Benign Paravertebral Ancient Neurilemmoma in a Young Adult: A Rare Occurrence
Narayanaswamy Chetty Y.V.1, Pankaja S.S2, S.V. Kulkarni3, Sridhar M.4, Ranganatha M.5
1Associate Professor, Department of General Surgery, M S Ramaiah Medical Teaching Hospital, Bengaluru , Karnataka, India.
2Assistant Professor, Department of General Surgery, M S Ramaiah Medical Teaching Hospital, Bengaluru , Karnataka, India.
3Professor, Department of General Surgery, M S Ramaiah Medical Teaching Hospital, Bengaluru , Karnataka, India.
4Associate Professor, Department of General Surgery, M S Ramaiah Medical Teaching Hospital, Bengaluru , Karnataka, India.
5Post Graduate Student, Department of General Surgery, M S Ramaiah Medical Teaching Hospital, Bengaluru , Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Narayanaswamy Chetty Y.V., Associate Professor, Department of General Surgery, M.S. Ramaiah Medical Teaching Hospital, Mathikere, Bengaluru-560054, India.
E-mail: drswamy20@gmail.com
Neurilemmoma is a benign neurogenic tumour arising from Schwann cells of the peripheral nerve sheath, which is commonly seen in women in the 5th decade. It rarely arises in the retroperitoneum, being more common in the head and neck region and extremities. Ancient variety of schwannoma is a long-standing tumour, is seen in the middle age and elderly age groups, and is associated with secondary degenerative changes. Herein, we report a case of benign retroperitoneal paravertebral ancient neurilemmoma occurring in a young male adult.
Ancient schwannomma, Retroperitoneal swelling, Retroperitoneal schwannoma, Retroperitoneal tumours, Schwannoma
Case Report
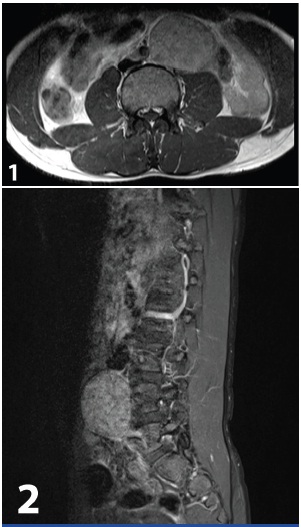
A young adult male 21-year-old presented to our out patient department (OPD) with history of periumbilical pain of 6 months duration with no other associated symptoms. Examination revealed a vague, hard, globular, retroperitoneal mass, of 5x4 cm, in the left para-umbilical region extending into lumbar region, with lateral and superior borders palpable only on deep palpation. Ultrasonography of the abdomen showed an encapsulated well-circumscribed solid mass, measuring 6x4 cm, in the left para-aortic area, with homogenous density and two tiny areas of necrosis, suggestive of paragangliomaora lymph nodal mass. CECT abdomen reported a large,well-defined, lobulated soft tissue mass lesion measuring approximately 6.2x4.8x7.3 cm in the left para-aortic aspect of retroperitoneum at the level aortic bifurcation with extension along the left common iliac artery. It showed mild heterogeneous enhancement within the mass on contrast study with mild peripheral vascularity. The mass was closely abutting the abdominal aorta with infero-medial displacement of the left common iliac artery and lateral displacement of the mid portion of the left ureter. CT guided FNAC of the mass revealed spindle cell tumour of nerve sheath origin probably of benign nature. MRI Lumbo-Sacral spine [Table/Fig-1,2] reported a large T1 hypo intense and T2 heterogeneously hyper intense, well-encapsulated retroperitoneal mass at the level of L4 vertebra representing nerve sheath tumour.
