Blastic Phase of CML with Microfilaria: A Rare Case Report
Suniti Pahwa1, Annapurna Saksena2, Ashu Singh3, M. K. Daga4, Tejinder Singh5
1 Junior Resident, Departments of Pathology, Maulana Azad Medical College, New Delhi, India.
2 Junior Resident, Departments of Pathology, Maulana Azad Medical College, New Delhi, India.
3 Junior Resident, Departments of Pathology, Maulana Azad Medical College, New Delhi, India.
4 Professor, Department of Medicine, Maulana Azad Medical College, New Delhi, India.
5 Director Professor, Department of Pathology, Maulana Azad Medical College, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Annapurna Saksena, Junior Resident, Department of Pathology, Maulana Azad Medical College, New Delhi, India. E-mail : anusaksena@gmail.com
Filariasis is a major public health concern in tropical and subtropical countries including India. There have been very few case reports of incidental filariasis in the bone marrow aspirate smears in patients with hematological malignancies. We present a case of blastic phase of chronic myeloid leukemia (CML) with associated filariasis with monocytosis. Such an association, to the best of our knowledge, is hitherto unreported. Moreover, eosinophilia was not a feature in our case.
A 37-year-old male, diagnosed case of CML, presented with low grade fever, weight loss and abdominal distension for one month. Physical examination revealed massive splenomegaly and hepatomegaly. However, there was no lymphadenopathy. His hemoglobin was 10.5 g/dl, total leukocyte count was 52.31x 109 / L with platelet count of 30x 109/L .Differential leukocyte count on peripheral smear showed 21% blasts, 30% polymorphs, 16% lymphocytes, 1% myelocyte, 1%metamyelocyte, 30%monocytoid cells and 1% eosinophils.
Bone marrow aspirate smears were diluted with peripheral blood and showed blasts and monocytoid cells constituting 25% and 15% of marrow nucleated cells respectively. In addition, occasional microfilaria of Wuchereria bancrofti were also seen both in the peripheral blood and aspirate smears.
Based on the above findings, a diagnosis of blastic phase of CML with monocytosis with microfilaria of W.bancrofti.
Hence this was an unusual case of CML blastic phase which was associated with filariasis. Moreover, inspite of having filariasis and CML, patient lacked eosinophilia and instead showed monocytosis, which is hitherto unreported.
Filariasis, Microfilaria, Leukemia, W.bancrofti
Case Report
A 37-year-old male, diagnosed case of CML on Imatinib mesylate, presented with low grade fever, weight loss and abdominal distension for one month. Physical examination revealed massive splenomegaly and hepatomegaly, however there was no lymphadenopathy.
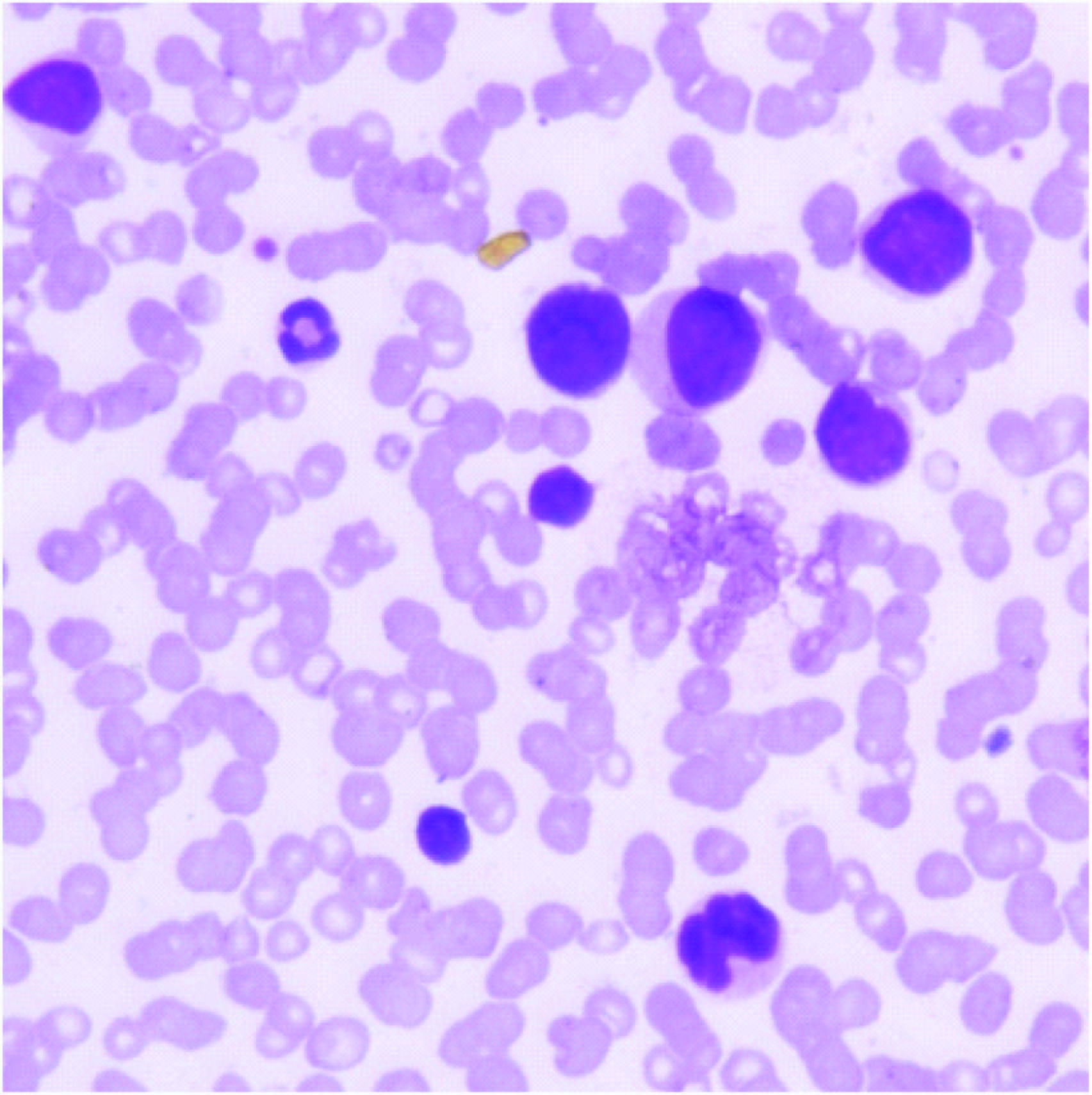
