The use of oestrogen medication for treatment of vaginal atrophy is rapidly increasing with the rise of population of postmenopausal women. An estimated 10 to 40 percent of postmenopausal women have symptoms of vaginal atrophy, also referred to as urogenital atrophy [1,2]. Although there are some clinical tests like vaginal pH and vaginal maturation indexes for diagnosing vaginal atrophy, clinicians prescribe oestrogen and lubricant therapy to alleviate postmenopausal patients’ complaints without investigating their clinical experiences [3]. Because it is easy to just prescribe oestrogen or lubricants to patients without performing any expensive and time-consuming laboratory tests, Hormonal therapy or lubricants are being excessively used by postmenopausal women without clinically proven vaginal atrophy. At the same time, although treatment with topical oestrogen and lubricants is effective in alleviating symptoms, women frequently do not report symptoms and thus go untreated [4].
Initially we planned to investigate whether it would be possible to use Wood’s Light (WL) [Table/Fig-1] for the diagnosis of vaginal atrophy. Vaginal mucosal atrophy, that occurs in menopause, shows a different colour under WL. As the oestrogen levels decrease at menopause, the vaginal epithelium loses it rugae and becomes thin and pale [5]. Light of short and long wavelengths provides superficial and deep layer information, respectively. Most of the blue light emitted is absorbed by hemoglobin, resulting in blood vessels appearing as a dark red color or the colour changes into green or intensity of redness changes [6].Therefore, vessels under the vaginal mucosa can be seen easily with fluorescent light when vaginal atrophy is present. Wood’s light is a useful diagnostic tool for dermatologic disorders, vitiligo, fungal infections, acne, erythrasma, tinea versicolor, microsporum canis, scabies, alopecia, porphyria, bacterial infections, and many other skin conditions [7].
The WL lamp is a device that emits ultraviolet (UV) light in the 365-nanometer range and is used by dermatologists to assess the diagnosis of various pigment and infectious disorders [8]. WL emits long-wave ultraviolet radiation and has a compound filter made of barium silicate with 9% nickel oxide, the “Wood's filter.” This filter is opaque to all light rays except a band between 320 and 400 nm with a peak at 365 nm. Fluorescence of tissues occurs when the WL is absorbed and radiation of a longer wavelength, usually visible light, is emitted during the WL examination based on the colour of fluorescence of the affected skin [8]. We aimed to asses the feasibility and diagnostic accuracy of WL for vaginal atrophy.
We encountered pale royal green fluorescence images in 36 of the 45 postmenopausal women’s atrophic vaginas with WL examination. Here, we present our experiences in postmenopausal women where we had used a WL lamp for the evaluation of vaginal atrophy.
Materials and Methods
The ethical committee permissions have been taken for this study through the local ethics committee. A case control study was conducted at the Department of Obstetrics and Gynaecology at the Gulhane Military Medical Academy from 1 March 2013 to 1 September 2013. The patients were informed about the examination process, and they provided informed consent. They were also informed that photographs of the speculum area would be taken without revealing their identity. Fourty-five healthy postmenopausal women complaining of vaginal dryness, dyspareunia, vulvar pruritus, and itching caused by menopause and 45 healthy women of reproductive age with no complaints were included in this study. All the patients had been referred to our clinic for routine examinations, and they underwent speculum examinations, serum glucose, renal, liver and thyroid function tests, follicular stimulating hormone and Beta human chorionic gonadotropin (B-hCG) testing for reproductive age women, Pap smear urinalysis and microbiological culture of the vagina and urine and endometrial thickness for postmenopausal women. After these tests, postmenopausal women who had vaginal atrophy symptoms and signs were selected for this study and recalled for photography of the vaginal mucosa for Wood’s light examination. Reproductive-aged women whose test results were negative were recalled on the 10th day of the menstrual cycle for photography of the vagina with Wood’s light examination.
The inclusion criteria for the postmenopausal group were menopausal status for at least five years and atrophic changes, a Pap smear, a vaginal pH above 5, and women of reproductive age who had regular menses and no gynaecological complaints whose pregnancy tests were negative.
