Inflammation of the periodontium caused by irritants of endodontic origin is termed as perioodontitis [1]. As a consequence of pathologic changes in the dental pulp, the root canal system can harbor numerous irritants. Egress of these irritants from infected root canals into the periradicular tissues can initiate formation and perpetuation of periradicular lesions. Depending on the nature and quantity of these irritants, as well as the duration of exposure of the periradicular tissues, a variety of tissue changes can occur. When the irritants are transient in nature, the inflammatory process is short-lived and self-limiting. However, with an excessive amount of irritants or persistent exposure, the nonspecific and specific immunologic reactions can cause destruction of periradicular tissues [2].
Radiographically, these lesions appear as radiolucent areas around the portal(s) of exit of the main canal or lateral and/or accessory canals. Histologically, depending on their stage of development, the lesions contain numerous inflammatory cells such as polymorphonuclear neutrophil leukocytes (PMNs), macrophages, lymphocytes, plasma cells, mast cells, basophils, and eosinophils [2].
Radiographs are an important part of root canal treatment; especially for detection, treatment planning and follow up of periapical bone lesions. However, routine radiographic procedures do not demonstrate reliably the presence of every lesion and they do not show the real size of the lesion and its spatial relationship with anatomical structures. Radiographs alone cannot differentiate between cystic and non cystic lesions [3].
Direct digital radiography (DDR) is the direct replacement of an x-ray film with an electronic image receptor or sensor and an image displayed on a computer [4]. The most significant advantage to the Direct Digital Radiography style devices is the near instantaneous (a few seconds) availability of the images after exposure without removing the sensor from the mouth. This allows multiple angles to be taken to help in location of canals, identification of root curvatures, verification of working lengths, and verification of intermediate obturation results [4]. Direct digital radiography is no better than conventional radiography in the detection and measurement of periapical lesions.
Ultrasonography is an imaging technique in which deep structures of the body are visualized by recording the reflections (echoes) of ultrasonic waves directed into the tissues. Frequencies in the range of 3 million to 12 million hertz are used for diagnostic ultrasonography in dentistry [5]. In diagnostic ultrasonography for periapical lesions the mechanism of action depends on the ultrasonic waves that are produced by electrically stimulating a piezoelectric crystal called a transducer. As the beam strikes an interface or boundary between tissues of varying acoustic impedance (e.g. muscle and blood) some of the sound waves are reflected back to the transducer as echoes. The echoes are then converted into electrical impulses that are displayed on an oscilloscope, presenting a ‘picture’ of the tissues under examination [5].
Doppler ultrasonography is one in which the shifts in frequency between emitted ultrasonic waves and their echoes are used to measure the velocities of moving objects, based on the principle of the Doppler effect. The waves may be continuous or pulsed and this technique is frequently used to examine blood flow in periapical lesions [5].
Periapical lesions accompanying endodontic infection are usually diagnosed and treated primarily on the initial radiographic findings. Sometimes periapical surgery is necessary to eliminate and diagnose the cystic and non-cystic nature of the lesion. Several authors have recommended that those periapical lesions not responding to conservative endodontic therapy should undergo histopathologic examination. For a predictable diagnosis and prognosis of non-surgical endodontic treatment and in some cases avoiding surgical trauma, it is important to evaluate new and perhaps more promising methods of imaging for the study of periapical lesions [6].
Materials and Methods
Study was done at Darshan dental college and hospital Udaipur in the year 2010, for a duration of one year and seven months.
Criteria case selection
Thirty subjects in the age group of 15 to 50 y irrespective of sex and socio-economic status were selected. Selected subjects were supposed to fulfill the following criteria –
Inclusion Criteria
Those whose teeth showed periapical radiolucency of endodontic origin raw were they diognosed with or without clinical signs and symptoms of inflammation.
Only the anterior teeth of either arch with periapical osseous defects were selected.
The subjects were selected irrespective of the number of teeth involved in the periapical osseous defect.
The patients were informed of the prognosis for a successful outcome and the risks involved in the surgical procedure, in addition to the benefits. They were also informed of the possible short-term effects of the surgery, such as pain, swelling, discolouration, and infection.