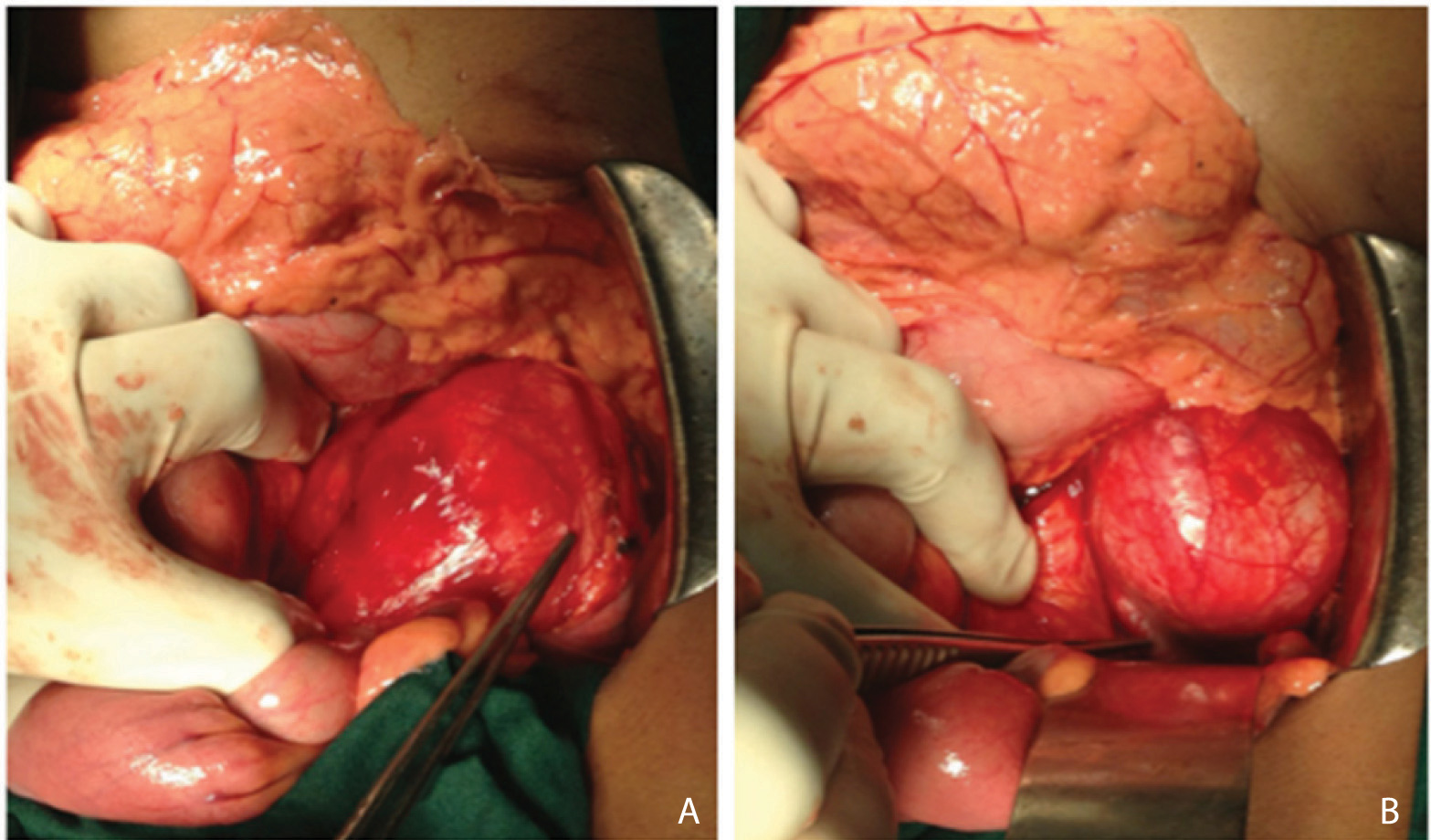
Following these investigative findings, an exploratory laparotomy was performed with midline approach. A mass was noted in the left paracolic gutter covered by the sigmoid mesocolon. Peritoneal reflection from the lateral paracolic gutter along with sigmoid mesocolon was reflected medially off the mass, preserving the inferior mesenteric vessels. The mass measuring 7x 8 cm, was found stretching and displacing the left ureter and gonadal vessels on its lateral aspect [Table/Fig-3a] and was closely abutting the lower 5cm of the aorta and displacing the left common iliac vessels inferiorly [Table/Fig-3b]. The above structures were densely adherent to the capsule of this mass. These structures were meticulously dissected and preserved. One lumbar spinal nerve was found entering the mass postero-superiorly, which was divided. The entire mass was excised with the capsule intact and sent for histopathological examination.