The exclusion criteria were pregnancy, smoking, vaginal or urinary infections, cervical smear abnormalities, women who used hormone replacement therapy, any vaginal medication or lubricant use or sexual intercourse prior to 10 days from the examination day any gynaecological surgical conditions, a chronic illness like diabetes mellitus, liver and renal failure, hepatitis, and any skin diseases for all patients.
We excluded patients who had sexual intercourse or applied vaginal medications because the presence of semen or vaginal infections could produce a fluorescent colour with Wood’s light.
At the first visit, all patients received the aforementioned gynaecological examinations and tests. Patients who were suitable for this study were recalled for a second examination.
According to our experiences with Wood’s light, it is not easy to differentiate the pale royal green colour at first sight. Every patient was examined in the lithotomy position using single-use, sterile vaginal speculums made of clear transparent plastic material. A WL lamp was allowed to warm up for about one minute. Warming of the WL is important because it can only produce appropriate fluorescent light after the lamp is heated. The examination was performed in a dark room. The WL was held about 10 - 13 centimetres (4 to 5 inches) away from the vulva to illuminate directly the affected area for 10 seconds, and any changes in the colour or fluorescence were observed.
Results
We had studied 45, healthy postmenopausal women with atrophic vaginitis (study group) and 45 healthy, reproductive-aged women as a control group whose demographic data were matched.
The demographic characteristics of our postmenopausal and reproductive-aged groups are shown in [Table/Fig-2]. The postmenopausal group’s mean age was 59.2 (53-67 y), while the reproductive-aged women’s mean age was 27.6 (23-31 y). Thirty-six of the postmenopausal group (n=45) were visualized as having a pale royal green colour on transparent speculum under WL examination [Table/Fig-3a]. Thirty-nine of the reproductive aged women’s vaginas (n=45) did not have a pale royal green (colourless with transparent speculum) fluorescence under WL [Table/Fig-3b]. The postmenopausal group’s mean parity was 2.7, while that of reproductive-aged women was one. Also, the postmenopausal group’s mean FSH and E2 levels were 64.9 and 5, and the reproductive-aged women’s mean FSH and E2 levels were 5 and 10.8. p-values under 0.001 were considered statistically significant. The Mann Whitney U-test was used for statistical comparisons.
The demographic properties of our postmenopausal and reproductive-aged groups
| Postmenopausal Group n:45 Mean±sd | Reproductive Aged Women Group n:45 Mean±sd | p-value |
|---|
| Age | 59.2 ± 3.9 | 27.6 ± 2.4 | <0.001 |
| Parity | 2.7 ± 0.7 | 1 ± 0.3 | <0.001 |
| FSH (pq/ml) | 64.9 ± 14.4 | 5 ± 1 | <0.001 |
| E2 (mlU/Ml) | 5 ± 0 | 10.8 ± 2.5 | <0.001 |
A: Postmenopausal atrophic vagina; pale royal green with WL
B: Normal reproductive age women’s vagina (control group)
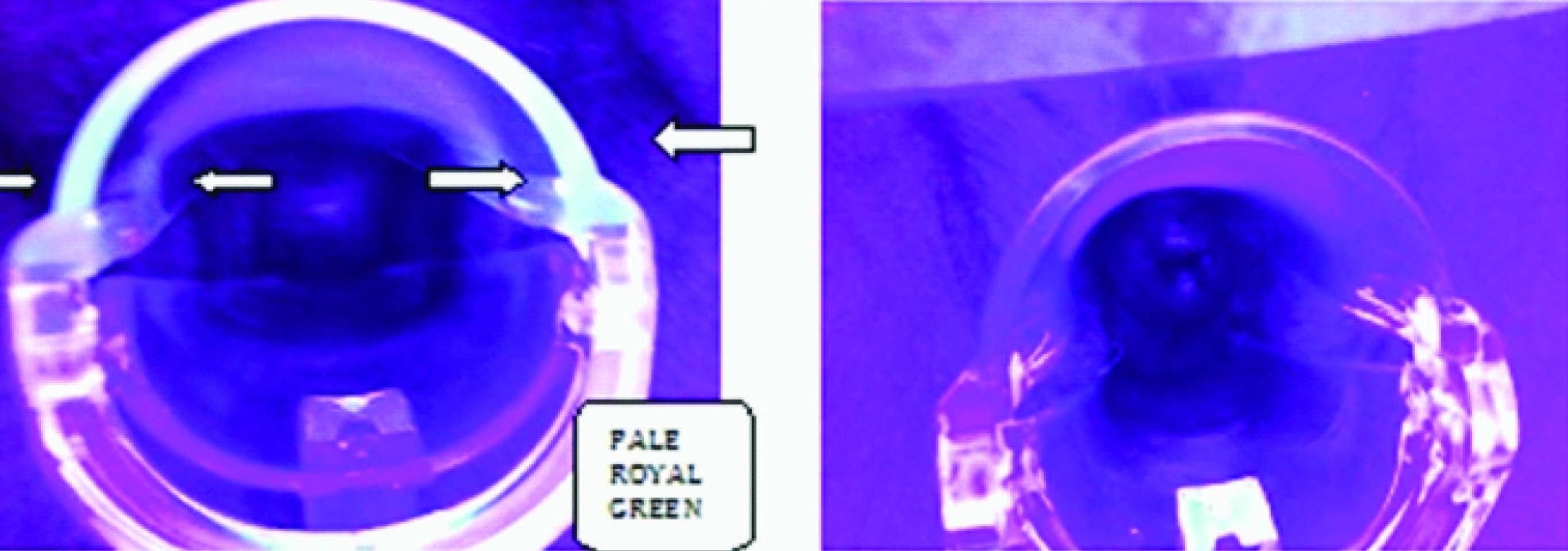
