A New Variant of Choledochal Cyst Diagnosed on Magnetic Resonance Cholangiopancreatography
Shailesh Gupta1, S. Rajesh2, Nitesh Agrawal3, Somsharan S. Betgeri4, Ankur Arora5
1 Senior Resident, Department of Radiology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi, India.
2 Assistant Professor, Department of Radiology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi, India.
3 Senior Resident, Department of Radiology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi, India.
4 Senior Resident, Department of Radiology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi, India.
5 Associate Professor, Department of Radiology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. S. Rajesh, Assistant Professor, Department of Radiology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi-11070, India.
E-mail: rajesh387@gmail.com
Choledochal cysts (CDC) have been traditionally classified into five types and subtypes based on the pattern and location of involvement of intra and extra hepatic biliary tree. Herein, we describe a new variant of choledochal cyst which has not been previously described in the English-language medical literature.
Biliary tree, Choledochal cyst, Cystic duct, MRCP
Case Report
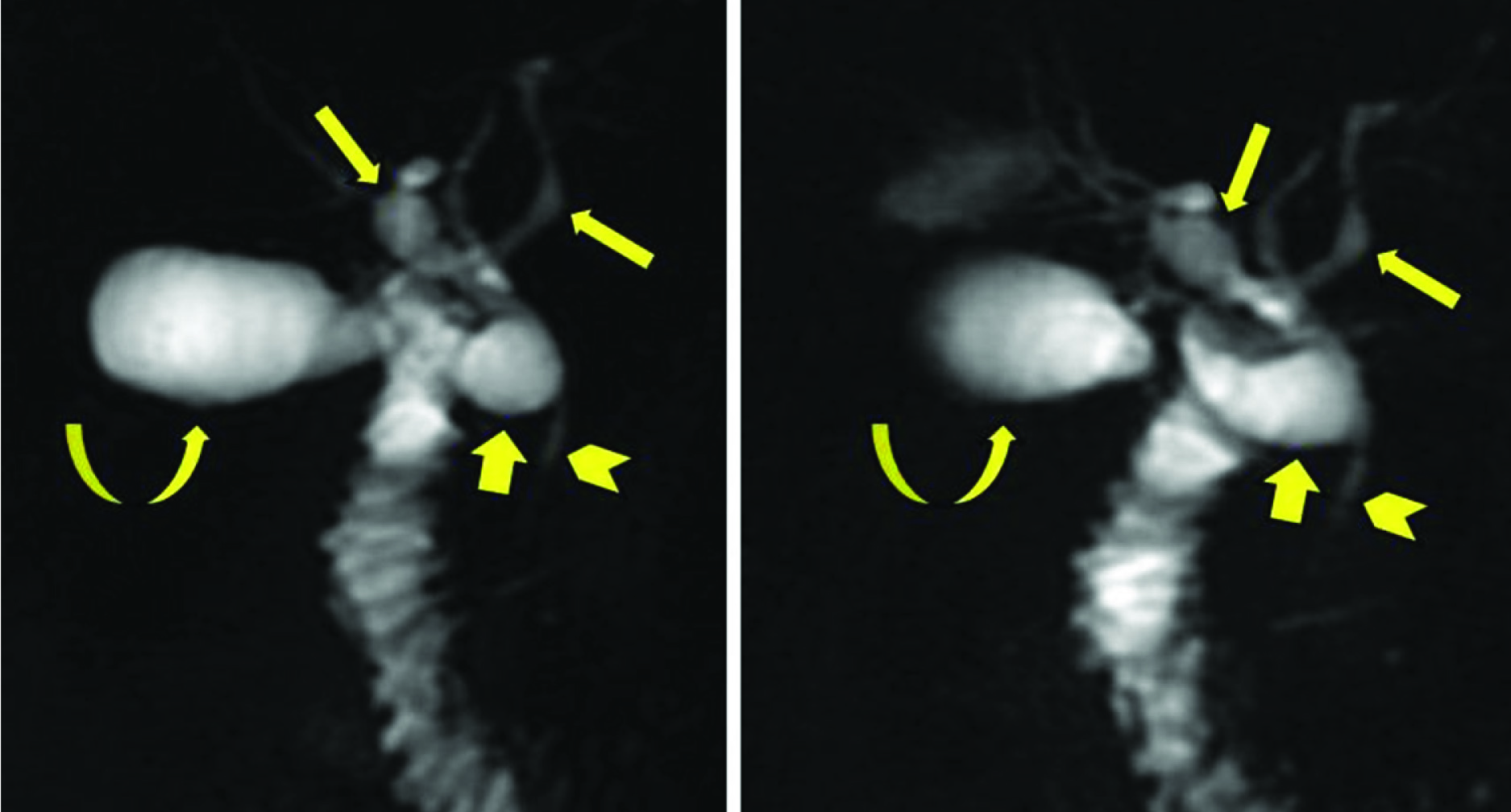
A 15-year-old male presented to the hepatology out-patient department with complaints of intermittent crampy upper abdominal pain for a month which got aggravated after meals. The pain was not associated with nausea, vomiting, and abdominal distension or altered bowel movements. There was no past history of fever or jaundice. Physical examination did not reveal any significant abnormality. Laboratory investigations including liver function tests were within normal limits. Ultrasound examination performed at an institution elsewhere had shown mildly thickened gall bladder walls with mild central bilobar intrahepatic biliary radical dilatation. In view of biliary dilatation, patient underwent magnetic resonance cholangiopancreatography (MRCP) which revealed that there was focal segmental fusiform dilatation of both right and left hepatic ducts just proximal to the primary biliary confluence. In addition, the cystic duct was also focally dilated [Table/Fig-1]. The common bile duct (CBD) was normal in caliber. There was no associated anomalous pancreatico-biliary junction. No evidence of any obstructive intraductal calculus or stricture was noted in any part of biliary tree. The patient was advised surgical management but was lost to follow-up.
