Transvaginal Small Bowel Evisceration in Known Case of Uterine Prolapse Due to Trauma
Umesh Gheewala1, Abhishek Agrawal2, Radha Shukla3, Ravi Bhatt4, Shirish Srivastava5
1Assistant Professor, Department of Surgery, Shree Krishna Hospital, Karamsad, India.
2Resident, Department of Surgery, Pramukhswami Medical College, Shree Krishna Hospital, Karamsad, India.
3Student,Pramukhswami Medical College, Karamsad, India.
4Student,Pramukhswami Medical College, Karamsad, India.
5Professor and Head, Department of Surgery, Shree Krishna Hospital, Karamsad, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Abhishek Agrawal, 14-PG Doctor's Hostel, Shree Krishna Hospital, Pramukswami Medical College, Gokal Nagar, Karamsad, Gujarat-388325, India.
E-mail: Abhishekagrawal2007@gmail.com
Spontaneous transvaginal bowel evisceration is a rare surgical emergency with only a few cases reported and particularly postmenopausal, posthysterectomy, multiparous elderly women are considered to be at higher risk for development of bowel evisceration. It is difficult to manage such a patient for any surgeon and poses significant challenges especially intraoperatively. Here, we report a case of vaginal vault rupture with small bowel evisceration through the vagina in a known case of uterine prolapse and highlight the risk factors, clinical presentation, and treatment options for this rare surgical emergency
Intestinal herniation, Multiparaous, Postmenopausal, Trauma, Uterine prolapse
Case Report
A 60-year-old postmenopasual female, with obstretic history of four full term vaginal deliveries, presented to emergency care with history of fall from chair at home causing perineal trauma, bleeding per vagina, with evisceration of bowel per vagina associated with transient loss of consciousness. Three months prior to this, she had presented with persistent cough for one year and grade three uterine prolapse for which she refused treatment due to financial constraints.
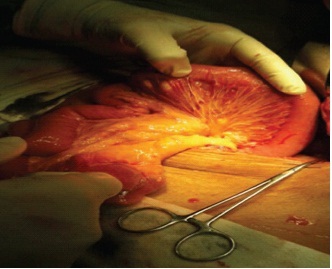
On examination, she was found to be vitally unstable, with irregular pulse of 54 beats/min, blood pressure of 220/120 mmHg and an abdominal examination indicated significant tenderness in lower abdomen and absent bowel sounds. Pelvic examination revealed 40-50 cm of small bowel including caecum and appendix prolapsing through her vagina along with associated uterine prolapse [Table/Fig-1]. Per vaginal examination revealed rent in Pouch of Douglas. After fluid resuscitation, she received intravenous broad-spectrum antibiotics (Piperacillin, Tazobactam and Metronidazole), and her bowel was wrapped with warm, sterile, saline-soaked padsand transfered to the operating room. Postanaesthesia, the eviscerated bowel was assessed and was found to be oedematous, thick walled yet viable with no evidence of necrosis and thus attempts were then made to reduce the bowel transvaginally into the peritoneal cavity which failed. Consequently, a lower midline vertical incision was made, suprapubic catheterization was done and after assessing the damage, the prolapsed bowel was reduced into the abdomen. A 5 cm mesenteric tear was found in the ileum [Table/Fig-2], 10cms proximal to the ileo-caecal junction plus a 7 cm vertical tear was found on the posterior surface of uterus extending from Pouch of Douglas, 2cms medial to the uterosacral ligament along with multiple superficial tears over the fundic part of the uterus and two vaginal tears [Table/Fig-3], all of which were sutured. Postoperatively, due to persistent high blood pressure, she was kept under close observation for one week along with antihypertensive treatment and was discharged on 15th postoperative day. On discharge she was vitally stable with no complaints and was advised for regular follow up for hypertension.
Discussion
Transvaginal bowel evisceration occurring spontaneously is a rare event in itself, has very little mention in literature. However, its reporting dates back to the 19th century, when Hyernaux described a disruption of the anterior wall of the proximal vagina, resulting in prolapse of abdominal contents [1]. Later McGregor, further went on to describe protrusion of small bowel through vaginal wall rupture [2].
Vaginal evisceration has been reported to occur after vaginal traumas induced by coitus, obstetric instrumentation, and the insertion of foreign bodies and direct trauma or after pelvic surgery and in patients with enterocele [3]. The risk groups for transvaginal small bowel evisceration include the elderly; postmenopausal women [4,5], Female patients after vaginal, abdominal or laparoscopic hysterectomy [6]; and multiparous women [1]. Due to weakening of vaginal tissue caused by genital atrophy and enterocele, the risk of spontaneous evisceration is increased in postmenopausal women, particularly in combination with straining at stool and/or vaginal ulceration. The postmenopausal vagina is thin, scarred, foreshortened, and has diminished vascularity, it is more prone to rupture [7,8]. In postmenopausal women, vaginal ruptures most commonly occur at the posterior fornix and either spontaneously or, more frequently, in connection with an increase in intra-abdominal pressure induced by coughing, defecating, or falling [9] or as a result of vaginal ulceration due to severe atrophy and forceful defecation [3,10].
