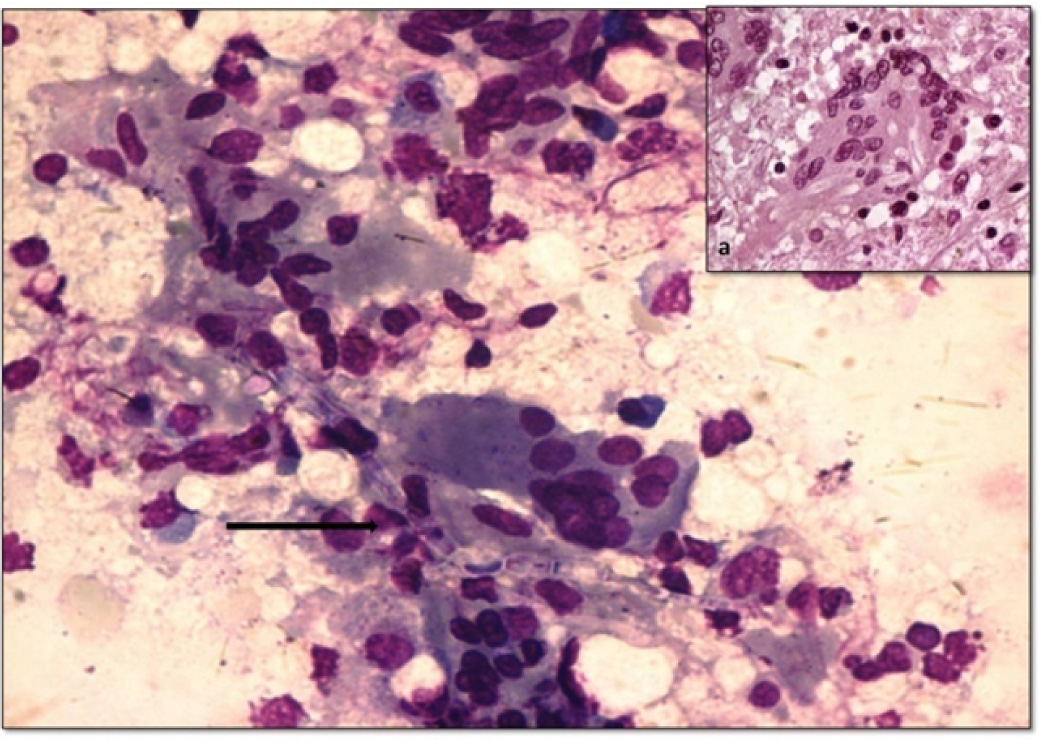
Case 1 was a 40-year-old male with history of sudden loss of consciousness. There was no history of fever or headache or focal neurological deficit. Magnetic resonance imaging (MRI) revealed a heterogeneously hyperintense mass on T2 weighted image [Table/Fig-1a&1b] and on postcontrast T1 weighted image a heterogeneously enhancing mass lesion showing necrosis and extensive perilesional edema in left parieto-occipital region suggestive of high grade glioma [Table/Fig-1c]. Magnetic resonance spectroscopy (MRS) also revealed high Choline peak (3.2 ppm) characteristic of high grade gliomas [Table/Fig-1d]. Informed consent was taken from the patient for intraoperative cytology consultation preoperatively. Intraoperative squash smears from the lesional area revealed many plasma cells, epithelioid cells, giant cells and many long, narrow, septate branching fungal bodies suggestive of Aspergilloma [Table/Fig-2]. The resection was halted after adequate surgical decompression and patient was immediately started on antifungal therapy. The patient responded quickly to the treatment. Histopathology was also consistent with Aspergillus granuloma and showed no evidence of a neoplastic lesion. Samples sent for microbiological culture confirmed Aspergillus fumigates as the infecting fungal species. An active search for primary foci was done but none was found in paranasal sinuses, ear canal or lungs. The patient was not diabetic, with normal hemogram findings and was negative for human immunodeficiency virus (HIV) infection.
