Histogenesis and Clinical Analysis of 2 Cases of Congenital Gingival Granular Cell Tumour
Karla Mayra Rezende1, Fernanda Nahás Pires Côrrea2, José Paulo Nahás Pires Côrrea3, Maria Salete Nahás Pires Côrrea4, Marcelo Bönecker5
1Ph.D Student, Department of Pediatric Dentistry, University of São Paulo, São Paulo, Brazil.
2Professor, Department of Pediatric Dentistry, Faculdade São Leopold Mandic Campinas, São Paulo, Brazil.
3Surgeon, Department of Pediatric Dentistry, Private Office, São Paulo, Brazil.
4Professors, Department of Pediatric Dentistry, School of Dentistry, Universidade de São Paulo, São Paulo, Brazil.
5Professors, Department of Pediatric Dentistry, School of Dentistry, Universidade de São Paulo, São Paulo, Brazil.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Karla Mayra Rezende Ph.D Student, Department of Pediatric Dentistry, University of São Paulo Professor Lineu Prestes, 2227, Zip code: 05508-000 São Paulo, SP, Brazil.
E-mail: karla.rezende@usp.br
Dentistry for babies aims to contribute to the formation of a generation with fewer dental problems, higher quality of oral health and more aware of the importance of prevention. The congenital gingival granular cell tumour (CGCT) is a rare benign soft tissue tumour in the newborn that can lead to respiratory difficulties and feeding. The aim of this work was to report two cases of CGCT in babies and discuss the clinical and histological differential diagnosis and their treatment, as well as the importance of knowledge of this pathology for dentists. Clinical features and treatment approaches are presented and discussed. The surgical approach improved the child quality of life and restored the parent’s confidence and emotional stability. Knowledge of this pathology helps in better diagnosis and treatment, which lead to a better quality of life of children and return confidence and emotional stability to parents.
Congenital epulis, Newborn, Pedunculated mass
Case Report
Consent forms for examination and authorization of images disclosure for scientific publication were properly signed by the legal guardian of the child, according to protocols of the 1996 resolution of the National Health Council of the Ministry of Health (Brazil).
Case 1
A 3-day-old of life Caucasian girl was brought by her parents to the Paediatric Dentistry Clinic, School of Dentistry, University of São Paulo, Brazil. The chief complaint for seeking dental care, was that the girl was born with a growth in the anterior maxillary alveolus, as well as the worry of parents concerning the breastfeeding.
The baby had normal antenatal scans during the pregnancy and the baby was born at term and weighing 3.85kg. Mother was fit with no drug history or family history of note.
On intra oral examination, the patient presented a pedunculated solid growth of one-centimeter diameter, pink coloured, smooth surface, lobulated with a narrow stalk and located on the front edge of the maxilla, in the region of the right lateral incisor, without infiltration to adjacent structures and no other changes [Table/Fig-1]. No difficulty in breathing or other structural deformities were present, though there was in breastfeeding. On palpation it was firm, not compressible or reducible and non-tender. A diagnostic biopsy was proposed and the lesion was totally removed under local anaesthesia. The mass was removed with an eliptical incision to the peduncles. Hemostasis was with gauze. There was minimal blood loss. Postoperative recovery was uneventful. There had not been any additional treatment. The material was immediately taken for histopathological examination which confirmed this pathology.
Case 2
A one-month-old female child who was a product of normal fullterm pregnancy was brought by her mother for evaluation of a mass protruding from her mouth, which was causing feeding difficulties, but no airway obstruction. Intraoral examination revealed a pedunculated mass, with color similar to the adjacent mucosa, arising from the anterior jaw alveolar ridge. Measuring approximately 08 x07 x 05 mm, it had a smooth and firm surface and was protruding slightly from the mouth [Table/Fig-2]. The mass was surgically excised under local anaesthesia using 2% Xylocaine. The blood loss was minimal and the specimen was fixed in 10% neutral buffered formalin and processed for histopathological examination. No recurrence was seen.