Signed informed consent forms were procured.
Ethical clearance was taken from the university prior to starting the study.
Exclusion Criteria
Pregnant & nursing patients.
History of antibiotic therapy.
Inability to comply with the follow-up visit requirements.
Distribution of patients
Group 1-Patient having lesions which were diagnosed as Granuloma in conventional radiography, digital radiography and colour Doppler ultrasonography.
Group 2-Patient having lesions which were diagnosed as Cyst in conventional radiography, digital radiography and colour Doppler ultrasonography.
Group 3-Patient having lesions which were diagnosed as mixed lesion in conventional radiography, digital radiography and colour Doppler ultrasonography.
Based on the findings by two Endodontists and an oral Radiologist (total number of three observers), the diagnosis of nature of the lesion was made. When two of three observers came to a common decision the diagnosis was confirmed for evaluation. If all the three evaluators failed to obtain a common decision, the lesion was re-evaluated by all of them.
Radiographic Examination Coventional Radiography
The preoperative periapical radiograph of each offending tooth was taken with intra-oral film Kodak E speed (Eastman Kodak co. France No. 2, 31mm x 41 mm W2) using paralleling technique using the Sensor-Pro film-holder(RINN EXP type film holder DENTSPLY) with beam aiming device and an X-ray unit:( GOMAX 10DRS) dental X-ray unit (65 kVp, 10 mA, 1.5 aluminium filtration, 60mm beam diameter, Focus to skin distance (FSD) 200mm). The radiographs were then analysed with the help of two endodontists and a oral radiologist opinion, with a view to the margin, size, and shape to assess the nature of lesion. It was also examined for the normal anatomy, trabecular pattern, thickness of the lamina dura or any external and/or internal resorption. After considering the clinical and radiographic findings, a provisional diagnosis of the Periapical Radiolucent Lesion (PARL) was made.
Digital radiographic examination
After conventional radiograph, the patients were subjected to direct digital paralleling technique radiographic examination using (SOPIX) digital charged couple device with intra oral sensor (39mm x 23 mm) model (13 705 La CIOTAT – FRANCE).with beaming device (ORIX – 70, 70 kVp, 8mA, 0.414 Kw, Focal spot- 0.8, filtration-2.5, tube diameter 60mm, Focus to Skin Distance – 200mm, X-Ray tube – Toshiba DG073B). The digital radiographs were then analysed with the help of two endodontits and an oral radiologist opinion, with a view to the margin, size and shape to assess the nature of lesion. When two of three observers came to a common decision the diagnosis was confirmed for evaluation. If all the three evaluators fail to obtain a common decision, the lesion was reevaluated by all of them.
Radiographic assessment was made based on following principles [3,7]:
Periapical Granulomas
Location – the cases in which apex was involved.
Periphery – lesions with ill defined margins, showing gradual transition from surrounding normal trabecular pattern into abnormal bone pattern of lesion.
Sharp transitional bone and appearance suggesting a cortical boundary.
Internal structure – loss of bone density
Widening of periodontal ligament space at apex.
Mixture of sclerosis and rarefaction of normal bone. Lamina dura lost at apex of tooth.
External resorption of apical region of root may occur in chronic cases.
Periapical Cysts
Location – cases in which epicenter of periapical cyst is located at the apex of non vital tooth.
Periphery & shape – well defined cortical borders
If cyst becomes secondary infected inflammatory reaction results in loss of cortex or alteration of the cortex into a more sclerotic borders.
Outline is usually curved or circular unless it is influenced by surrounding structures.
Internal structure – radiolucent
Dystrophic calcification - in long standing cases.
A cyst is usually larger than granuloma and may cause the root of adjacent teeth to spread apart because of continuous pressure from accumulation of cystic fluid.
Ultrasonographic Examination
An ultrasound examination was then performed using the diagnostic ultrasound machine, Volusion-730- expert (GE Medical System, USA), with colour Doppler function, incorporating a high definition, multifrequency, 40 mm linear foot print, ultrasonic Probe (LA-39) operating at a frequency of 6–12 MHz. The ultrasound probe was first covered with disposable cling film for control of infection, and then covered with a layer of ultrasound gel (Ultragel, Medicon, India). The probe was positioned outside the mouth on the skin overlying the periapical area. The probe position was changed several times in order to obtain an adequate number of transverse scans (axial plane) to define the bony defect. Longitudinal scans (sagittal plane) were also obtained.