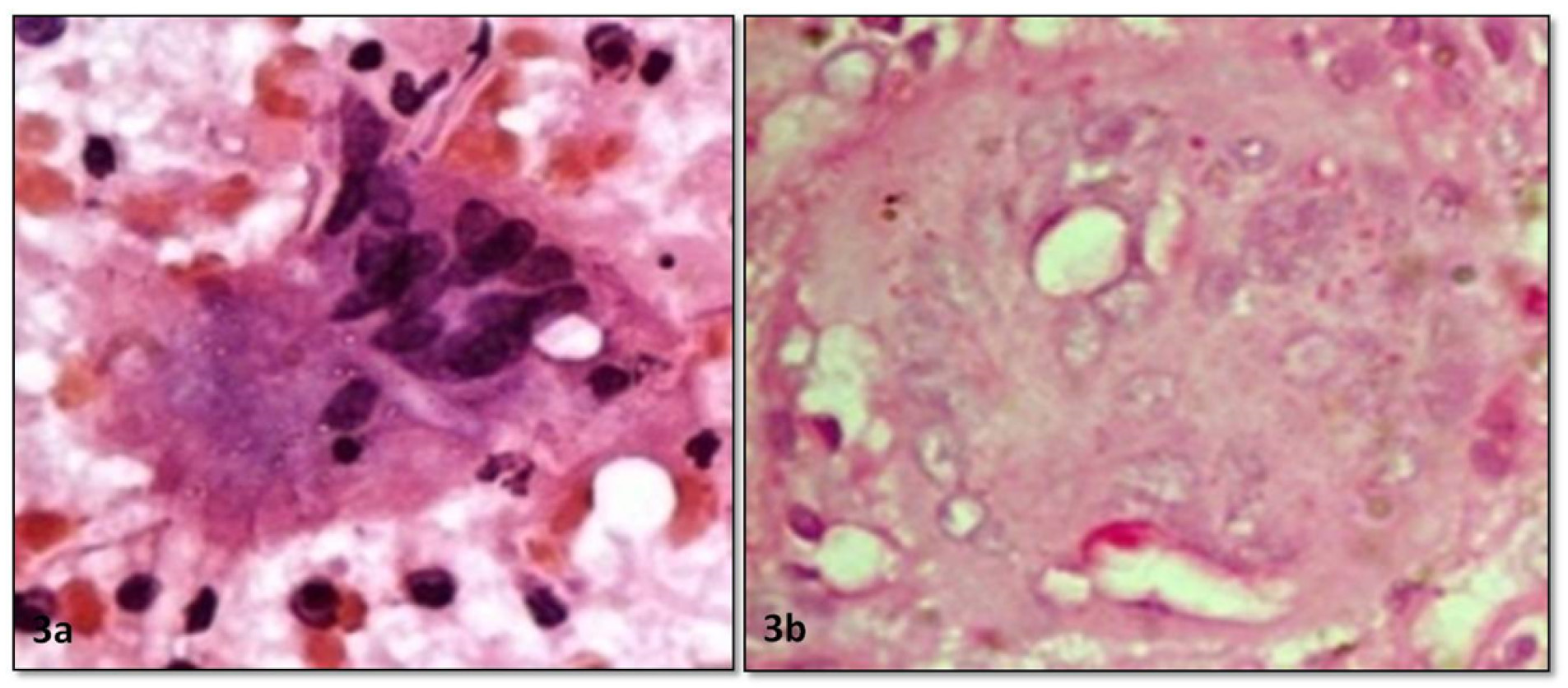
Case 2 was a 25-year-old male who presented with a short term history of headache, low grade fever, sudden episodes of unconsciousness and two episodes of seizures since last two months. MRI revealed a necrotic mass in right parietal region showing heterogeneous postcontrast enhancement, suggestive of high grade glioma. MRS findings showed no specific peak. CSF examination was normal. Hence, the patient was operated and sample was sent for cytological consultation. Informed consent was taken preoperatively from the patient for intraoperative cytology consultation. The smears revealed glial tissue with minimal pleomorphism, no overcrowding and many plasma cells and few histiocytes. Few broad aseptate fungi were seen, suggestive of Zygomycetes infection [Table/Fig-3a]. The patient was immediately shifted on antifungal treatment histopathology revealed a granulomatous lesion surrounded by gliotic tissue and many broad aseptate hyphae which were characteristic of Zygomycosis and confirmed using periodic acid stain (PAS) stain [Table/Fig-3b]. Interestingly, again no foci of entry of the fungal infection or any history of diabetes mellitus or immunocompromised state could be established. Culture studies confirmed Rhizopus species.
1a) T2 weighted axial MR image of brain shows heterogenouly hyperintense mass lesion in left parieto-occipital region with extensive perilesional edema
1b) T1 weighted post contrast Coronal MRI showing heterogeneous enhancement with central necrosis and perilesional edema;
1c) Single voxel MR spectroscopy from the solid part of the lesion reveals elevated choline level (3.2 ppm), with markedly reduced NAA and creatinine level
1d) T2 weighted axial MRI image showing large mass lesion is noted in left parieto-occipital region, showing heterogeneous T2 hyper intensity
SC from case 1 showing plasma cells & giant cells with ingested septate fungal hyphae diagnostic of Aspergilloma (arrow) (400x,Giemsa), Inset-(a) HPE from case 1 showing a giant cell with ingested fungal hyphae (400x,HE).