Histological characteristics of CGCT
Light microscopy examination in both cases revealed a mass of connective tissue covered with mildly acanthotic squamous epithelium and showed closely packed polygonal cells with centrally placed nuclei and markedly granular cytoplasm. No cross striations were seen, while numerous blood vessels were present. These histopathological features confirmed the diagnosis of congenital epulis [Table/Fig-3a-d].
Discussion
Tumours of the oral cavity are not common among newborns. Congenital gingival granular cell tumour (GGCT) characteristically occurs as a solitary mass on the anterior alveolus of newborns. The cytogenesis and hormonal receptor studies give no clues for female predominance; because of the absence of detectable estrogen and progesterone receptors [1]. This pathology is a unique and rare benign lesion arising from the mucosa of the alveolar ridges of the jaws present at birth, although it has been also described as arising from the mandibular gingiva as well as from several locations simultaneously. Lesions may be sessile or pedunculated, normally colored or reddish, varying in size from several millimeters to a few centimeters and they are typically seen protruding from the neonate mouth [2,3]. In our cases described here, the tumours had a firm consistency and were pedunculated. As noted in the literature, the two presented cases occur in female children, perhaps implicating a hormonal component to their genesis [2,4-6].
Large lesion can interfere with fetal deglutition resulting in hydramnios and respiratory obstruction, difficulty in feeding postnatally. As the size of the lesion in both cases, were relatively small but causing breastfeeding problems. Studies show that the lesion appears to stop growing and there have been no documented recurrences, even with incomplete excision, and no reports of malignant transformation [7,8]. The literature does not recommend surgical excision, because they say that small lesions tend to regress and disappear spontaneously [1], which was not observed in these two breastfeeding-cases. Other authors recommend the surgical procedure so that the lesion is observed but limited only to the injury [5,9]. However, the treatment of our choice is surgical excision mostly to reassure parents. In both cases the tumour were pedunculated mass and easily excised without difficulty, and even after total resection, neither the recurrence nor malignancy has been reported.
The exact nature of this entity is not clear. Once thought to be a form of odontogenic dysgenesis, it is now thought to originate from primitive mesenchymal cells of neural crest origin, although the evidence for this is less than conclusive [1,10]. It has been suggested that the CGCT is merely a stage in the development of the tooth germ but the finding of occasional epithelial, ameloblastlike, cells among the granular cells does not constitute proof of this contention, since epithelial residues are rampant in all gingival tissues [11]. Different studies discussed several theories: odontogenic, fibroblastic, hystocytic, myogenic and neurogenic, but the exact aetiology and histogenesis still remain uncertain [1,5,10]. So diagnosis of CGCT is made based on clinical findings and is confirmed by histologic examination. Histological characteristic [Table/Fig-3] shown in this work include revealing fragments of mucosa lined by stratified squamous epithelium parakeratinized laying flat compared with adjacent tissue, and some cells of the basal layer with a more columnar and arranged in palisades. The lamina propria is composed of dense connective tissue and shows proliferation of cells whose cytoplasm is voluminous granulomatous, and hyperchromatic nucleus, rounded. These cells are arranged in a large sheet and looks interspersed with numerous blood vessel. Extensive hemorrhagic area in the periphery. Not found histopathologic the formation of the epithelial islands commonly found in the gum pad of newborns and infants suggests its origin from odontogenic epithelial rests [1] or does not have schwannian origin because this is reflected by its S 100 negativity [12]. Out of several theories, the most widely accepted hypothesis is that of a degenerative process of undifferentiated mesenchymal cells which, in turn, are capable of multiple differentiation [13,14]. The clinical differentials include myoblastoma, teratoma, hemangioma, rhabdomyoma, schwanomma, hibernoma and fibroma [2]. Nowadays, the diagnosis is based on their clinical manifestations and behavior, certain histopathologic features, and immunophenotypic markers.
