Gastrointestinal stromal tumours (GISTs) account for less than 3% of all gastrointestinal tract tumours and 5.7% of all sarcomas, and the majority of these tumours are gastric in origin. Patients commonly present with gastrointestinal bleeding or abdominal pain with 10-30% of patients presenting with symptoms of gastrointestinal obstruction. We report a rare case clinically presenting as gastric outlet obstruction, gastroscopy suspecting it to be organo-axial gastric volvulus, CECT(Contrast Enhanced Computerised Tomography) suggesting features of gastric malignancy (leiomyosarcoma) keeping the possibility of differential diagnosis of GIST. Eventually on exploratory laparotomy we discovered gastric outlet obstruction due to transpylorically herniated pedunculated polypoid GIST leading to gastroduodenal inussusception.
Diagnosis, Endoscopy, Gastrointestinal Stromal tumour, Sarcoma
Case Report
A 74-year-old male presented with a history of vomiting, since three weeks. Physical examination revealed a mildly tender abdomen without guarding or rebound tenderness. The patient was dehydrated. No mass was palpated per abdomen.
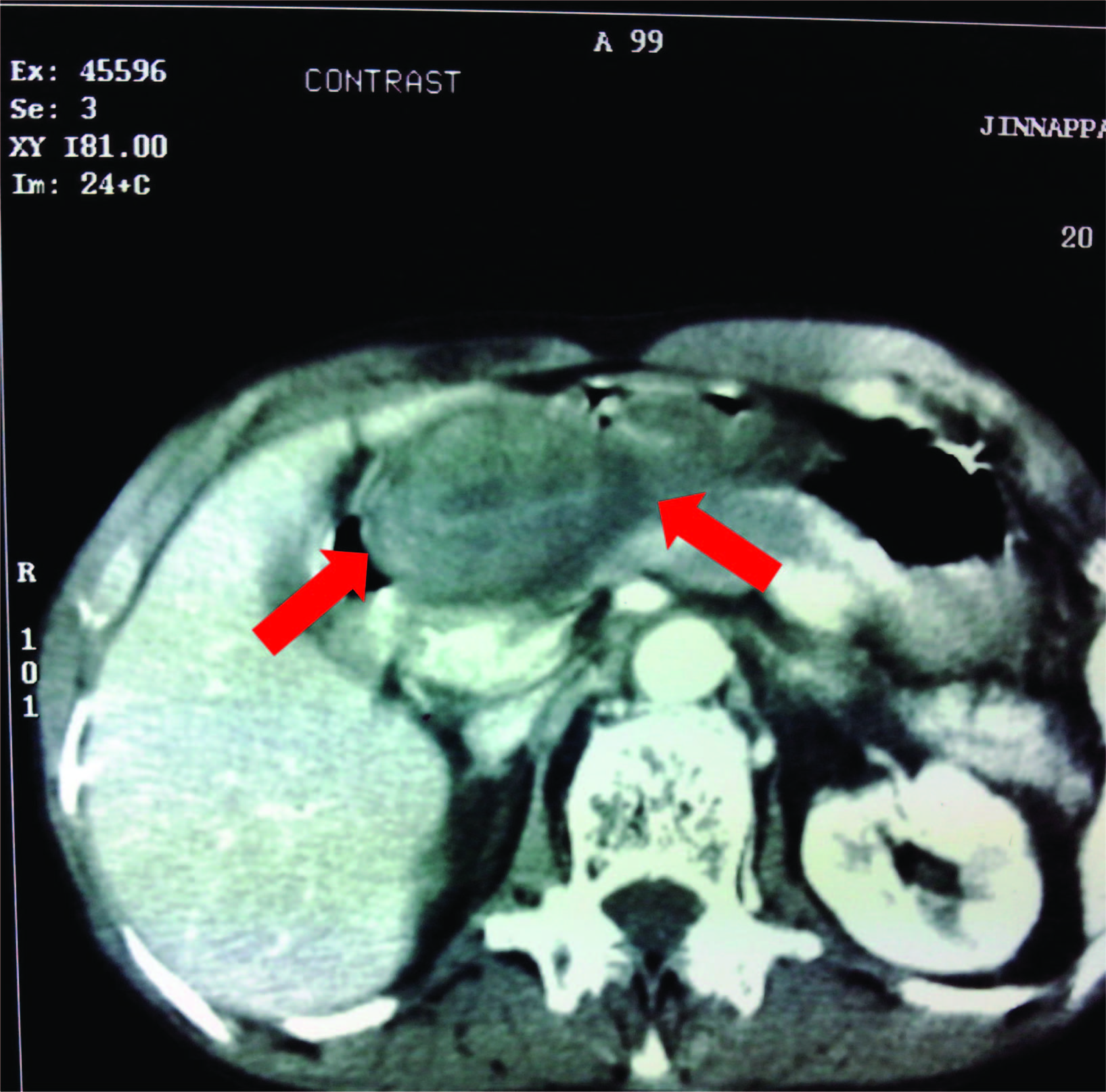
CECT (Contrast Enhanced Computerised Tomography) abdomen revealed a polypoidal lesion at pyloro-duodenal junction growing concentrically along the pylorus, occluding the lumen [Table/Fig-1]. It extended eccentrically along first part of duodenum with anchoring of the mass to pyloro- duodenal junction causing partial organo-axial volvulus which is a possibility of GIST.
