Idiopathic Eosinophilic Synovitis of the Knee Joint with Peripheral Eosinophilia – A Rare Case Report
Niranjanan Raghavn Muralidharagopalan1, Volga Harikrishnan2, Sivasubramanian Subbaiah3, Chitra Srinivasan4
1 Assistant Professor, Department of Orthopaedic Surgery, Saveetha Medical College, Thandalam, Chennai, India.
2 Assistant Professor, Department of Pathology, Saveetha Medical College, Thandalam, Chennai, India.
3 Professor & Head, Department of Orthopaedic Surgery, Saveetha Medical College, Thandalam, Chennai, India.
4 Professor & Head, Department of Pathology, Saveetha Medical College, Thandalam, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Niranjanan Raghavn Muralidharagopalan, Flat Number 1, Durbar Apartments, Plot number 56, MMTC Colony, Nanganallur, Chennai, Tamil Nadu-600061, India. Phone : +91-9965518810, E-mail : nir.rag@gmail.com
Synovitis, presenting as a synovial effusion is common. The most common cause include tuberculosis, osteoarthritis. Here with, presenting a rare case of monoarticular synovitis with synovial fluid and peripheral blood eosinophilia of unknown aetiology in an 18-year-old male. We review the clinical and pathological features and impress the need for synovial fluid examination in all cases.
Diethyl carbamazine, Eosinophilic synovitis, Synovial effusion
Case Report
An 18-year-old male, student by profession, presented to us with a history of knee pain and swelling over the right knee joint for a period of 6 wk. Prior to presentation patient had visited a general practitioner who had prescribed NSAIDs for a period of 3 wk.
Patient had no history of trauma, any constitutional symptoms such as fever/loss of weight/loss of appetite, no history of cough with expectoration, no history of gastrointestinal symptoms such as diarrhoea/dysentery, no history of similar illnesses in the family, no history of similar episodes in the past.
Physical Examination
Patient was conscious comfortable and afebrile with normal vital parameters. Detailed examination of the cardiovascular, respiratory and gastrointestinal systems did not detect any abnormality.
Examination of Right knee joint revealed a diffuse swelling which was not warm. Minimal joint line tenderness was present. Patellar tap was elicited and the skin over the joint appeared normal [Table/Fig-1]. Assessment of range of movements showed a restriction in the terminal range and no deformities were observed.
Swelling of the right knee joint

Investigations
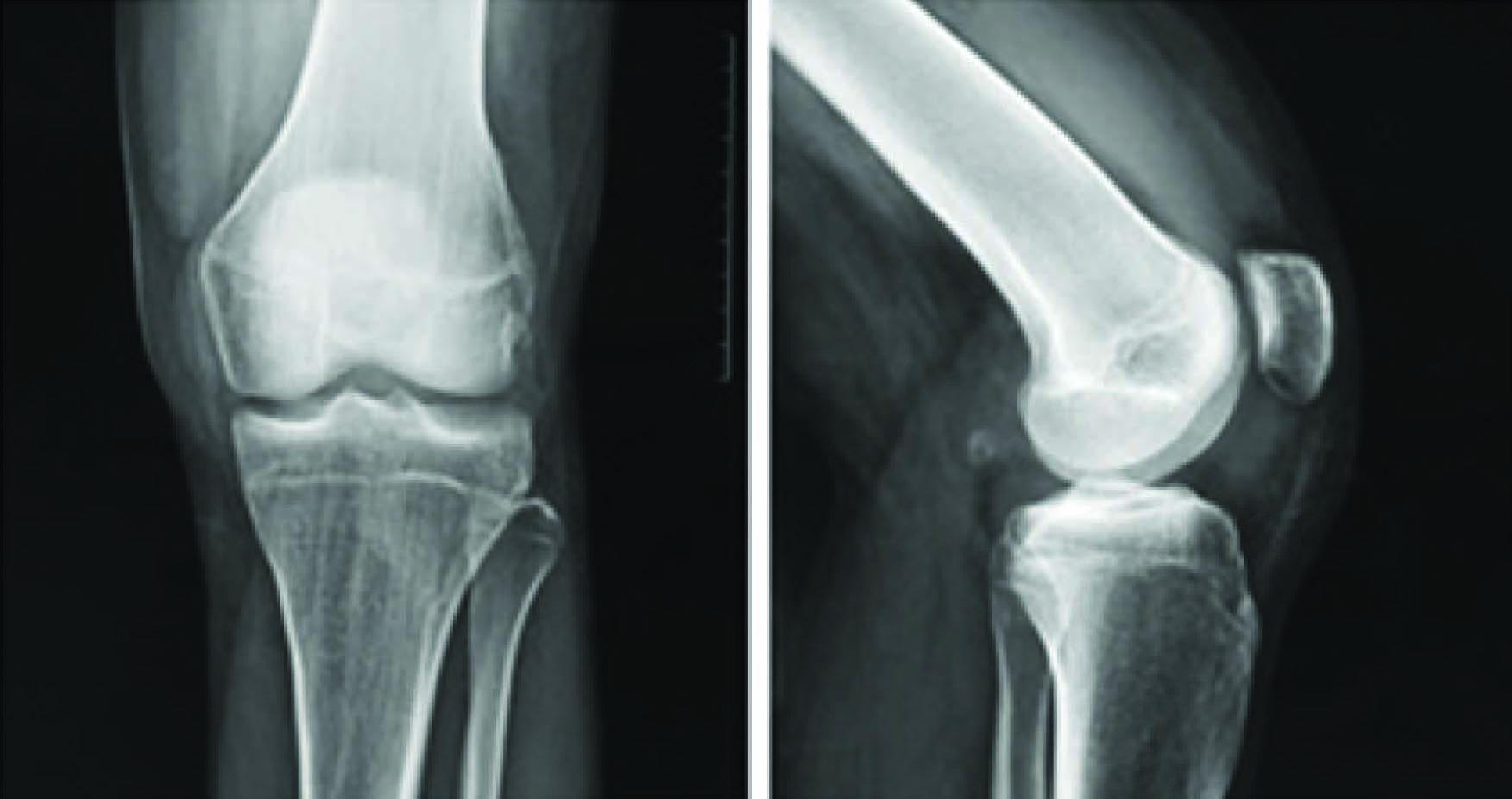
We admitted the patient, performed an x-ray of both the knees [Table/Fig-2a,b] and a chest x-ray presuming a provisional diagnosis of tuberculous synovitis of the right knee. Investigations such as Complete blood count, ESR, Peripheral smear, Mantoux test were done.