In premenopausal patients, evisceration is usually preceded by vaginal trauma caused by rape, coitus, obstetric instrumentation, or the insertion of foreign bodies [11]. According to Kowalski et al., [6], 73% of patients with vaginal evisceration had previously undergone some kind of vaginal surgery, most commonly transvaginal hysterectomies or enterocele repairs. In 63% of the reported cases, the patients had enteroceles, which putatively caused further stretching of the atrophic vagina, thus making it more susceptible to rupture. Majority of all the vaginal evisceration reported to date, 50– 75% of the patients had undergone one or more previous vaginal operations and roughly 25% of the eviscerations occurred after abdominal hysterectomy [6].
In the present case, one of the probable underlying causes of the evisceration was the fact the patient was postmenopausal multigravida female, contributing to a weak pelvic floor leading to vaginal rupture. Associated cause can also be attributed to persistent cough for one year. However, the main trigger factor is trauma to the perineum, leading to sudden increase in abdominal pressure and inability of the weakened pelvic floor to offer resistance.
Vaginal evisceration is a surgical emergency, and immediate recognition and surgical repair are crucial for its successful management. The appropriate management of evisceration includes a thorough assessment of the herniated viscus and surgical repair of the vaginal defect. In cases where the eviscerated bowel is viable and can be reduced into the peritoneal cavity without complication, the closure of the vaginal defect can be accomplished by a vaginal approach however, in patients with minimal or no enterocele, the vaginal defect may be located high in the vagina, as was the case in the present study. Under these circumstances, a vaginal approach is not viable because the bowel, which becomes trapped and strangulated after protruding through the defect, prevents access to the defect itself. In these cases, laparotomy is necessary to access the defect, reduce the bowel into the abdomen, and resect any nonviable bowel. A combined abdominal and vaginal surgical approach, as the one used in the present case report, is recommended for adequate evaluation and effective repair of the tissues involved.
Eviscerated small bowel per vaginum

Two vaginal tears repaired

Conclusion
It can be concluded that transvaginal small bowel evisceration despite being rare, is common among grand multipara during their post menopausal stage with an aditional risk in those with known history of uterine prolapse. Further, the situation would be aggravated by those conditions leading to an increase in intraabdominal pressure. Thus a thorough clinical evaluation, detailed history in addition to abdominal and vaginal surgical approaches is essential in management of such patients.
[1]. P Gandhi, S Jha, Vaginal vault eviscerationThe Obstetrician & Gynaecologist 2011 13:231-37. [Google Scholar]
[2]. AN McGregor, Rupture of the vaginal wall with protrusion of small intestine in woman of 63years of ageBritish Journal of Gynecology 2005 11:252-58. [Google Scholar]
[3]. MD Moen, M Desai, R Sulkowski, Vaginal evisceration managed by transvaginal bowel resection and vaginal repairInternational Urogynecology Journal 2003 14:218-20. [Google Scholar]
[4]. PT Ramirez, DP Klemer, Vaginal evisceration after hysterectomy: A literature reviewObstetrical and Gynecological Survey 2002 57:462-67. [Google Scholar]
[5]. LM O’Brien, LS Bellin, GA Isenberg, SD Goldstein, Spontaneous transvaginal small-bowel evisceration after perineal proctectomy: Report of a case and review of the literatureDiseases of the Colon and Rectum 2002 45:698-99. [Google Scholar]
[6]. LD Kowalski, JC Seski, PF Timmins, AI Kanbour, AJ Kunschner, A Kanbour-Shakir, Vaginal evisceration: Presentation and management in postmenopausal womenJournal of the American College of Surgeons 1996 183:225-29. [Google Scholar]
[7]. S Rajesh, E Kalu, J Bong, N Wales, Evisceration 5 years post abdominal hysterectomyJournal of Obstetrics and Gynaecology Research 2008 34:425-27. [Google Scholar]
[8]. K Yuce, P Dursun, M Gultekin, Post hysterectomy intestinal prolapse after coitus and vaginal repairArchives of Gynecology and Obstetrics 2005 272(1):80-81. [Google Scholar]
[9]. S Chabbra, P Hegde, Spontaneous transvaginal bowel eviscerationIndian Journal of Urology 2013 29(2):139-41. [Google Scholar]
[10]. B Feiner, A Lissak, R Kedar, O Lefel, O Lavie, Vaginal evisceration long after vaginal hysterectomyAmerican College of Obstetricians and Gynecologists 2003 101:1058-09. [Google Scholar]
[11]. N Gujar, Coitus induced vaginal evisceration in a premenopausal woman: a case reportPatient Safety in Surgery 2011 5:6 [Google Scholar]