A Rare Case of Multple Myeloma (Mm) Presented With Pancytopaenia in A Patient of HIV – At Very Early Age
Sisir Kumar Patra1, Manoj Soren2, Anjan Kumar Das3, Srishtidhar Mangal4
1 Postgraduate Teacher, Department of Pathology, Calcutta National Medical College and Hospital, Kolkata, India.
2 Senior Resident, Department of General Medicine, Calcutta National Medical College and Hospital, Kolkata, India.
3 Associate Professor, Department of Pathology, Calcutta National Medical College and Hospital, Kolkata, India.
4 Associate Professor, Department of Pathology, Calcutta National Medical College and Hospital, Kolkata, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sisir Kumar Patra, A/1 Rameswar Apartment, 29-31 Sangha Sarani, Bally, Durgapur-Makaltala, Howrah, West Bengal-711205, India.
E-mail: dr.sisirpatra@rediffmail.com
Non-hodgkin`s lymphoma (NHL) is the most common haematological malignancy which is seen in HIV infected patients. Among NHLs, immunoblastic lymphomas are most common and a majority of these are diffuse large B-cell lymphomas. Multiple myeloma is a disease of the elderly. It is extremely rare below 30 years of age. On the other hand, in HIV infected individuals, the average age of presentation with plasma cell disorders is 33 years, which is far younger than the average age of presentation in general population. The incidence of AIDS defining malignancies has declined markedly, whereas non-AIDS defining cancers are being increasingly diagnosed in patients with HIV infection during the HAART-era and they may be the presenting manifestations of AIDS. Multiple myeloma, however, usually is not a first presenting feature of AIDS. The usual clinical presentation of multiple myeloma is bone pain and pallor. Pancytopaenia is a rare presenting feature of multiple myeloma. Here, we are reporting a case of pancytopaenia which occurred in a 28-year-old, newly diagnosed, HIV-1 positive female, who with the help of bone marrow examination and further investigations, was subsequently diagnosed as multiple myeloma.
Early age, Multiple myeloma, Pancytopaenia, HIV, CD4 lymphocyte
Case Report
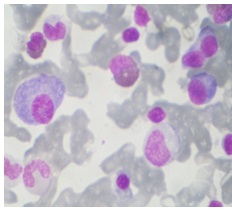
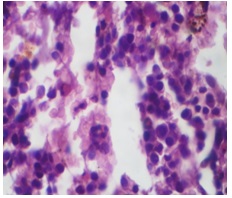
A 28–year-old female presented with severe asthaenia, persistent small nodular skin rashes of 6 months duration, fever and recurrent chest infections of 2 months duration and significant weight loss of 1 month’s duration. Physical examination revealed severe pallor, tender, firm hepatomegaly (8 cm from right lower costal margin), tachycardia, tachypnoea, bilateral basal crepitations. The patient was nondiabetic and normotensive. There was no past or contact history of tuberculosis or jaundice. She did not receive any blood transfusion. There was no significant past or family history. She was a maid servant by occupation. Her husband had died when he was around 32 years of age. The cause of death was not known, but according to patient, at the terminal stage, he had developed multiple ulcers over oral, anal and genital regions and was very much cachectic. Initial Investigations revealed normocytic, normochromic anaemia with haemoglobin - 3.5 gm/dl, total leucocyte count – 1900/cumm, platelets – 27,000/cumm with neutrophils -56%, lymphocytes -34%, eosinophils -6% and monocytes -4%. ESR was 116mm in 1st hr. Also, there was rolouaex formation in peripheral smear. Her fasting blood sugar was 98gm/dl, urea was 95mg/dl, creatinine was 1.7mg/dl. Liver function tests are within normal limits except albumin – 2.2g/dl and globulin – 3.5g/dl. Blood was tested for HIV-1 and 2 and for HBsAg and Anti-HCV. Patient was found to be HIV-1 positive. HBsAg and Anti-HCV were negative. The CD4 lymphocyte count was 270 cell/ mm3. For further evaluation of pancytopaenia, after proper consent and precaution, a bone marrow aspiration was done and it revealed an increased percentage of plasma cells (22%) in a hypocellular bone marrow [Table/Fig-1]. Subsequent bone marrow biopsy showed a trilineage depression of haematopoietic cells and diffuse infiltration by plasma cells [Table/Fig-2].