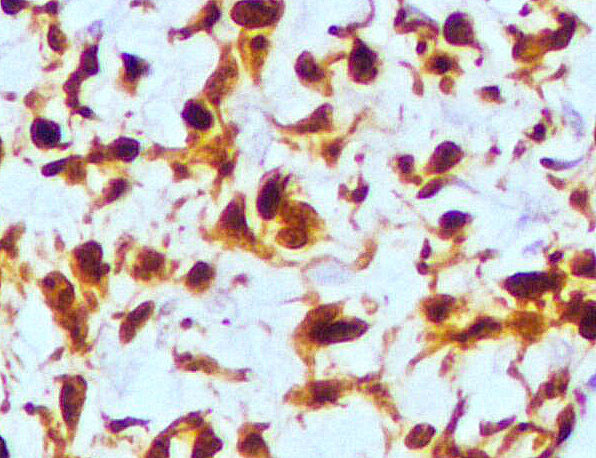
Gross examination revealed a well-circumscribed tumour with solid and cystic areas and calcific foci. Histopathologic examination [Table/Fig-4] reported a benign neurilemmoma of ancient variety with typical high cellularity Antoni A regions, low cellularity Antoni B regions along with areas of hyalinization and blood vessels showing degenerative changes. Diagnosis was confirmed with immunohistochemistry, which revealed neoplastic cells, which were diffusely positive for S-100 protein (Biogenex Clone -1E2E2) [Table/Fig-5]. Postoperative period was uneventful and patient was discharged after 10 days. Patient was followed up on regular basis clinically and with ultrasonography of the abdomen at 6 months and at one-year post surgery. A year after surgery, the patient is asymptomatic and doing well.
Discussion
Schwannomas or neurilemmomas or neurinomas are benign, slow growing, solitary and well-encapsulated lesions that arise from the Schwann cells [1].The common sites include the head and neck, the flexor surfaces ofthe upper and lower extremities, the posterior mediastinum in the thorax and on the trunk. Cases involving the retroperitoneum, small bowel, extrahepatic biliary tree, pancreas, pelvis and sacrum have been reported as rare sites of occurrence [2]. Retroperitoneal schwannomas are rare tumours, with incidence of 0.7% to 2.6% of all schwannomas [3] and they are the cause of 0.5 to 12% of retroperitoneal masses [4]. In a large study of 82 cases of retroperitoneal and pelvic scwannomas, it was found that the left lower lumbar schwannomas are the least common, accounting to only 13.4% of such cases [5]. In the retroperitoneal position, they occur most commonly between 40 and 60 years of age, with a male/female ratio of 2:3. Most schwannomas are benign, although malignant cases are rarely known to occur, especially when there is association with Von Recklinghausen’s disease, which occurs in 5% to 18% of cases [6]. These tumours usually attain a large size of 10 – 20cm in diameter by the time of surgery since they are usually asymptomatic or give rise to nonspecific symptoms such as vague abdominal or back pain or discomfort [3]. Surprisingly, our patient was a young male who was found to have an uncommon variant i.e. ancient retroperitoneal neurilemmoma or schwannoma of medium size.
Histologically they are composed of bipolar spindle cells with a focal nuclear palisading pattern. There are areas of high cellularity named Antoni A and with low cellularity and myxoid matrix named Antoni B [7]. When schwannomas show pronounced degenerative changes including cyst formation, hemorrhage, calcification, and hyalinization these are termed “ancient” schwannomas [3]. “Ancient variety” is a rare form of schwannoma, which was initially mentioned by Ackerman and Taylor. These degenerative features are attributed to the growth and “aging” of the tumour, histologically characterised by nuclear hyperchromasia, mild nuclear pleomorphism, stromal oedema, fibrosis and xanthomatous changes leading to a misdiagnosis of malignancy in the aspirates [1]. Immunohistochemically, these tumours show diffuse positivity for S100 protein in the cytoplasm of the tumour cells [1].
When degenerative changes occur in these tumours, they pose a preoperative challenge in clinical and radiological diagnosis. Pancreatic tumours(cystadenoma, cystadenocarcinoma), smooth muscle tumours(leiomyoma,leiomyosarcoma), fat tumours (lipoma, liposarcoma), fibrous tumours (fibroma,fibrosarcoma), vascular tumours (haemangiopericytoma), psoas abscess, retroperitoneal Hemorrhage and hydatid cyst are known to mimic with similar imaging appearances [2]. Degeneration is due to central tumour necrosis as the schwannoma grows to a size beyond the capacity of its blood supply. Cystic changes occur more commonly in retroperitoneal schwannomas (upto 66%) compared to other retroperitoneal tumours [1].