Further on upper GI endoscopy, the visualized gastric mucosa was normal, gastric luminal axis was twisted. So the scope could not be negotiated into pylorus/duodenum suggesting Organo axial gastric volvulus [Table/Fig-2a-c]. During laparotomy, a tumour on the posterior wall of the stomach causing intussusception of the stomach into the duodenum was found [Table/Fig-3,4]. After reducing the intussusception, resection of the tumour was performed. The resection would not be possible without intussusception, these operative features were suggestive of GIST. The patient’s postoperative recovery was unremarkable.
Gross specimen of stomach containing mass was shiny with attached fibro-fatty tissue at one surface and the other side was raw area. The cross section of the gross specimen revealed dark brown hemorrhagic area at centre surrounded by pale white area [Table/Fig-5].
Microscopic features showed proliferating spindle cells with oval to elongated nuclei arranged in fascicles [Table/Fig-6]. Areas of Sagari4hyalinization and mitosis were evident. The tumour cells were seen extending into the subserosal area. Sections also showed calcified nodule along with muscle. To conclude with all the above features it was diagnosed as benign gastric GIST (Gastrointestinal stromal tumour).
Discussion
Gastrointestinal stromal tumours (GISTs) are uncommon tumours of the gastrointestinal (GI) tract. GIST is a non-epithelial, mesenchymal tumour first described by Mazur and Clark in 1983. Gastrointestinal stromal tumours (GISTs) account for less than 3% of all gastrointestinal tract tumours and 5.7% of all sarcomas, and the majority of these tumours are gastric in origin [1,2].
These tumours were previously referred to as leiomyomas and leiomyosarcomas, but have recently been re-classified as they arise from undifferentiated stromal fibroblasts rather than mature smooth muscle cells [3,4].
Patients commonly present with gastrointestinal bleeding or abdominal pain with 10-30% of patients presenting with symptoms of gastrointestinal obstruction. This may be acute, as in melena, hematemesis, or chronic insidious bleeding leading to anaemia [5].
Symptoms of these neoplasms range from intermittent epigastric pain to sudden onsets of severe pain with vomiting and shock. A preoperative diagnosis can be difficult and diagnosis cannot be confirmed until surgery [2]. GIST can also cause symptoms secondary to mass effect including satiety, bloating, and abdominal pain [5,6]. Gastroduodenal intussusception of a stromal tumour of the stomach is a very rare cause of duodenal obstruction [7].
The treatment of choice for localised GIST is surgical resection. The present case was also initially diagnosed as organo-axial gastric volvulus by gastroscopy and CECT findings. Further during laparotomy we discovered gastric outlet obstruction due to transpylorically herniated pedunculated polypoid GIST leading to gastroduodenal inussusception.
So the tumour size, location, and mitotic index remain the main variables used in risk stratification systems, which was first developed by the National Institute of health (NIH), the so-called Fletcher’s criteria [2,8].
Revised version of the NIH risk stratification system is done by inclusion of additional prognostic factors, such as non-radical resection (R1) and a tumour rupture that affects adverse outcomes, which was proposed by several investigators; and was later referred to as the modified NIH criteria [9,10].