His hemoglobin was 10.5 g/dl, total leucocyte count was 52.31 x 109 / L with platelet count of 30 x 109/L. Differential leucocyte count on peripheral smear showed 21% blasts [Table/Fig-1], 30% polymorphs, 16% lymphocytes, 1% myelocyte, 1%metamyelocyte, 30%monocytoid cells and 1% eosinophils. Blasts were large with high N: C ratio, pale basophilic cytoplasm, some of them showed 1-4 nucleoli. In addition, occasional microfilaria was also seen [Table/Fig-2]. They were morphologically characterized as the microfilaria of W. bancrofti, as they were sheathed and lacked terminal nuclei.
Peripheral smear showing blasts and a few monocytoid cells (H&E 40X)
Bone marrow aspirate showing sheathed microfilaria with tip free from nuclei
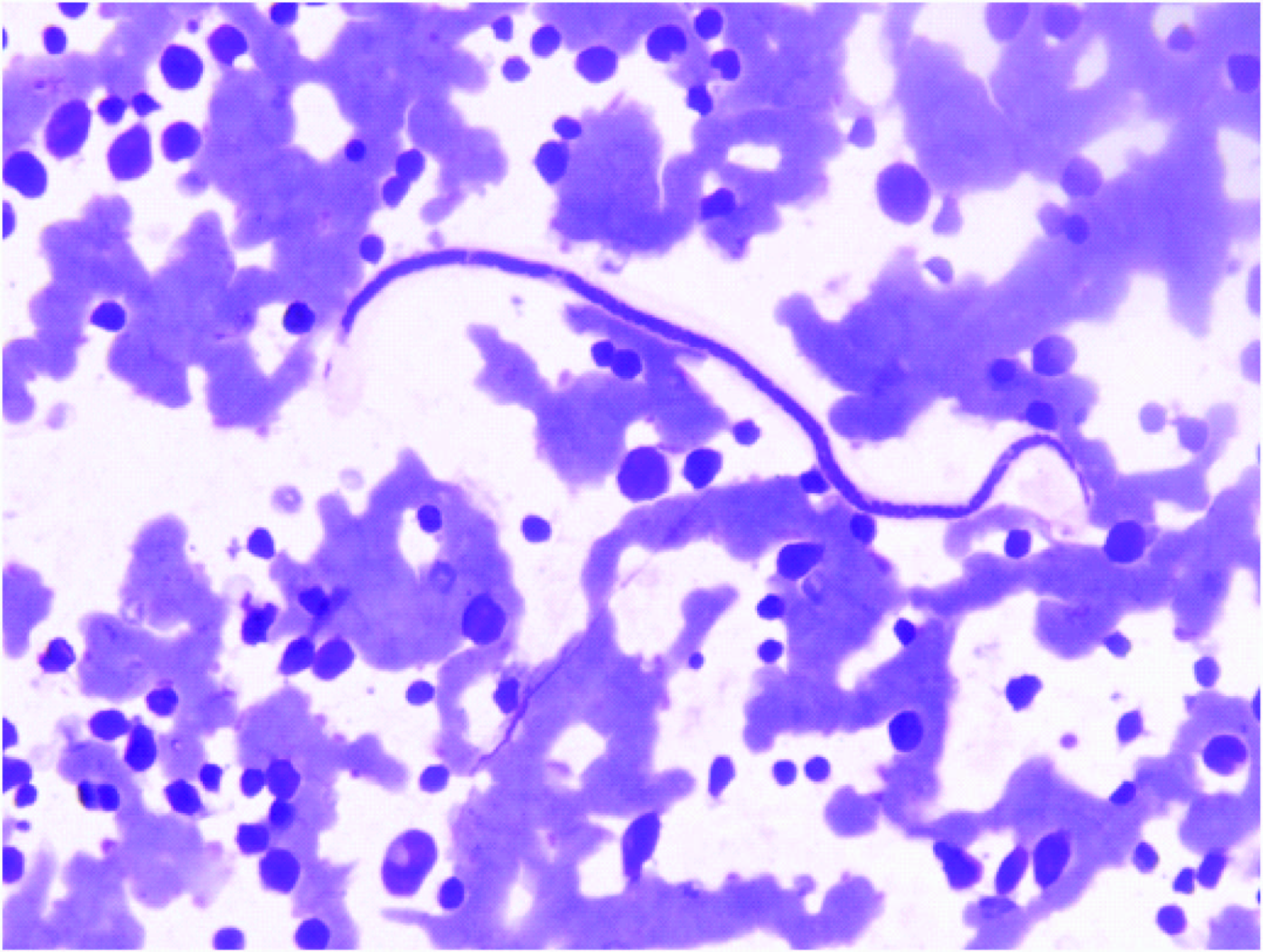
Bone marrow aspirate smears were diluted with blood. However, they showed blasts and monocytoid cells accounting for 25% and 15% of marrow nucleated cells respectively .The blasts had same morphology as in peripheral smear. Few megakaryocytes were seen. In addition, occasional microfilariae of Wuchereria bancrofti were seen but no significant eosinophilia was seen as in peripheral blood.
Bone Marrow biopsy smears were hypercellular for age with a cellularity of 90%. Marrow showed increase in blasts with round nuclei with prominent nucleoli. Another distinct population of cells with vesicular and lobulated nuclei was seen (monocytoid). No microfilaria was seen.