Plain X-ray showing synovial effusion
Under sterile aseptic precautions we aspirated 20 ml of synovial fluid which was dark yellow colour [Table/Fig-3] and the fluid sent for analysis.
Synovial fluid aspirate – dark yellow in colour
With above clinical history and investigation results a diagnosis of eosinophilic synovitis with peripheral eosinophilia was made.
Further tests such as stool examination, ultrasound abdomen were carried out to identify the cause of the eosinophilia. However all tests came out negative [Table/Fig-4,5,6].
| Test Mantoux test | Result Negative |
|---|
| Complete Blood Count | Total Count : 6000 cells/cu mm Differential count : Neutrophils: 40% Lymphocytes: 43% Monocytes: 5% Eosinophils: 12% ([Table/Fig-5] Leishman stain (40X); Smear shows predominantly of eosinophils. No RBCs seen in the background.) Haemoglobin: 10g% |
| Peripheral smear | Microcytic hypochromic anaemia with eosinophilia No blood parasites seen. |
| Erythrocyte sedimentation rate C-reactive protein RA factor | 12mm/hr 4.6mg% Negative |
| Synovial fluid analysis | Total count : 10,000 cells/cumm Differential count(from centrifuged deposits) : [Table/Fig-5] -Neutrophils :1% -Lymphocytes: 4% -Eosinophils: 95% Others: Few synoviocytes present No red blood cells seen in the background No microfilaria. |
| Synovial fluid | Proteins: 5.9g% Sugar: 85mg |
| Staining and culture | Gram stain : Negative AFB Stain: Negative Culture : No growth |
Leishman stain (40X); Smear shows predominantly of eosinophils. No RBCs seen in the background)

Clues to probable etiology [6]
| clues to probable etiology | ASIA grade A | ASIA grade B |
|---|
| volume, ml | <3.5 | >3.5 | >3.5 |
| Viscosity, cm | 3-6 | <3 | <3 |
| Color | Straw yellow | Opaque yellow | Milky |
| Leukocytes/ul | 50-2000 | 2000=75000 | >75000 |
Treatment and follow up
Patient was put on Hetrazan (Diethylcarbamazine) in a dose of 2mg/kg TDS for a period of 3 wk + iron and folic acid supplementation to correct the anaemia After a course of 3 wk of DEC+ iron and folic acid, the blood parameters returned to normal – with a fall in eosinophils from 12 % to 5%. The patient did not develop any subsequent swellings of the knee. On 6 months follow up the patient has not had any recurrence of symptoms an.
Discussion
Needle aspiration of synovial fluid forms the bedrock in the work up of patients presenting with synovial effusion [1]. The synovial fluid should be aspirated under strict aseptic precautions and sent as separate samples for a) Gross characteristics, b) Cell count, c) Constituents such as sugar, protein d) Microbiological staining such as Gram and Ziehl Nielsen for acid fast bacilli and e) Culture.