Sequence of the first clinical case
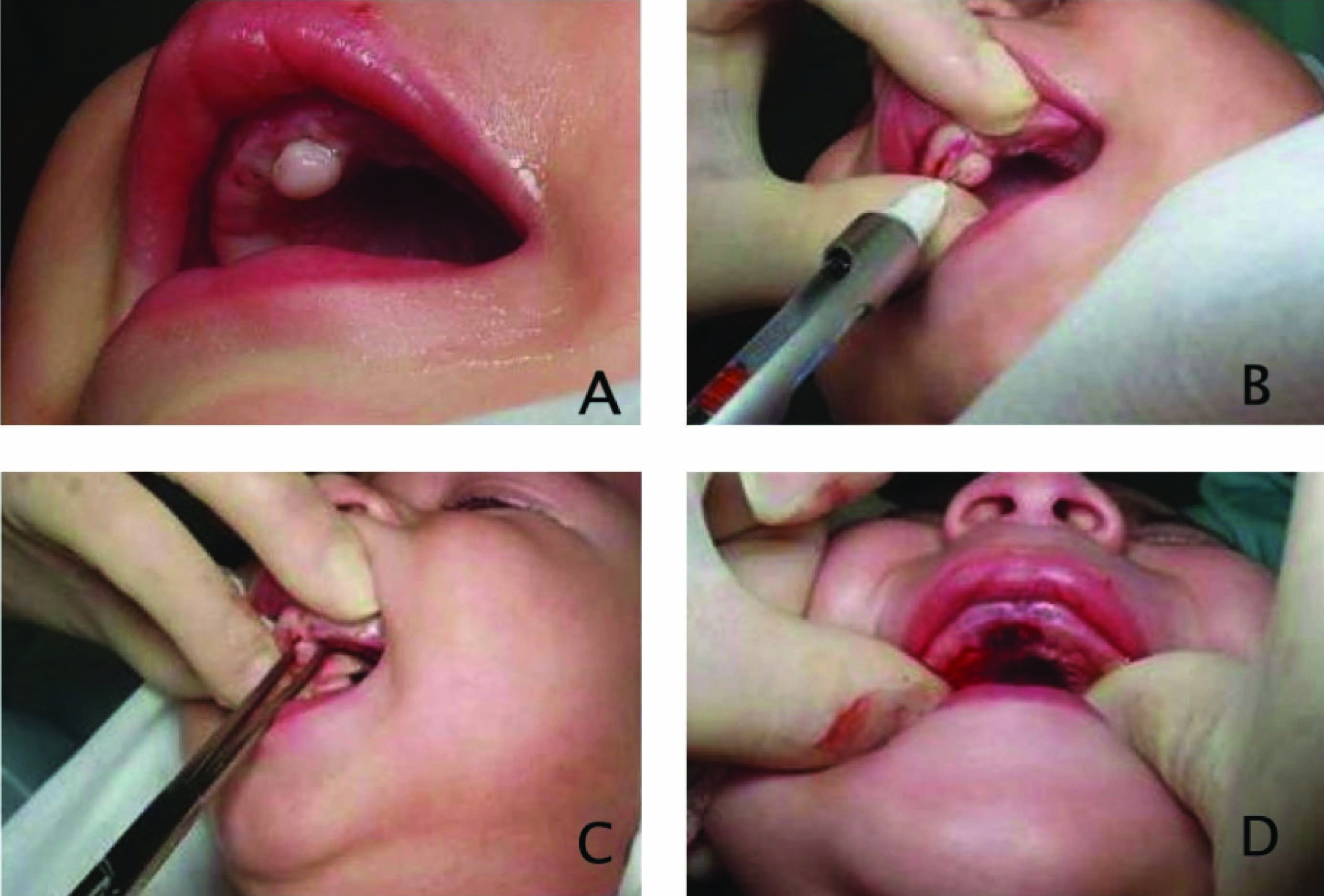
Sequence of the second clinical case
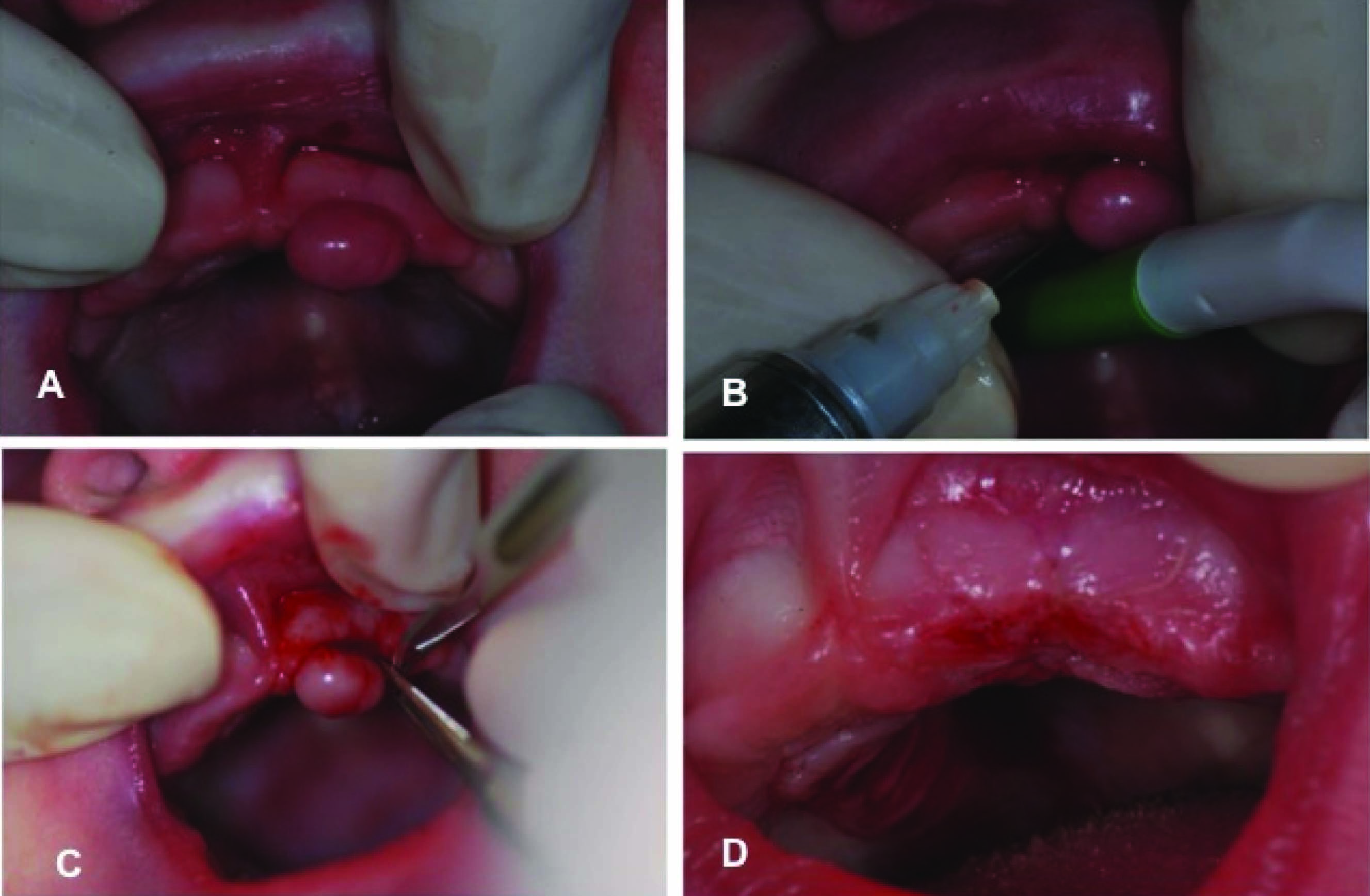
A) Light micrograph showing the oral epithelium covering a highly cellular connective tissue. In A, it may be seen the normal squamous epithelium and below it the tumour, which is composed of polygonal cells with a meshwork of delicate blood vessels (arrows). B) High-power view of rounded and elongated cells with abundant eosinophilic granular cytoplasm and small round nuclei with capillaries (HE X 400). C)&D) the peripheral portion of the mass reveals abundant collagenous connective tissue with numerous vascular channels (HE X 100)

Conclusion
Newborns present some normal oral characteristics, as well as physiological variations, according to their development stage. It is important that Paediatricians and Paediatric dentists have the knowledge about oral characteristics within normal patterns in newborns, and be prepared to realize a correct diagnosis of the anomalies in early stages, in order to avoid unnecessary therapeutic procedures, provide suitable information to the newborn's parents about the nature of these lesions and reassure them on the proper treatment