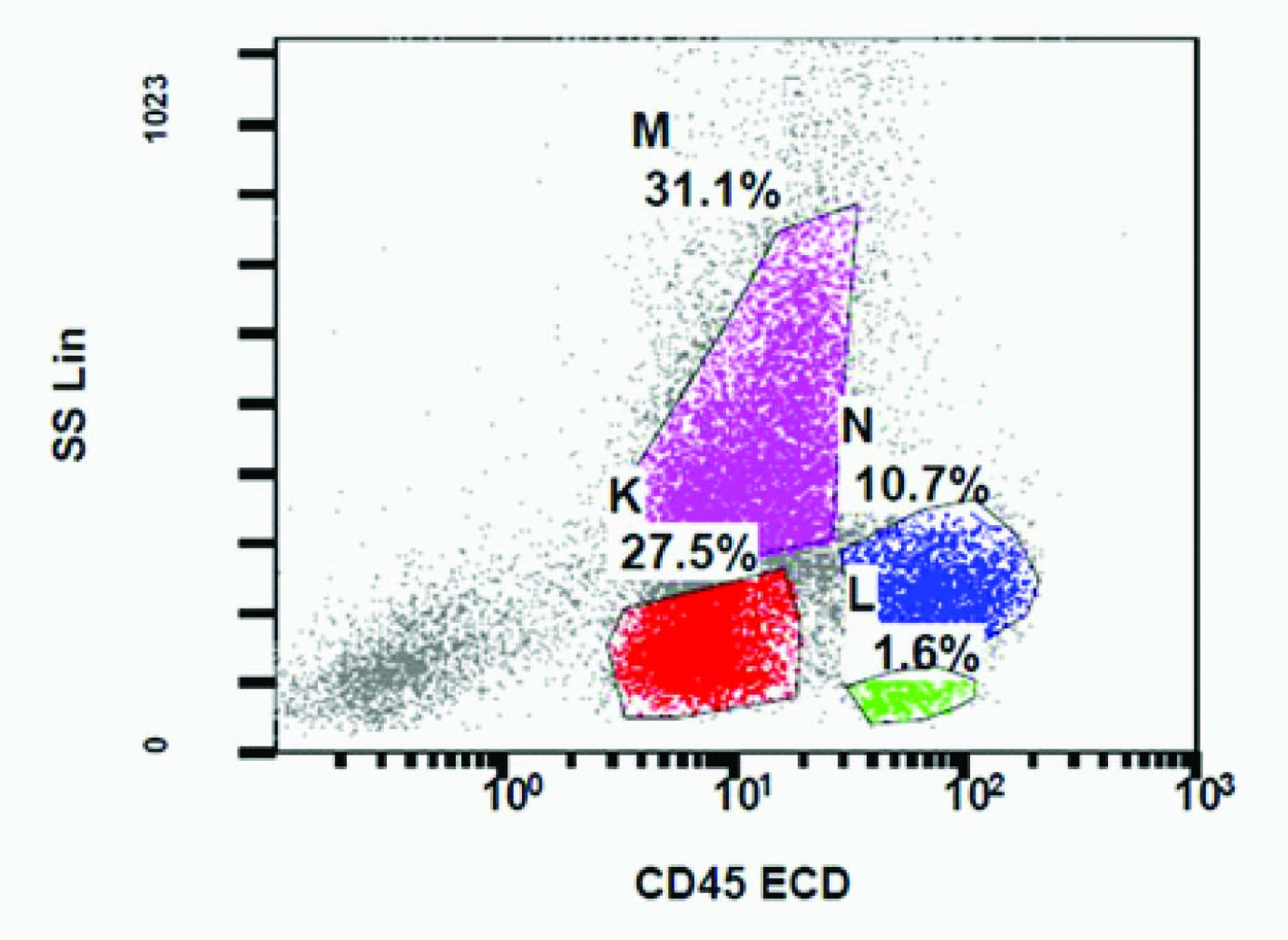
Flow cytometry was done on the peripheral blood and cells were gated on CD45/SSC plot. There were 28% cells in the blast window and 11% monocytes along with maturing granulocytes and few lymphocytes [Table/Fig-3]. Blasts cells were dim positive for CD13 and CD34. The monocytoid population of cells showed dim to moderate positivity for CD11c and CD13 and was negative for CD34.
Flow plot showing maturing granulocytes, blast population and monocytes
Based on the above findings diagnosis of blastic phase of CML with monocytosis with microfilaria of W.bancrofti was made.
Patient was treated with DEC (Diethylcarbamazine citrate tablets) tablets (3 Tabs of 100 mg each stat) for filariasis. Dose of imitanib was increased from 400mg to 800mg. Subsequent peripheral smears and aspirates were free of filariae.
Discussion
Filarial infection is endemic in some parts of India. It may be associated with any disorder. Even when not suspected clinically, microfilaria may be sometimes found in peripheral smear or bone marrow smear [1].
The larvae, once deposited at the site of puncture, slowly enter through the skin on their own and reach the lymphatic channels to settle down in regional lymph nodes. There, they mature in 5-18 months time producing new larvae which then enter through the thoracic duct into the venous system, pulmonary capillaries and finally into the peripheral circulation [2]. Thus they may enter in any part of the circulatory system including the bone marrow. However, presence of microfilaria on bone marrow aspirate is unusual and rare [2].
Asymptomatic microfilaremia is relatively common in India [3]. The coexistence of microfilaria and malignancy may be coincidental. Filariasis, in association with solid malignancies, is well-described in literature. However, so far, there have been only three case reports of incidental finding of filariasis on bone marrow aspirate with co existing hematological malignancies. Jain et al., reported coexistence of microfilaria with CD10 positive B-cell ALL and also with Hodgkin’s lymphoma [1]. Sharma et al., found coincidental microfilaria in a case of AML- M4 with eosinophilia [4]. However,to the best of our knowledge, this is the first case report of CML with associated filariasis.