Both the postmenopausal group and the reproductive-aged group had not experienced any vaginal or urinary infections. All the cultures were negative in both groups. The reproductive aged women’s pregnancy tests were also negative. In postmenopausal women, endometrial thicknesses were under 5 mm, and all the vaginal pH were above 5. Both groups’ Pap smear results were negative for malignancy and cervical dysplasia. Postmenopausal women’s Pap smear results were positive for atrophic changes. There were no chronic illnesses for both groups. Due to the study design, there were no smokers in either group. There were 36 women in the postmenopausal group (n: 45) whose vaginas were seen as a pale royal green colour with the Wood’s light. Nine women in the postmenopausal group and 39 women of reproductive age did not have significant fluorescence illumination with the Wood’s light and appeared colourless [Table/Fig-4]. Six women in the reproductive-aged group also did not have a significant illumination and appeared purple. It may be due to vaginal infections which remained undiagnosed in the vaginal culture.
Fluorescence illumination with the Wood’s light in the postmenopausal group and reproductive aged women
| Postmenopausal women n:45 | Reproductive aged women n:45 |
|---|
| Wood's Light (+) | 36 | 6 |
| Wood's Light (-) | 9 | 39 |
The sensitivity of Wood’s light in the determination of vaginal atrophy was calculated to be 80% (95%, CI 0.66–0.89) with a specificity of 86% (95%, CI 0.73–0.93). The positive likelihood ratio of Wood’s light in the determination of vaginal atrophy as a diagnostic test was 6.0 (95%, CI: 2.80-12.81) with a negative likelihood ratio of 0.23 (95%, CI: 0.12-0.41). The diagnostic odds ratio was 26.0 (95%, CI: 8.4-80.3).
Discussion
Oestrogen, which is produced by the ovaries, plays a vital role in keeping vaginal tissues lubricated and healthy. It encourages the growth and development of vaginal epithelial cells, which make up the thick, healthy layers of the vaginal wall and condone a moist, supple, and elastic environment [9]. When levels of oestrogen are low, vaginal tissue becomes atrophic, thin, dry, and shrunken. Vaginal atrophy typically develops so slowly that a woman may not notice any symptoms until five to ten years after menopause begins. A diagnosis of atrophic vaginitis is based on the patient’s history and physical examination findigs [5,10]. Symptoms are vaginal dryness, burning, pruritus, and dyspareunia. Atrophy of the labia, loss of subcutaneous fat tissue, or loss of pubic hair can also be seen. Findings of vaginal atrophy on pelvic examinations are pale, smooth, dry, fragile vaginal epithelium, areas of petechiae, and rash [11,12]. Although, signs of vaginal atrophy were detected during gynaecological examinations, some of women didn’t have any related symptoms. Vaginal pH could be used to clarify vaginal atrophy. A pH > 5 may indicate vaginal atrophy [13]. However, there are some limitations to detect vaginal pH because it can change in vaginal infections and could cause a misdiagnosis of atrophic vaginitis. In women with vaginitis, vaginal pH measurements have increased false positive results due to overgrowth of facultative and obligate anaerobic bacteria [14].