The gross characteristics such as colour, volume and viscosity provide clues to the probable aetiology as referenced in [Table/Fig-6].
Special investigations may then be carried out depending on the outcome of the preliminary workup.
Few cases of synovial fluid eosinophilia have been reported in literature [2]. Gupta and Katji [3] identified presence of eosinophils in cases of tuberculous synovitis and rheumatoid arthritis. But, in their study the eosinophil was not the predominant cell and hence did not have any diagnostic utility. Similar to Bona Tauro [4] our study is also from an area of high prevalence of filaria and similarly we did not find any evidence of microfilaria in the synovial fluid or blood. The presence of synovial fluid eosinophilia could be secondary to a wide variety of diseases which need to be investigated for as listed in [Table/Fig-7] below [5]. If these tests cannot pick up a primary factor causing the eosinophilia they are labelled as idiopathic. Hence, our patient falls under the idiopathic variety. All previous reports of idiopathic eosinophilic synovitis have had normal levels of eosinophils in the peripheral smear. However, our patient has peripheral blood eosinophilia which is the first of its kind according to our review of literature. After 3 wk of DEC, the peripheral blood eosinophilia was corrected and the patient did not develop subsequent knee effusions.
List of diseases causing eosinophilia [7–11]
| Allergic Diseases : Drug reactions, allergic rhinitis, Urticaria |
| Atopic diseases: Asthma, eczema, atopic dermatitis |
| Parasitic infections : ancylostomiasis, filaria, ascariasis |
| Connective tissue disorders : poly arteritis nodosa, rheumatoid arthritis, Chrug-strauss syndrome |
| Skin disease : Pemphigus, exfoliative dermatitis, dermatitis herpetiformis |
| Pulmonary infiltration syndromes : Lofflers syndrome, Tropical pulomnary eosinophilia |
| Malignancy : Lymphoma, Leukemia, Hodgkin's disease |
| Eosinophilic syndromes : Eosinophilia myalgia, Shulman's syndrome, Idiopathic Hypereosinophilic Syndrome |
| Miscellaneous : Brucellosis, radiation therapy |
A short course of DEC may hence be considered curative for this problem as the symptoms have not reappeared after 6 months follow up. However, longer study periods are necessary in a larger sample of patients before definitive conclusions can be made.
Conclusion
Idiopathic eosinophilic synovitis with peripheral eosinophilia is an extremely rare but easily curable condition. The above case is a beautiful illustration of the principle that all effusions need to be investigated appropriately and not passed off as just another effusion which is drained and samples forgotten which might lead to a recurrence of the disease. This is case is hence presented not only for its rarity but also the fact if correctly identified, cured very easily.
[1]. Johnson Michael W, Acute Knee Effusions: A Systematic Approach to DiagnosisAm Fam Physician 2000 61(8):2391-400. [Google Scholar]
[2]. Curtiss PH Jr, Changes produced in the synovial membrane and synovial fluid by diseaseJ Bone Joint Surg (Am) 1964 46-A:873-88. [Google Scholar]
[3]. Rajendra Verma, Gupta SP, Katju Vinod, Place of synovial fluid examination and needle biopsy of synovial membrane in diagnosis of monoarticular joint diseaseIndian J Orth 1983 17:8-13. [Google Scholar]
[4]. Bona Tauro, Eosinophilic synovitis - a new entity?J Bone Joint Surg (Br) 1995 77-B:654-56. [Google Scholar]
[5]. Tay CH, Eosinophilic ArthritisRheumatology 1999 38:1188-94. [Google Scholar]
[6]. Araceli Martinez-Castillo, Carlos Nunez, Javier Cabiedes, Synovial fluid analysisReumatol Clin 2010 6(6):316-21. [Google Scholar]
[7]. Vazquez-Trinanes C, Sopena B, Synovial fluid eosinophilia: a case series with a long follow-up and literature reviewRheumatology (Oxford) 2013 52(2):346-51. [Google Scholar]
[8]. Atanes A, Fernandez V, Idiopathic eosinophilic synovitis. Case report and review of the literatureScand J Rheumatol 1996 25(3):183-85. [Google Scholar]
[9]. Brown JP, Rola-Pleszczynski M, Menard HA, Eosinophilic synovitis: clinical observations on a newly recognized subset of patients with dermatographismArthritis Rheum 1986 29(9):1147-51. [Google Scholar]
[10]. Padeh S, Laxer RM, Gleich GJ, Armstrong PF, Silverman ED, High synovial immunoglobulin E levels in eosinophilic synovitisJ Pediatr 1992 121(3):417-19. [Google Scholar]
[11]. Martín-Santos JM, Mulero J, Arthritis in idiopathic hypereosinophilic syndromeArthritis Rheum 1988 31(1):120-25. [Google Scholar]