Lymphatic filariasis commonly presents as lymphangitis, elephantiasis and eosinophilia. However, it has been reported that in cases of bone marrow microfilaria, the above mentioned classical clinical presentation is often lacking [5–12]. Similarly our case also lacked the classical clinical presentation. The diagnosis of filariasis was made after demonstration of the microfilaria in the bone marrow aspirate.
Peripheral blood eosinophilia is a common hematological finding in filariasis. Our case was unique since it lacked eosinophilia. This is similar to a few other reported cases where bone marrow microfilaria was associated with lack of eosinophilia [6,8,10]. The absence of peripheral blood eosinophilia in these cases may be due to altered immune response secondary to malignancy or due to the oxidative stress associated with filariasis [13].
Another interesting feature observed was presence of monocytosis. The cause for this was not established. This may have been as a part of CML or due to an unusual reaction to microfilaria. The latter is not yet reported.
Conclusion
Hence, it is concluded that in endemic countries, the possibility of microfilaria should be kept in mind in patients with fever, even in the absence of classical clinical presentation or eosinophilia and the peripheral smears and aspirates should be screened with a high index of suspicion. This will ensure that a treatable infection is not missed in the presence of more malignant condition.
[1]. Jain S, Sharma M, Jasmita Tyagi S, Common parasite with uncommon associationMediterr J Hematol Infect Dis 2011 3e2011015,DOI10.4084/MJHID.2011.015 [Google Scholar]
[2]. Chartterjee KD, Parasitolgoy in Relation to Clinical Medicine 1969 7th edition:180-83. [Google Scholar]
[3]. Sabesan S, Vanamail P, Raju K, Jambulingam P, Lymphatic filariasis in India: Epidemiology and control measuresJ Postgrad Med 2010 56:232-38. [Google Scholar]
[4]. Sharma P, Tyagi S, An Unusual Cause of Eosinophilia in AML-M4 without the Inv (16) AbnormalityJ Blood Disord Transfus 2010 1:104doi:10.4172/2155-9864.1000104 [Google Scholar]
[5]. Anupindi L, Sahoo R, Rao RV, Verghese G, Rao PV, Microfilariae in the bronchial brushing cytology of symptomatic pulmonary lesions. A report of two casesActa Cytol 1993 37:397-99. [Google Scholar]
[6]. Sharma S, Rawat A, Chowhan A, Microfilariae in bone marrow aspiration smears; their correlation with marrow hypoplasia: a report of six casesIndian J Pathol Microbiol 2006 49:566-68. [Google Scholar]
[7]. Hemachandran M, Varma N, Varma S, Aplastic anaemia following a varicella infection with a coexistent microfilaraemia of Wuchereria bancrofti- a case reportIndian J Pathol Microbiol 2003 46:662-63. [Google Scholar]
[8]. Pradhan S, Lahiri VL, Elhence BR, Singh KN, The microfilariae of Wuchereria bancrofti in bone marrow smearsAm J Trop Med Hyg 1976 25:199-200. [Google Scholar]
[9]. Molina MA, Cabezas MT, Giménez MJ, Mansonella perstans filariasis in an HIV patient: a finding in the bone marrowHaematologica 1999 84(9):861 [Google Scholar]
[10]. Shenoi U, Pai RR, Pai U, Nandi GK, Adhikari P, Microfilariae in bone marrow aspiration smearsActa Cytol 1998 42:815-16. [Google Scholar]
[11]. Arundhati Kumar A, Kumar R, Acute lymphoblastic leukaemia with microfilaria: a rare coincidence in bone marrow aspiratesIndian J Hematol Blood Transfus 2011 27:111-12. [Google Scholar]
[12]. Panja M, Ganguly S, Kar AK, Chhetri MK, Atypical filariasisJ Assoc Physicians India 1987 35(8):596-97. [Google Scholar]
[13]. Pal BK, Kulkarni S, Bhandari Y, Ganesh BB, Goswami K, Reddy MV, Lymphatic filariasis: a possible pathophysiological nexus with oxidative stressTrans R Soc Trop Med Hyg 2006 100:650-55. [Google Scholar]