GISTs normally present a wide clinico-pathological spectrum, from a small incidental nodule to large pedunculated mass. They are usually described as a tan to white, well circumscribed lesions within the walls of the stomach [2].
Microscopically GISTs demonstrate any of the 3 main histological cell types: spindle cell type (most common), epithelioid cell type, and the mixed (spindle-epithelioid) type [2,6,8,11] The present case showed the most common spindle cell type variant with some hyalinised areas.
The literature suggests immunostaining to differentiate between spindle cells and epitheloid cells. So, the most commonly applied markers are CD 117, CD 34, SMA and S-100 [2].
Greater than 95% of GISTs are positive for CD117 but are no longer considered as an absolute requirement [8,11]. Commonly expressed but less GISTs specific antigens are CD34, nestin, smooth muscle actin (SMA), caldesmon, calponin, vimentin, and embryonic smooth muscle myosin. GISTs are generally negative or weakly positive for desmin [8].
S100 positivity is rare but relatively more common in small intestinal GISTs than gastric GISTs [2,11]. In the present case Immunohistochemistry was not required as the laparotomy and microscopic features were confirmative of the diagnosis.
CECT showing polypoidal lesion in pyloroduodenal junction narrowing the lumen with intraluminal infiltration
Endoscopic view revealing normal appearing gastric mucosa with organo-axial twisting of stomach, (a) Gastric fundus and corpus, (b) Proximal gastric corpus, (c) Site of gastric volvulus

Gastro duodenal intussusceptions
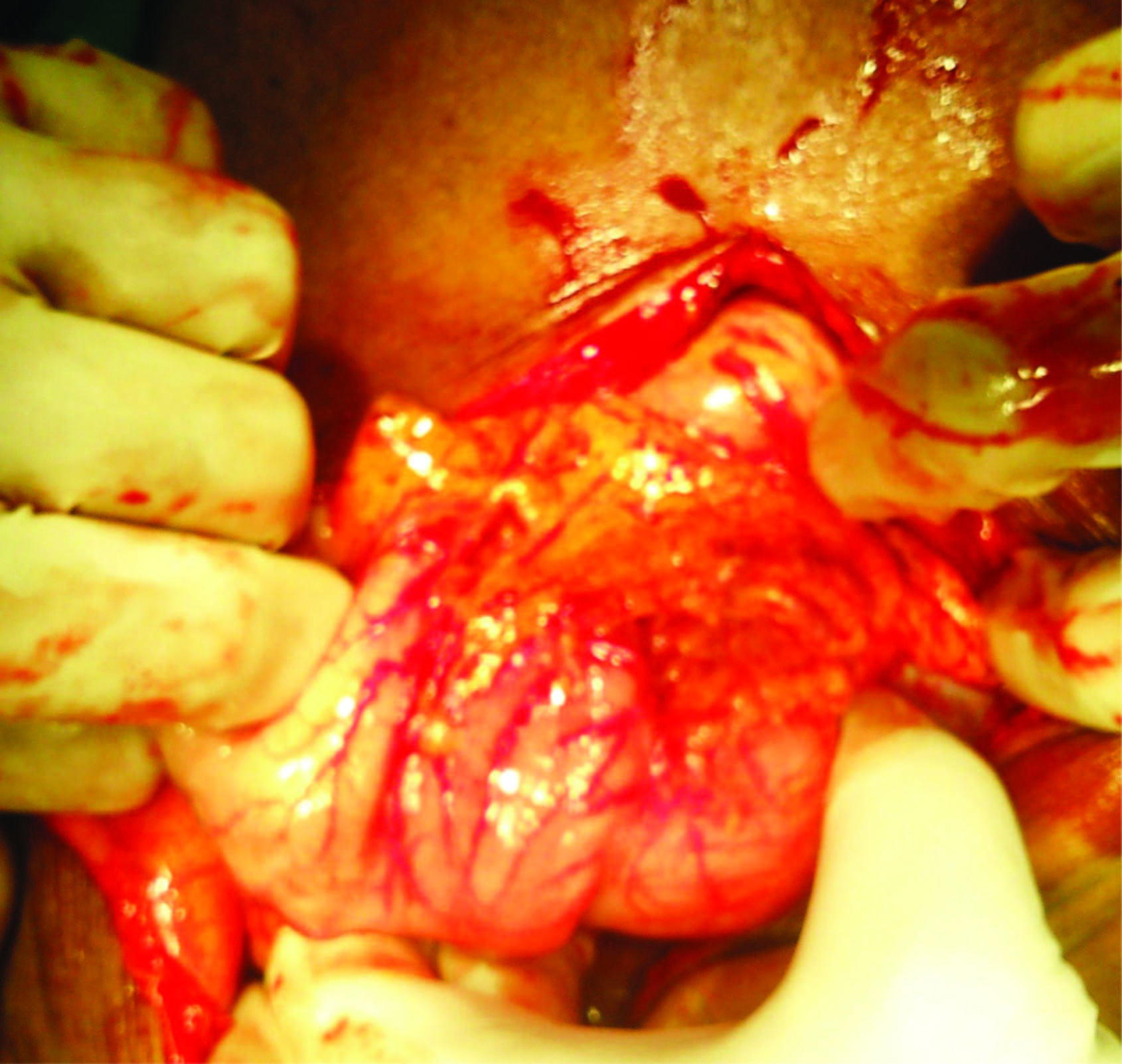
GIST arising from posterior wall of stomach

Gross specimen revealed dark brown hemorrhagic area at centre surrounded by pale white area

H&E section showing proliferating spindle cells with oval to elongated nuclei arranged in fascicles

Conclusion
Although gastroduodenal intussusception, particularly secondary to a GIST, is uncommon, clinicians need to have a high index of suspicion in acutely vomiting patients, especially if they had experienced similar symptoms intermittently in the immediate past
Improvement in surgical techniques has decreased the incidence of tumour recurrence from tumour seeding. Postoperative chemotherapy has also shown to improve relapse-free survival (RFS) but not overall survival (OS) and needs further studies in predicting prognosis and treatment outcome