The images of each lesion were analysed by two endodontists and by an expert ultrasonographer. A tentative differential diagnosis was agreed upon, based on the following principles.
Cystic lesion: A hypoechoic well-contoured cavity surrounded by reinforced bone walls, filled with fluid and with no evidence of internal vascularization on colour Doppler examination.
Granuloma: A poorly defined hypoechoic area, showing rich vascular supply on colour Doppler examination.
Mixed lesion: Predominantly hypoechoic area with focal anechoic area, showing vascularity in some areas on Colour Doppler examination.
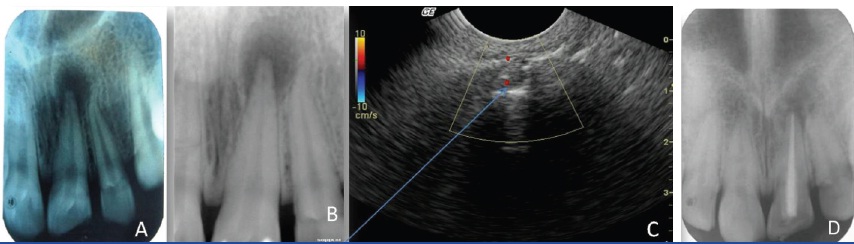
The cases which were diagnosed either as periapical cysts or as periapical granuloma by conventional radiography, digital radiography and ultrasonography were operated following the principles of periradicular surgery and biopsies were obtained from the periapical areas. After fixation in 10% buffered formalin, the surgical specimens were processed for routine histopathological examination [Table/Fig-1].
Large periapical lesion which was diagnosed as cyst in conventional radiography(A). Digital radiograph of same periapical lesion (B) Ultrasonographic image of lesion. Arrow shows peripheral blood supply the borders diagnosingh the lesions as granuloma. (C) Histopathological picture of the lesion revealing featuresd of granuloma i.e stromal components exhibiting numerous proliferating dilated blood capillaries, abundant chronic inflammatory infiltrate predominantly of plasma cells and lymphocytes, areas of stromal necrosis surrounded by inflammatory cells, haemorrhagic areas along with cellular debris.(D)

The cases which were diagnosed as granuloma by conventional radiography and digital radiography, but mixed lesion by colour Doppler ultrasonography were treated non-surgically [Table/Fig-2].
Pretreatment radiograph of lesion in relation to 21 diagnosed as Granuloma in conventional radiograph. (A) Pretreatment radiograph of lesion diagnosed as granuloma in digital radiograph. (B) Ultrasound image showing predominantly hypoechic area, hence diagnosed as mixed lesion. (C) Postreatment radiograph after nonsurgical treatment.(D)
Results
Statistical analysis was done with Chi-Square test and using one-way-Anova. [Table/Fig-3] Reveals that the nature of the lesion in identification of the lesion depends on the type of diagnostic aid p<0.001.
Correlation of CR, DDR and CDUSG in diagnosing periapical lesions
| Granuloma | Cyst | Mixed lesion |
|---|
| Conventional Radiography (CR) | 25 | 5 | 0 |
| Digital radiography (DDR) | 25 | 5 | 0 |
| Ultrasonography(CDUSG) | 16 | 0 | 14 |
| p < 0.001 |
For conventional radiography and digital radiography the findings were same i.e. 25 granuloma and 5 cyst whereas in case of ultasonography 16 were diagnosed as granuloma and 14 as mixed lesion.
[Table/Fig-4] After correlating ultrasonography and histopathological report it can be concluded that the results were significant p<0.001.
Correlation between ultrasonography and histopathological reports
| Type of Lesion Cyst | | Histopathology | Ultrasonography |
|---|
| Granuloma | Within Groups(p-Value) | <0.001 | <0.001 |
| Within Groups (p-Value) | <0.001 | <0.001 |
[Table/Fig-4] shows that the there was a significant correlation between the results of ultrasonography and histopathological reports. Hence, it can be concluded that colour Doppler ultrasonography is an effective tool for diagnosis for nature of periapical lesions.