[1]. JK Dash, PK Sahoo, SN Das, Congenital granular cell lesion "congenital epulis"- -report of a caseJournal of the Indian Society of Pedodontics and Preventive Dentistry 2004 22(2):63-67. [Google Scholar]
[2]. O Lapid, R Shaco-Levy, Y Krieger, L Kachko, A Sagi, Congenital epulisPaediatrics 2001 107(2):E22 [Google Scholar]
[3]. AH Fuhr, PH Krogh, PJ Porter, EH Kass, Congenital epulis of the newborn: centennial review of the literature and a report of caseJ Oral Surg 1972 30(1):30-5. [Google Scholar]
[4]. KS Canavan-Holliday, RA Lawson, Anaesthetic management of the newborn with multiple congenital epulidesBritish journal of anaesthesia 2004 93(5):742-44. [Google Scholar]
[5]. S Guven, A Kaymakci, MS Bugday, M Yilmaz, Congenital granular cell tumour The Journal of craniofacial surgery 2009 20(3):976-77. [Google Scholar]
[6]. SJ Merrett, PJ Crawford, Congenital epulis of the newborn: a case reportInternational journal of paediatric dentistry / the British Paedodontic Society [and] the International Association of Dentistry for Children 2003 13(2):127-29. [Google Scholar]
[7]. KO Bang, AS Bodhade, AM Dive, Congenital granular cell epulis of a newbornDental research journal 2012 9(Suppl 1):S136-38. [Google Scholar]
[8]. M Hiradfar, N Zabolinejad, M Gharavi, S Sebt, Multiple congenital epulis of the mandibular ridge: a case reportIranian journal of otorhinolaryngology 2012 24(69):193-96. [Google Scholar]
