Surgical Management of Fractured Orthodontic Mini- Implant- A Case Report
Manthan Desai1, Anoop Jain2, Nida Sumra3
1Periodontist and Implantologist, Department of Periodontics,Private Practitioner, Mumbai, India.
2Consultant and Prosthodontist, Dental Xperts-Multispeciality Dental Clinic, Rohini, Delhi, India.
3Post Graduate Student, Department of Periodontics, HKE’S S N Institute of Dental Sciences & Research, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anoop Jain, Consultant and Prosthodontist, Dental Xperts-Multispeciality Dental Clinic, A3/221, First floor, Sector 17, Rohini, Delhi-110089, India.
E-mail: dranoopjn@gmail.com
The idea of absolute anchorage has always been an elusive goal for clinicians. Orthodontic mini-implants or temporary anchorage devices allow tooth movements previously thought to be impossible or difficult. Although extensive literature exists on use of temporary anchorage devices, their failures have been hardly focused upon, especially implant fracture. The following case report describes successful management of fractured orthodontic mini-implant.
Fracture, Mini-implant, Micro-implants, Orthodontics, Temporary anchorage device
Case Report
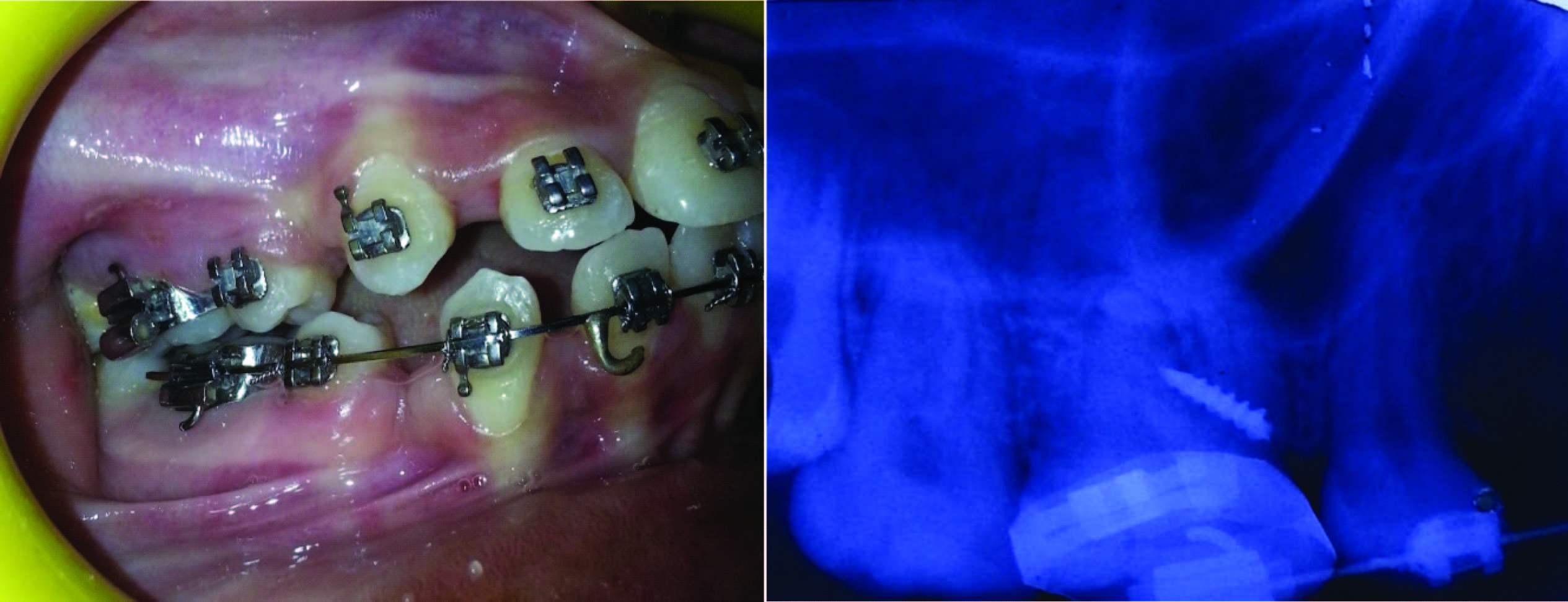
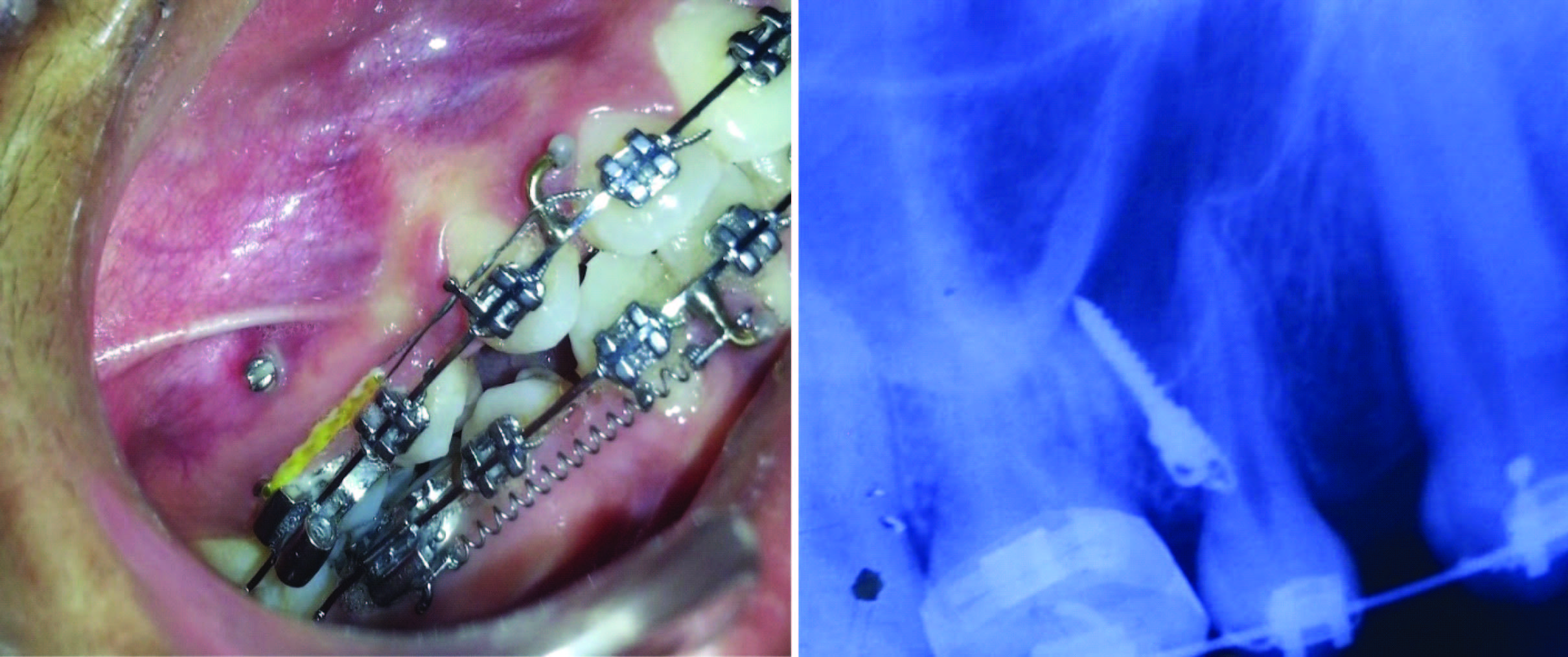