Discussion
This study has confirmed ultrasound real time imaging as a reliable diagnostic technique for differentiating periapical lesions, i.e. periapical cysts and granulomas, based on the echo-texture of their contents and the presence of vascularity using colour Doppler along buccal caries as where the buccal cortical bone is thin. Even sinus tracts and cystic lesions with complications, i.e. infected cyst and mixed lesion of cyst and granuloma, can be diagnosed.
16 lesions, out of 30, were diagnosed as granuloma and 14 lesions were diagnosed as mixed lesion using colour Doppler ultrasonography (CDUSG) as shown in [Table/Fig-3]. Conventional radiography (CR) and Digital Radiography (DDR) enable diagnosis of periapical disease existence, but not of its nature; while ultrasound underestimates the extent of disease, but can provide accurate information on the pathological nature of the lesion.
Ultrasound imaging is a very useful imaging technique which can give significant diagnostic information in relation to periapical lesions in the anterior region where the buccal bone is thin. The results suggested that, if only clinical findings were available, an endodontist trained to use ultrasound should be able to diagnose a periapical lesion without taking a periapical radiograph and be sure of the underlying disease process. Dimensional measurements of the lesion still require Conventional radiography or Digital radiographs.
Colour Doppler Ultrasonography (CDUSG) gives exact nature of the lesion. If a clinician can predict exact nature of the lesion, it will be easier to plan treatment and can have predictable prognosis. In this study in cases of mixed lesion (a lesion with capillary supply) were treated non-surgically and the results were favorable.
Goel et al., concluded that ultrasonography imaging with colour Doppler and power Doppler is superior to conventional intraoral radiographic methods for diagnosing the nature of periapical lesions in the anterior jaws [8].
Parihar et al., compares the effectiveness of ultrasound and radiography techniques in diagnosing the endodontic lesions. Generally, the identification of periapical lesions is based on biopsy and surgery is a necessity for lesions which persists even after re-root treatement. Conventional radiography could not identify the nature of lesions while the diagnosis based on ultrasound images of a cyst, was agreed by both, an ultrosonographer and an endodontist [9].
Christo Naveen Prince et al stated that with its potential usefulness to differentiate the periapical lesions, ultrasonography can be considered as a better imaging modality with improved efficacy when compared to conventional radiography. In comparision to histopathologic diagnosis, ultrasonography showed less accuracy and thus can be considered to be a supplementary tool in the differential diagnosis of periapical lesions [10].
There has been an endless controversy about an accurate diagnosis of periapical granuloma and a cyst using conventional radiographic image. Its line of treatment whether to be treated surgically, non-surgically or a combined non-surgical re-treatment with periapical surgery is still a topic of debate.
But a study by Vier Figueiredo (2002) suggest that the most common periapical radiolucent lesion of endodontic origin is not a periapical granuloma but a non cystic lesion with periapical abscess, occupying more than or equal to 1/3rd of total area visualized in the histologic section.
In all 16 cases, histology confirmed the ultrasound observations with respect to the nature of the underlying lesions. Out of 16 patients 5 patients were diagnosed as radicular cyst by CR and DDR, but CDUSG had diagnosed these lesions as periapical granulomas. The results of histological examination of these lesions were also periapical granuloma, hence confirming the diagnosis of ultrasonography. Rest 11 patients were diagnosed as granulomas by ultrasonography and histopathology of the lesion confirmed the diagnosis.
Conclusion
Within the limitations of this study it could be concluded that Conventional radiography and direct digital radiography enable the diagnosis of the presence of periapical disease, but do not give any indication of its nature. Colour Doppler Ultrasonography can predict the nature of the lesion. Ultrasound imaging is possible through thinned or perforated cortical bone. It underestimates the dimensions of the lesions, but can provide accurate information on the pathological nature of periapical disease.
Treatment planning becomes unpredictable with Conventional and digital radiography as they are unable to detect mixed lesions. But, Periapical lesions which are diagnosed as mixed lesion only on Colour Doppler Ultrasonography can be treated nonsurgically.