Ultrasonography is inexpensive but very non-specific in the detection of these tumours. Mixed echogenicity is a common feature in these cases. CT scan and MRI are more helpful in detecting specific characteristics of the tumour. Size, exact location, relationship with other organs and invasion can be accurately reproduced. Calcification and cystic degenerations seen in ancient schwannomas are also well made out [7]. MRI is the examination of choice and presents iso- or slightly hyper-intensity on T1 weighted images. However, in our case the tumour presented hypointense on T1 and hyperintense onT2 weighted images. Compared to CT scan, MRI has higher specificity, better resolution and can delineate the tumour better, but still it cannot distinguish between benign and malignant tumours [8].
Most of the retroperitoneal and pelvic schwannomas throw a challenge to the operating surgeon due to its proximity to vital structures. Though most of them are benign and well encapsulated they have a significant potential for recurrence if not excised in toto. The rates of local recurrence range from 16% to 54% after conservative intralesional enucleation [9]. So, local excision should be the treatment of choice, sparing the adjacent vital organs. However, some surgeons believe that since malignancy cannot be excluded preoperatively, or with intra-operative frozen section, clear margins should be attained even if other organs have to be sacrificed. Malignant retroperitoneal schwannomas are very rare and account for about 1% of all retroperitoneal schwannomas [10].The prognosis of benign schwannomas is good when excised. The most frequent complication is recurrence, probably due to incomplete excision, which is reported in 5-10% cases [11].
Contrast MRI LS Spine showing a large heterogeneously enhancing, well-encapsulated retroperitoneal mass at the level of L4 vertebra
Intra-operative pictures. (a) Showing the mass measuring 7x8 cm with the left ureter stretched and displaced laterally. (b) Showing the mass displacing the left common iliac vessels inferiorly
Histopatholgical images of the specimen: (a) 10x image showing high cellularity Antoni A regions (ARROW), low cellularity Antoni B regions (STAR) along with areas of hyalinization and blood vessels showing degenerative changes. (b) 20x image showing bipolar spindle cells in Antoni A regions

Imuunohistochemistry showed neoplastic cells diffusely positive for S 100 protein
Conclusion
Ancient neurilemmoma in a young male occurring in the least probable retroperitoneal site with degenerative changes occurring in a relatively small to medium sized neurilemmoma is indeed a rare finding. It is important therefore to accurately assess and investigate such patients who present with non-specific symptoms and despite radiological and cytological investigations, pose a preoperative diagnostic dilemma due to degenerative changes. Surgical excision of the entire tumour is the treatment of choice.
[1]. A Narasimha, MH Kumar, RR Kalyani, R Madan, Retroperitoneal cystic schwannoma: a case report with review of literatureJ Cytol 2010 27:136-39. [Google Scholar]
[2]. LM Toh, SK Wong, A case of cystic schwannoma of the lesser sacAnn Acad Med Singapore 2006 35:45-48. [Google Scholar]
[3]. B Goh, Y Tan, Y Chung, PK Chow, LL Ooi, WK Wong, Retroperitoneal schwannomaAm J Surg 2006 192:14-18. [Google Scholar]
[4]. Y Aslan, AÖ Aydin, ÜY Tekdogan, A Atan, Retroperitoneal Schwannoma: A Case Report and Review of The LiteratureJ Neurol Sci [Turk] 2010 27:353-58. [Google Scholar]
[5]. Q Li, C Gao, JT Juzi, X Hao, Analysis of 82 cases of retroperitoneal schwannomaANZ J Surg 2007 77:237-40. [Google Scholar]
[6]. J Cury, RF Coelho, M Srougi, Retroperitoneal schwannoma: case series and literature reviewClinics 2007 62:359-62. [Google Scholar]
[7]. T Theodosopoulos, VK Stafyla, P Tsiantoula, Special problems encountering surgical management of large retroperitoneal schwannomasWorld J Surg Oncol 2008 6:107-12. [Google Scholar]
[8]. K Hayasaka, Y Tanaka, S Soeda, P Huppert, CD Claussen, MR findings in primary Retroperitoneal schwannomaActa Radiol 1999 40:78-82. [Google Scholar]
[9]. S Andonian, PI Karakiewicz, HW Herr, Presacral cystic schwannoma in a manUrology 2003 62:8-10. [Google Scholar]
[10]. Neuroradiology: Neurilemmoma. Medcyclopaedia website http://www.medcyclopaedia.com/library/topics/volume_vi_1/n/neurilemmoma Accessed 1 May 2009 [Google Scholar]
[11]. JY Song, SY Kim, EG Park, CJ Kim, DG Kim, HK Lee, IY Park, Schwannoma in the retroperitoneumJ Obstet Gynaecol 2007 33:371-75. [Google Scholar]