A 19-year-old female patient was referred to the clinic and diagnosed of having bimaxillary protrusion. It was decided to use TAD for retraction, as per the anchorage requirements. A 1.3 x 9 mm stainless steel implant (S.K Surgical, Pune, India) was used. During the placement of the implant in 15 - 16 regions it fractured with 8 mm inside the bone. The probable cause of fracture was thick cortication of bone. A radiograph was taken to determine the exact position of the implant and to gauge its proximity to nearby structures [Table/Fig-1a,b]. It was decided to surgically remove the implant. Written informed consent was obtained from the patient. After obtaining adequate anaesthesia a full thickness flap was reflected in 15-16 regions. The TAD site was identified and located [Table/Fig-2] . 2-3 mm of bone was circumferentially removed around TAD with a carbide bur under copious irrigation. The fractured TAD was held with Howe’s plier and with a “pull-out” motion the TAD was retrieved [Table/Fig-3]. Another TAD of same dimensions was placed slightly above to the first site uneventfully. The surgical defect was grafted with bone graft material (Osseograft, Demineralized Bone Matrix, Advanced Biotech Products Limited, Chennai, India) [Table/Fig-4]. Simple interrupted sutures were placed (5-0 black braided silk, Ethicon, USA). The head of TAD was exposed post suturing [Table/Fig-5]. Postoperative antibiotics and analgesics were prescribed. Suture removal was done after a week following uneventful healing and the implant was loaded for function. Postoperative view at one and half months is shown in [Table/Fig-6a,b].