Thick-section (40-mm) MRCP images demonstrates the fusiform dilatation of Intrahepatic bile ducts (thin arrows) and cystic duct (thick arrows). Note normal caliber of common bile duct (arrow head). Curved arrow denotes gall bladder
Discussion
Choledochal cysts are an uncommon anomaly and are thought to be a result of abnormal long common channel between the distal CBD and pancreatic duct which can lead to reflux of pancreatic enzymes into the biliary tree causing weakness in ductal walls and abnormal dilatation [1]. Another proposed theory is malfunctioning sphincter of oddi causing upstream reflux of pancreatic juices with resultant biliary dilatation [2]. Both extra and intrahepatic ducts can be involved. Based on the location of involvement, Todani et al., [3] have classified CDC into five types: Type 1 is the most common type and is further divided into three subtypes on the basis of morphology of dilated CBD – 1A(cystic dilatation), 1B(segmental dilatation) and type 1C corresponds to fusiform dilatation of common bile duct, type 2 represents diverticulum of CBD, while type 3 is focal cystic dilatation of terminal CBD known as choledochocele; type 4 has been further subdivided into type 4a which is saccular dilatation of both intra and extra hepatic bile ducts and type 4b where there is saccular dilatation of only extra hepatic bile duct, type 5 is cystic dilatation of only intrahepatic bile ducts and popularly known as Caroli’s disease. This classification does not take into account the involvement of cystic duct. The tremendous advancements in imaging technology have resulted in incidental detection of a number of new variants most of which include involvement of cystic duct. However, all the previous literature is either on isolated cystic duct involvement or the involvement of cystic duct along with extra hepatic duct involvement [4–7]. The present case was unique as there was involvement of cystic duct along with bilobar central intra hepatic bile ducts [Table/Fig-2].
Schematic diagram depicting different types of choledochal cysts as proposed by Todani et al., [3] and the present case. Yellow colour- biliary tree, green- gall bladder and cystic duct, orange- duodenum, light pink- pancreas

Preoperative diagnosis is very important as choledochal cysts with only extrahepatic duct involvement are managed by complete excision of cyst with hepaticoenterostomy and cholecystectomy, while if there is intrahepatic involvement then partial hepatectomy or liver transplantation may be needed according to the extent of disease [8,9]. As the use of laparoscopic management of CDC is increasing [10], preoperative diagnosis of such variants helps in deciding the surgical approach and to avoid complications of duct injury.
Conclusion
In conclusion, with the recent surge in the volume of literature describing new variants of CDC, especially including cystic ducts, we propose the inclusion of cystic duct variants in the classification and that a suffix “c” can be added after the parent subtype if cystic duct is also involved. Hence, our case can be considered as a variant of Todani’s type 4A with extrahepatic duct involvement in form of cystic duct dilatation. Hence it can be classified as type 4A’c’ or 4c, while an isolated cystic duct can be considered as type 6.
[1]. Babbitt DP, Starshak RJ, Clemett AR, Choledochal cyst: a concept of etiologyAm J Roentgenol Radium Ther Nucl Med 1973 119(1):57-62. [Google Scholar]
[2]. Imazu M, Iwai N, Tokiwa K, Shimotake T, Kimura O, Ono S, Factors of biliary carcinogenesis in choledochal cystsEur J Pediatr Surg 2001 11(1):24-27. [Google Scholar]
[3]. Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K, Congenital bile duct cysts: Classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cystAm J Surg 1977 134(2):263-69. [Google Scholar]
[4]. Yoon JH, Magnetic resonance cholangiopancreatography diagnosis of choledochal cyst involving the cystic duct: report of three casesBr J Radiol 2011 84(997):e18-22. [Google Scholar]
[5]. Michaelides M, Dimarelos V, Kostantinou D, Bintoudi A, Tzikos F, Kyriakou V, A new variant of Todani type I choledochal cyst. Imaging evaluationHippokratia 2011 15(2):174-77. [Google Scholar]
[6]. Serena Serradel AF, Santamaría Linares E, Herrera Goepfert R, Cystic dilatation of the cystic duct: a new type of biliary cystSurgery 1991 109(3 Pt 1):320-22. [Google Scholar]
[7]. Maheshwari P, Cystic malformation of cystic duct: 10 cases and review of literatureWorld J Radiol 2012 4(9):413-17. [Google Scholar]
[8]. Metcalfe MS, Wemyss-Holden SA, Maddern GJ, Management dilemmas with choledochal cystsArch Surg 2003 138(3):333-39. [Google Scholar]
[9]. Ulas M, Polat E, Karaman K, Dalgic T, Ercan M, Ozer I, Management of choledochal cysts in adults: a retrospective analysis of 23 patientsHepatogastroenterology 2012 59(116):1155-59. [Google Scholar]
[10]. Jang JY, Kim SW, Han HS, Yoon YS, Han SS, Park YH, Totally laparoscopic management of choledochal cysts using a four-hole methodSurg Endosc 2006 20(11):1762-65. [Google Scholar]