[1]. CB Tan, W Zhi, G Shahzad, P Mustacchia, Gastrointestinal stromal tumours: a review of case reports, diagnosis, treatment, and future directionsISRN Gastroenterology 2012 2012:595968 [Google Scholar]
[2]. DT Patil, BP Rubin, Gastrointestinal stromal tumour. advances in diagnosis and managementArchives of Pathology and Laboratory Medicine 2011 135(10):1298-310. [Google Scholar]
[3]. H Appelman, Smooth muscle tumours of the gastrointestinal tract. What we know now that Stout didn’t knowAm J Surg Pathol 1986 10(1):83-94. [Google Scholar]
[4]. M Van de Rijn, MR Hendrickson, RV Rouse, CD 34 expression by gastrointestinal tract stromal tumoursHum Pathol 1994 25(1):766-71. [Google Scholar]
[5]. JA Laurini, JE Carter, Gastrointestinal stromal tumours: a review of the literatureArchives of Pathology and Laboratory Medicine 2010 134(1):134-41. [Google Scholar]
[6]. R Laperouse, Raines D, Diamond K, Gastrointestinal stromal tumours: a case report and review of the literatureThe Journal of the Louisiana State Medical Society 2008 160(1):128-34. [Google Scholar]
[7]. KS Crowther, Jacob G, Wyld L, Yamani Q, Gastroduodenal intussusception of a gastrointestinal stromal tumourThe British Journal of Radiology 2002 75:987-89. [Google Scholar]
[8]. GD Demetri, M von Mehren, CR Antonescu, NCCN task force report: Update on the management of patients with gastrointestinal stromal tumoursJNCCN Journal of the National Comprehensive Cancer Network 2010 8(2):S1-44. [Google Scholar]
[9]. A Agaimy, Gastrointestinal stromal tumours (GIST) from risk stratification systems to the new TNM proposal: more questions than answers? A review emphasizing the need for a standardized GIST reportingInternational Journal of Clinical and Experimental Pathology 2010 3(5):461-71. [Google Scholar]
[10]. P Rutkowski, ZI Nowecki, W Michej, Risk criteria andprognostic factors for predicting recurrences after resectionof primary gastrointestinal stromal tumourAnnals of Surgical Oncology 2007 14(7):2018-27. [Google Scholar]
[11]. M Miettinen, J Lasota, Gastrointestinal stromal tumours: review on morphology, molecular pathology, prognosis, and differential diagnosisArchives of Pathology and Laboratory Medicine 2006 130(10):1466-78. [Google Scholar]