Discussion
The idea of absolute anchorage is a solution for clinicians who seek to move teeth without unwanted sequel [1] Orthodontic miniimplant or temporary anchorage devices (TAD) when used as either direct or indirect skeletal anchors, can provide absolute anchorage for a multitude of tooth movements. TADs have opened a new vista in orthodontics, allowing tooth movements previously thought to be difficult or impossible. They provide a fixed point for the application of forces to move teeth in the desired position. They can be placed in different positions in the mouth and can be customized as per patient’s need. Clinicians continue to search methods that aid in accomplishing desired treatment objectives without relying on patient compliance. TADs appear to fulfill these objectives [2].
Though helpful, TADs are not without disadvantages. The ease of use of TAD has led to their injudicious use. Some problems associated are inadequate bone for placement, risk of infection, loss of primary or secondary stability, soft tissue impingement, and fracture [3,4]. These problems can be minimized by analyzing implant material, dimensions and bone - soft tissue biology.
Insertion methods of TADs may be categorized as either drill-free or non-drill-free, depending on the thread design. Drill-free feature a cutting tip which does not require that a pilot hole be created before insertion, while non-drill-free designs commonly require a soft-tissue punch and a pilot hole to be drilled in bone before placement. Factors that influence the amount of torque exerted during insertion: bone, quality, pilot hole size, thread design, and insertion methodology [5]. Suzuki et al., concluded that incidence of fracture and torque values were directly proportional [6]. Barros et al., concluded that TADs with diameter less than 1.5 mm are more prone to fracture [7]. Butcher et al., reported an average 4% incidence of fracture while placement of TADs [8]. Mischkowski et al., reported 9.5% incidence of fracture at insertion torques ranging from 52-56 Ncm [9] . A few precautions can be exercised to avoid fracture of TAD - (1) assessment of bone density utilizing radiographs or CBCT scan, which are used for treatment planing, (2) use of pilot drills when tough resistance is experienced during placement, (3) use of torque measuring devices while placement of TAD. Optimal range of torque is 5-10 Ncm, values exceeding 10 Ncm may result in fracture of TAD [10]. Once the TAD fractures, there are only limited options at hand. The decision whether or not to retrieve the fractured TAD depends on site and location of the fracture and patients consent. Periodic evaluation is needed when it is decided not to retrieve the TAD. If the TAD stump is visible, a slot can be prepared to engage a screw driver and unscrew it. And if it is not visible, a carbide or trephine bur to facilitate the removal surgically. Trephine burs may remove excessive amount of bone or damage neighboring structures. Circumferential bone removal around the TAD with a carbide bur is a more conservative alternative, as described in the case report.