The vaginal maturation index, which is available through vaginal cytology, may present the hormonal status of the vagina. The total number of parabasal, intermediate, and superficial cells in 100 cells from smear are counted, and the mean index is determined. If the majority of cells in the smear are superficial cells, oestrogen is sufficient. When parabasal and intermediate cells are dominant, it reflects a hypo-oestrogenomic state [15]. This test can be performed in pathology laboratories, but it is time consuming and is not cost effective for treatment. However, it is suitable for sexual function indices research and also for academic research purposes. Up to 70 percent of women with vaginal atrophy do not discuss their conditions with their health care provider [16]. Some believe that this condition is normal. Also, a woman’s symptoms do not always correlate with their physical findings [14]. A woman who has had no sexual intercourse would not report discomfort or pain, while a woman who has had intercourse would have dyspareunia or discomfort. Therefore, a diagnosis of vaginal atrophy should be made by considering both the patient’s clinical signs and reported symptoms.
In our study, we wanted to evaluate old device but a new technique to diagnose vaginal atrophy accurately that was simple, fast, and easy. We thought that WL would be a suitable instrument for this task. We chose this tool from dermatological examinations with WL as it is very useful in some dermatological fungal infections and skin diseases [8]. According to our literature review, this study was the first to use WL in the assessment of vaginal atrophy. There is only one study using WL in gynaecology. Oral 5-aminolevulinic acid was administered to patients by Duska LR et al., and excellent absorption was documented with a WL lamp in cervical dysplasia on biopsy [17].
Postmenopausal women with vaginal atrophy produced a fluore-scence colour like pale royal green in our study with WL examination. We observed this fluorescent colour in 36 postmenopausal women with atrophic vaginitis. All reproductive aged women except for six participants didn’t produce a fluorescence colour in our study with WL examination. These six participants however, didnot show signs of vaginal atrophy under WL.
Narrow band imaging is a new technique to improve the visibility of capillaries, veins, and other tissue subtleties by narrowing the bandwidth of spectral transmittance using optical filters. It is a real-time imaging technique. Our opinion about Wood’s light’s success is similar to that behind narrow band imaging [18]. When the vaginal mucosal thickness is thinner with postmenopausal status, illumination with Wood’s light supplies different fluorescence colour due to superficial subepithelial vessels.
Semen could be fluorescence with a WL, and it is not easy to differentiate semen from other common contaminants using a WL [19].
We selected the patients with very strict criteria because any infection, disease, or cervicovaginal smear abnormalities or chronic illnesses, like diabetes mellitus or skin conditions, could make the diagnosis of vaginal atrophy with Wood’s light incorrect. We did not specifically study the effects of chlamydial or other microorganisms that were not isolated with routine cultures.
Limitations
There were some limitations of our study. Because it was a case control study, our findings should be repeated in expanded, randomized studies. In the future, postmenopausal-related vaginal atrophy cases as well as other conditions of oestrogen deficiency should be studied.
Our number of cases were limited, and we selected cases using very strict criteria. Therefore, in future, the number of the cases and groups, such as pregnant women, surgical menopausal patients, or those with chemotherapy-induced vaginal atrophy, should be evaluated in subsequent studies.
Conclusion
Our study’s preliminary findings will be helpful to clinicians. Because the examination is easy to perform and this tool is painless, fast, and free, every gynaecology unit should have a Wood’s light for diagnosing vulvar skin lesions and vaginal atrophy in postmenopausal women. This tool will be helpful to clinicians as an objective test for diagnosing vaginal atrophy. The diagnostic accuracy and cost-effectiveness of WL can be better optimized in further trials.