Photomicrograph of bone marrow aspiration showing plasma cell (Leishman Stain – Oil immersion)
Photomicrograph of bone marrow trephine biopsy showing atypical plasma cells (H&E stain 40X)
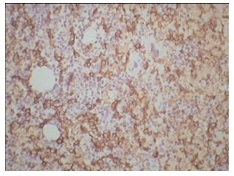
Extensive workup for evaluation of multiple myeloma was undertaken. The corrected serum calcium was 11.5 mg/dl. X-ray of skull and pelvis did not reveal any osteolytic lesion. Serum protein electrophoresis showed hypoalbuminaemia with a slightly increased alpha2 globulin fraction, and an M-band in gamma globulin region. Serum immunofixation electrophoresis revealed presence of Monoclonal IgG Kappa light chain, Serum IgG – 1592 mg/100ml, IgA-70mg/100ml,IgM-40mg/100ml,beta2-microglobulin – 10600 mcg/L. Urine immunofixation electrophoresis also showed Monoclonal IgG kappa light chain paraprotein. Bone marrow immunohistochemistry showed CD138 positivity [Table/Fig-3]. After diagnosing multiple myeloma, we started with thalidomide and dexamethasone and the patient was discharged and referred to School of Tropical Medicine, Medical College, Kolkata, India, for further management, as HAART therapy was not available in our institution.
Photomicrograph of bone marrow immunohistochemistry showing - CD138 positive
Discussion
Lymphoma occurs in both congenital or acquired immunodeficiencies, with an increased frequency. AIDS is no exception and the incidence is around 6% [1]. Lymphomas which are commonly found in patients with HIV infection are immunoblastic lymphoma, Burkitt`s lymphoma, primary CNS lymphoma. 90% of these lymphomas are of B cell type in phenotype [1]. Multiple myeloma is a malignant disorder which is characterized by the proliferation of monoclonal plasma cells which develop from common progenitors in the B lymphocyte lineage. But they are very rare in HIV infected patients [2]. The peak incidence of MM is in the seventh decade, whereas, it is a rare entity in young patients, with less than 2% cases occurring in patients who are under the age of 40 years and it is still rarer in patients who are younger than 30 years [3]. Although HIV positive patients are at an increased risk of development of aggressive, disseminated and extranodal B cell lymphoma [4], in the setting of B-cell stimulation and activation , frank multiple myelomas are seen less frequently. However, the frequency of multiple myeloma in HIV infected individuals is increased as compared to that in general population [5]. HIV infection plays a major role in the evolution of plasma cell neoplasms. Several studies demonstrated that marked abnormalities of B cell activation and immunregulation occur in AIDS patients. Polyclonal B cell activation is commonly observed [6] and it may represent a signal for B lineage tumourigenesis. Elevated IL-6 plasma levels have been detected in HIV infected patients [7]. This apparent overproduction of IL6 promotes B cell proliferation, immunoglobulin secretion, myeloma cell growth and it has been suggested that it has a central role of in the pathophysiology of myeloma [8].
IL-6 is a multifunctional cytokine which is induced by a variety of stimuli, including bacteria, viruses and other cytokines. Many viruses can stimulate IL-6 production, in particular HIV, human herpes virus 8 and Epstein-Barr virus. Co-infection with other viruses such as Epstein-barr, human herpes virus-8 can cause clonal expansion of plasma cells. Finally, it appears that HIV-1 antigen can induce clonal selection that plays a part in the pathogenesis of plasmacytic disorders. Indeed, Konrad et al. reported an HIV-1-positive patient with myeloma, whose IgG kappa paraprotein specifically recognized the HIV-1 p24 antigen.