Pre-operative view (a) Intraoral (b) Radiograph
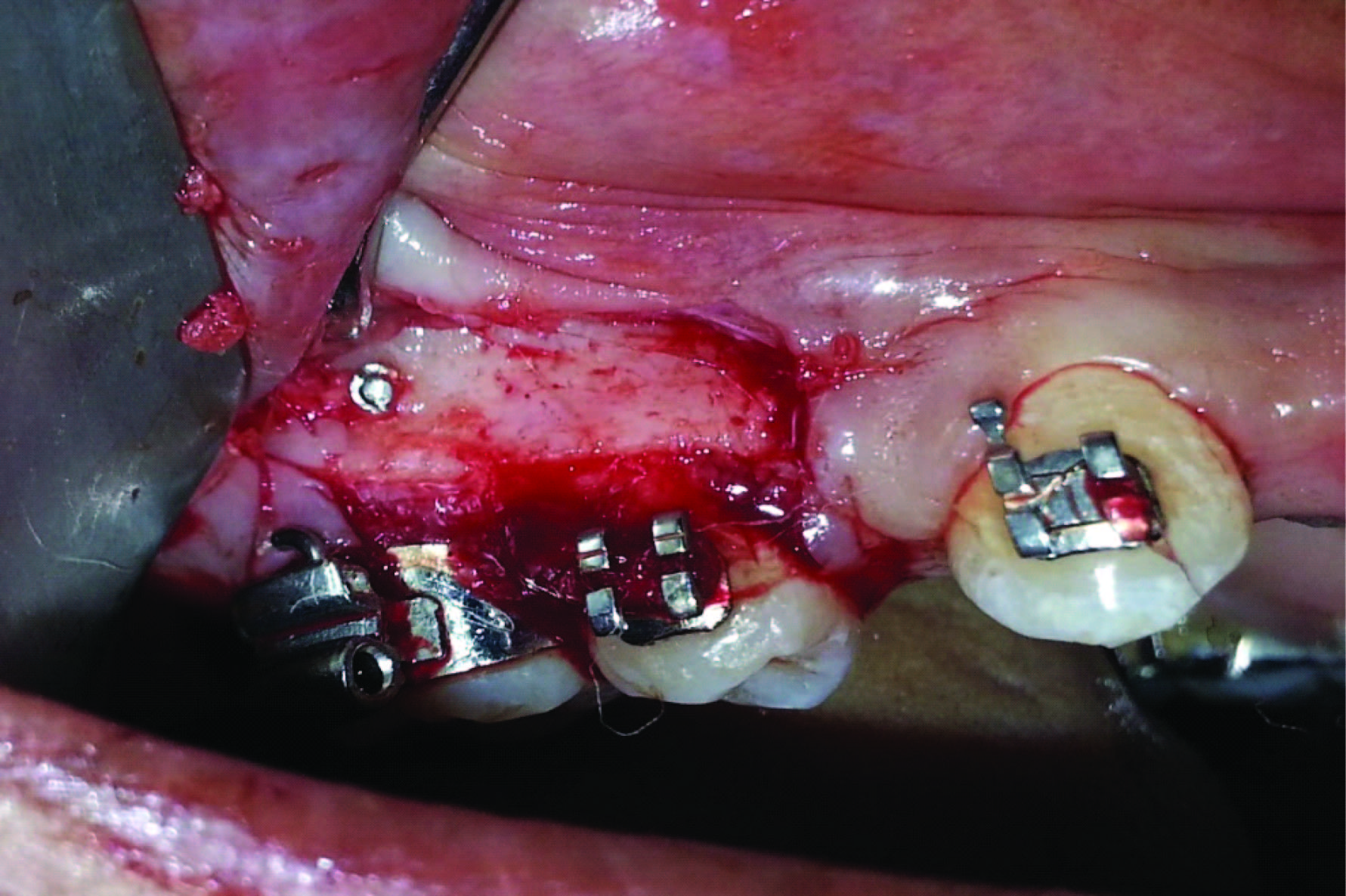
(a) TAD held by howe's piler (b) Retrieved fractured TAD

Bone graft placement and placement of second TAD


Postoperative view (a) Intraoral (b) Radiograph
Conclusion
There exists extensive literature on TADs but their failures, especially fracture has been rarely focused upon. There are only a few documented case reports on it. The following case report describes successful management of TAD fracture. TAD fractures although is a rare clinical possibility and has to be managed wisely. A sound knowledge of biological and mechanical aspects of TADs would be instrumental in avoiding complications.
[1]. TD Creekmore, MK Eklund, The possibility of skeletal anchorageJ Clin Orthod 1983 17(4):266-69. [Google Scholar]
[2]. S Baumgaertel, MR Razavi, MG Hans, Mini-implant anchorage for the orthodontic practitionerAm J Orthod Dentofacial Orthop 2008 133(4):621-27. [Google Scholar]
[3]. HS Park, SH Jeong, OW Kwon, Factors affecting the clinical success of screw implants used as orthodontic anchorageAm J Orthod Dentofacial Orthop 2006 130(1):18-25. [Google Scholar]
[4]. SJ Cheng, IY Tseng, JJ Lee, SH Kok, A prospective study of the risk factors associated with failure of mini-implants used for orthodontic anchorageInt J Oral Maxillofac Implants 2004 19(1):100-06. [Google Scholar]
[5]. RH Ansell, JT Scales, A study of some factors which affect the strength of screws and their insertion and holding power in boneJ Biomech 1968 1(4):279-302. [Google Scholar]
[6]. EY Suzuki, B Suzuki, Placement and removal torque values of orthodontic miniscrew implantsAm J Orthod Dentofacial Orthop 2011 139(5):669-78. [Google Scholar]
[7]. SE Barros, G Janson, K Chiqueto, DG Garib, M Janson, Effect of mini-implant diameter on fracture risk and self-drilling efficacyAm J Orthod Dentofacial Orthop 2011 140(4):e181-92. [Google Scholar]
[8]. A Büchter, D Wiechmann, S Koerdt, Load-related implant reaction of miniimplants used for orthodontic anchorageClin Oral Implants Res 2005 16(4):473-79. [Google Scholar]
[9]. RA Mischkowski, P Kneuertz, B Florvaag, F Lazar, J Koebke, JE Zöller, Biomechanical comparison of four different miniscrew types for skeletal anchorage in the mandibulo-maxillary areaInt J Oral and Maxillofac Surg 2008 37(10):948-54. [Google Scholar]
[10]. M Motoyoshi, M Hirabayashi, M Uemura, N Shimizu, Recommended placement torque when tightening an orthodontic mini-implantClin Oral Implants Res 2006 17(1):109-14. [Google Scholar]