[9]. AM Kupers, P Andriessen, MJ van Kempen, IG van der, JA Baart, AG Dumans, Congenital epulis of the jaw: a series of five cases and review of literaturePaediatric surgery international 2009 25(2):207-10. [Google Scholar]
[10]. GC Silva, TC Vieira, JC Vieira, CR Martins, EC Silva, Congenital granular cell tumour (congenital epulis): a lesion of multidisciplinary interestMedicina oral, patologia oral y cirugia bucal 2007 12(6):E428-30. [Google Scholar]
[11]. S Kay, RP Elzay, MA Wilson, Ultrastructural observations on a gingival granular cell tumour (congenital epulis)Cancer 1971 27(3):674-80. [Google Scholar]
[12]. M Dhingra, C Pantola, A Agarwal, Congenital granular cell tumour of the alveolar ridgeIndian journal of pathology & microbiology 2010 53(2):327-28. [Google Scholar]
[13]. EE Lack, AR Perez-Atayde, TJ McGill, GF Vawter, Gingival granular cell tumour of the newborn (congenital "epulis"): ultrastructural observations relating to histogenesisHuman pathology 1982 13(7):686-89. [Google Scholar]
[14]. H Senoo, S Iida, M Kishino, N Namba, T Aikawa, M Kogo, Solitary congenital granular cell lesion of the tongueOral surgery, oral medicine, oral pathology, oral radiology, and endodontics 2007 104(1):e45-8. [Google Scholar]