In addition, the observation that T cells were able to induce terminal differentiation of transformed B cells into mature plasma cell tumours [9] might explain the high frequency of lymphoma as compared to that of myeloma in AIDS patients who were depleted of T cells. In the future, highly active antiretroviral therapy and immune restoration may favour the emergence of plasma cell neoplasms rather than AIDS defining malignancies, the incidence of which has decreased as a consequence of HAART therapy.
It is not straightforward to distinguish between HIV positive patients with plasma cell neoplasms and non-infected patients, because both share some clinical and laboratory features such as recurrent bacterial infections, anaemia, benign polyclonal hypergammaglobulinaemia, bone marrow plasmacytosis. But plasma cell neoplasms involve higher number of patients and they present at younger ages in HIV infected individuals than in general population. The overall incidence of monoclonal gammopathy in general population is 0.15% [10], whereas in HIV positive individuals, the incidence is higher, about 2.5% [11].
Our patient had some unique characteristics. First of all, she was just 28-year-old and multiple myeloma rarely develops in this age group. The average age of presentation of plasma cell disorders among HIV-infected individuals is 33 years, which is very much younger than the average age of presentation in general population [2]. Secondly, tri-lineage depression of haematopoiesis caused by multiple myeloma leads to development of pancytopaenia, but multiple myeloma which presents as pancytopaenia has a very rare incidence. Thirdly, our patient was diagnosed as HIV-infected in our institution. So, she had not received any type of HAART earlier. Despite that, patient developed multiple myeloma first rather than AIDS-defining malignancies.
Conclusion
In B cell lymphoma, myeloma patients, especially young patients, should be systematically screened for HIV, and HIV-positive patients should be monitored for the occurrence of monoclonal gammopathy.
[1]. Anthony S, Fauci H, Clifford Lane, Human immunodeficiency virus disease: AIDS and related disorders. In : Longo, Fauci, Kasper, Hauser, Jameson, LoscalzoHarrison’s Principles of Internal Medicinevolume-118th edition(189):1566 [Google Scholar]
[2]. Fiorino AS, Atac B, Paraproteinemia, Plasmacytoma, Myeloma and HIV infectionLeukemia 1997 11:2150-56. [Google Scholar]
[3]. Ishida T, Dorfman HD, Plasma cell myeloma in unusually young patient: A report of 2 cases and review of literatureSkeletal Radiol 1995 24:47-51. [Google Scholar]
[4]. Levine AM, Meyer PR, Begandy MK, Parker JW, Tailer CR, Irwin L, Developement of B cell lymphoma in homosexual menAnn Intern Med 1984 100:7-30. [Google Scholar]
[5]. Pantanowitz L, Dezube BJ, Editorial comments: Multiple myeloma and HIV infection- causal or causal to incidence?AIDS Read 2003 13(8):386-87. [Google Scholar]
[6]. Lane HC, Masur H, Edgar LC, Whalen G, Rook AH, Fauci AS, Abnormalities of B cell activation and immunoregulation in patients with acquired immunodeficiency syndromeN Engl J Med 1983 309:453-58. [Google Scholar]
[7]. Breen EC, Rezai AR, Nakajima K, Infection with HIV is associated with elevated IL-6 level and productionJ Immunol 1990 144:480-84. [Google Scholar]
[8]. Klein B, Zhang X, Jourdan M, Paracrine rather than autocrine regulation of myeloma-cell growth and differentiation by interleukin-6Blood 1989 73:517-26. [Google Scholar]
[9]. Hilbert DM, Shem MY, Rapp UR, Rudikoff S, T cell induce terminal differentiation of transformed B cells to mature plasma cell tumorsProc Natl Acad Sci USA 1995 92:649-53. [Google Scholar]
[10]. Fine JM, Lambin P, Derycke C, Muller JY, Marneux M, Systematic survey of monoclonal gammopathy in the sera from blood donorsTransfusion 1979 19:32-35. [Google Scholar]
[11]. Lefre`re JJ, Fine JM, Lambin P, Muller JY, Couroux AM, Salmon C, Monoclonal gammopathies in asymptomatic HIV-seropositive patientsClin Chem 1987 33:1697-98. [Google Scholar]