(a) SC from case 2 showing many broad aseptate fungal hyphae in a giant cell consistent with Zygomycosis (400x,PAP stain); (b) HPE from case 2 showing PAS+ broad hyphae of Zygomycosis in a giant cell (400x,HE).
Discussion
CNS fungal infections are not seen commonly in general population but commonly seen in immunocompromised hosts or patients with uncontrolled diabetes mellitus [1]. They can present as meningitis or as mass lesions [1,2]. Candidiasis is the most common CNS fungal infection presenting mostly as acute meningitis and occasionally as mass lesion [1]. Cryptococcus neoformans is an important cause of chronic lymphocytic meningitis especially in immunocompromised patients. Common fungus causing mass lesions as granulomas or abscess are Aspergillus, Zygomycetes (Rhizopus, Absidia, mucor), Candida, Blastomyces dermatidis and Coccidioides immitis [1,3,4]. The inflammatory reaction in these cases is minimal especially with granulomas, possibly causing confusing MRI and MRS findings [5]. Fungal granulomas are not a very common cause of space occupying lesions in immunocompetent patients or without history of diabetes mellitus [6]. Mortality of intracranial fungal granulomas is high nearly reaching 63% [1,4]. Both these cases were suspected to be neoplastic lesions on MRI. Even the MRS findings were either in favor of a neoplastic lesion (Case 1) or nonspecific (Case 2), implying that a preoperative diagnosis of fungal infection in these cases was almost impossible. Choline peak has found to be raised in certain intracranial Aspergillomas in the past [5]. Hence, SC was of extreme utility in these cases for the neurosurgeon in limiting the extent of resection, preserving the sample for microbial culture, begin immediate empirical antifungal therapy as well as to search for the source of infection. The squash features that helped in diagnosis were rich plasma cell infiltrate along with lymphocytes, minimal reactive changes in the background glial tissue with few gemistocytes and no overcrowding or atypia in both the cases, presence of giant cells, ill-defined granulomas and negative fungal shadows. Although on low power, SC in both cases showed hyper-cellular tissue clumps but the majority of the cellularity was composed of the inflammatory infiltrate and on close inspection the background glial cells were normal appearing and there were reactive gemistocytes and astrocytes with fine processes radiating on all sides highly indicative of reactive glial tissue. Plasma cell rich infiltrate in absence of eosinophils in case of CNS fungal granulomas has been described previously in similar cases reported by Jaiswal et al., [7]. SC has been an extremely useful tool for intraoperative neurosurgical consultation due to the problems with frozen sections in neuropathology [8]. These cases do highlight the extreme utility of intraoperative SC in avoiding significant patient morbidity and unnecessary removal of eloquent areas of brain which could be saved if correct diagnosis is achieved at the right time.
Conclusion
Hence, intracranial fungal mass lesions can occur in immunocompetent hosts rarely and without any known primary focus. They can radiologically mimic CNS tumours. Hence, intraoperative SC will help as a check point in these cases for redirecting the management in such surprising cases and help in reducing significant morbidity and mortality as seen in these two cases.
[1]. Chakrabarti A, Epidemiology of central nervous system mycosesNeurol India 2007 55(3):191-97. [Google Scholar]
[2]. Dubey A, Patwardhan RV, Sampth S, Santosh V, Kolluri S, Nanda A, Intracranial fungal granuloma: analysis of 40 patients and review of the literatureSurg Neurol 2005 63(3):254-60. [Google Scholar]
[3]. Azarpira N, Esfandiari M, Bagheri MH, Rakei S, Salari S, Cerebral aspergillosis presenting as a mass lesionBraz J Infect Dis 2008 12(4):349-51. [Google Scholar]
[4]. Cunliffe CH, Fischer I, Monoky D, Intracranial lesions mimicking neoplasmsArch Pathol Lab Med 2009 133:101-23. [Google Scholar]
[5]. Jain KK, Mittal SK, Kumar S, Gupta RK, Imaging features of central nervous system fungal infectionsNeurol India 2007 55(3):241-50. [Google Scholar]
[6]. Tintelnot K, de Hoog GS, Haase G, Fungal infections of the central nervous system in the immunocompetent hostPathologe 2013 34(6):534-39. [Google Scholar]
[7]. Jaiswal S, Vij M, Jaiswal AK, Behari S, Intraoperative Squash cytology of Central Nervous system lesions: A single Center study of 326 casesDiagn Cytopathol 2010 13:234-39. [Google Scholar]
[8]. Roessler K, Dietrich W, Kitz K, High Diagnostic Accuracy of Cytologic smears of Central Nervous System Tumours, A 15 year experience based on 4172 patientsActa Cytol 2002 46:664-69. [Google Scholar]