Diffuse large B – Cell lymphoma involving the maxilla in a minor
Garish Kumar1, Nupur Hingad2, Navneet Singh3, Gagandeep Kaur Sidhu4
1 Reader, Department of Oral Pathology and Microbiology, Maharaja Ganga Singh Dental College and Research CenterSriganganagar, Rajasthan, India.
2 Reader, Department of Oral Pathology and Microbiology, Sri Sukhmani Dental College and Hospital, Dera Bassi, Punjab, India.
3 Senior Lecturer, Department of Oral Pathology and Microbiology, Maharaja Ganga Singh Dental College and Research CenterSriganganagar, Rajasthan, India.
4 Senior Lecturer, Department of Oral Pathology and Microbiology, Maharaja Ganga Singh Dental College and Research CenterSriganganagar, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Garish Kumar, Reader, Department of Oral Pathology and Microbiology, Maharaja Ganga Singh Dental College and Research Center, Sriganganagar, Rajasthan, India. Phone : 09988634315, E-mail : drgarish@gmail.com
Lymphomas can be simply defined as malignant neoplasms of lymphocytes and their precursor cells. We report a case of a diffuse large B-cell lymphoma of the maxilla, in an 11-year-old male patient who reported with a diffuse swelling of the maxillary labial mucosa accompanied with oral candidiasis. A subsequent biopsy and immunohistochemistry were instrumental in this diagnosis. What makes this case significant is that the incidence of primary DLBCL in the oral cavity of a minor which is not very common and has rarely been specified earlier in the literature.
Biopsy, Immunohistochemistry, Swelling
Case Report
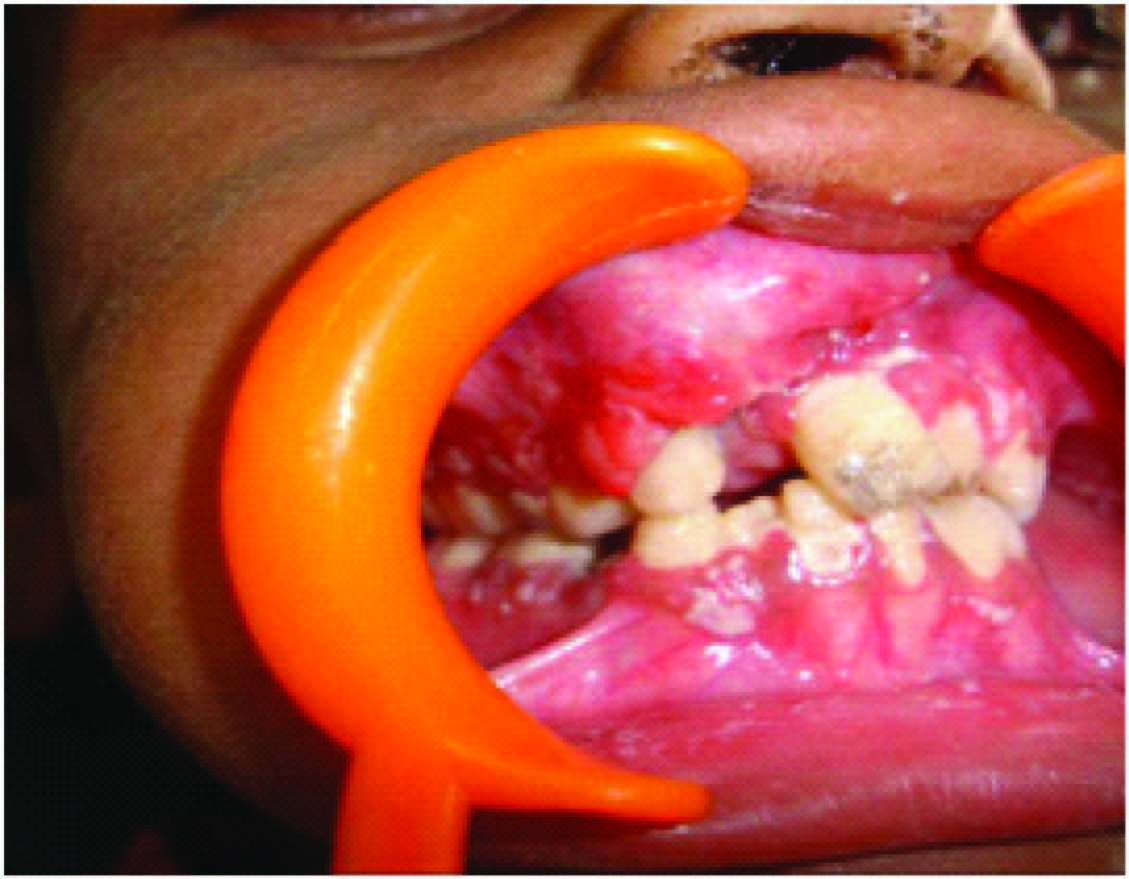
An 11-year-old male patient was referred to the Department of oral Surgery with a diffuse swelling involving the maxillary mucosa. The swelling was insidious in onset and gradually increased in size. There was asymmetry of the face due to the swelling, and no altered sensation. On intaoral inspection a solitary diffused swelling was evident. Extension of the Soft tissue swelling was from the left central incisor to right first Molar. Lingual extension of the swelling was also observed in the anterior region. Swelling appeared reddish pink in colour with a smooth surface. Patient had a mixed dentition. The oral hygiene was very poor. On palpation there was no local raise in temperature and the swelling was non tender. It was firm to hard in consistency and the surface was smooth. Extraorally Overlying skin was easily pinchable [Table/Fig-1]. Extraoral examination showed swelling of the submandibular, sublingual and cervical lymph nodes. The patient looked very weak and disoriented. His medical history and family history were not contributory.
Diffuse swelling involving the maxillary mucosa
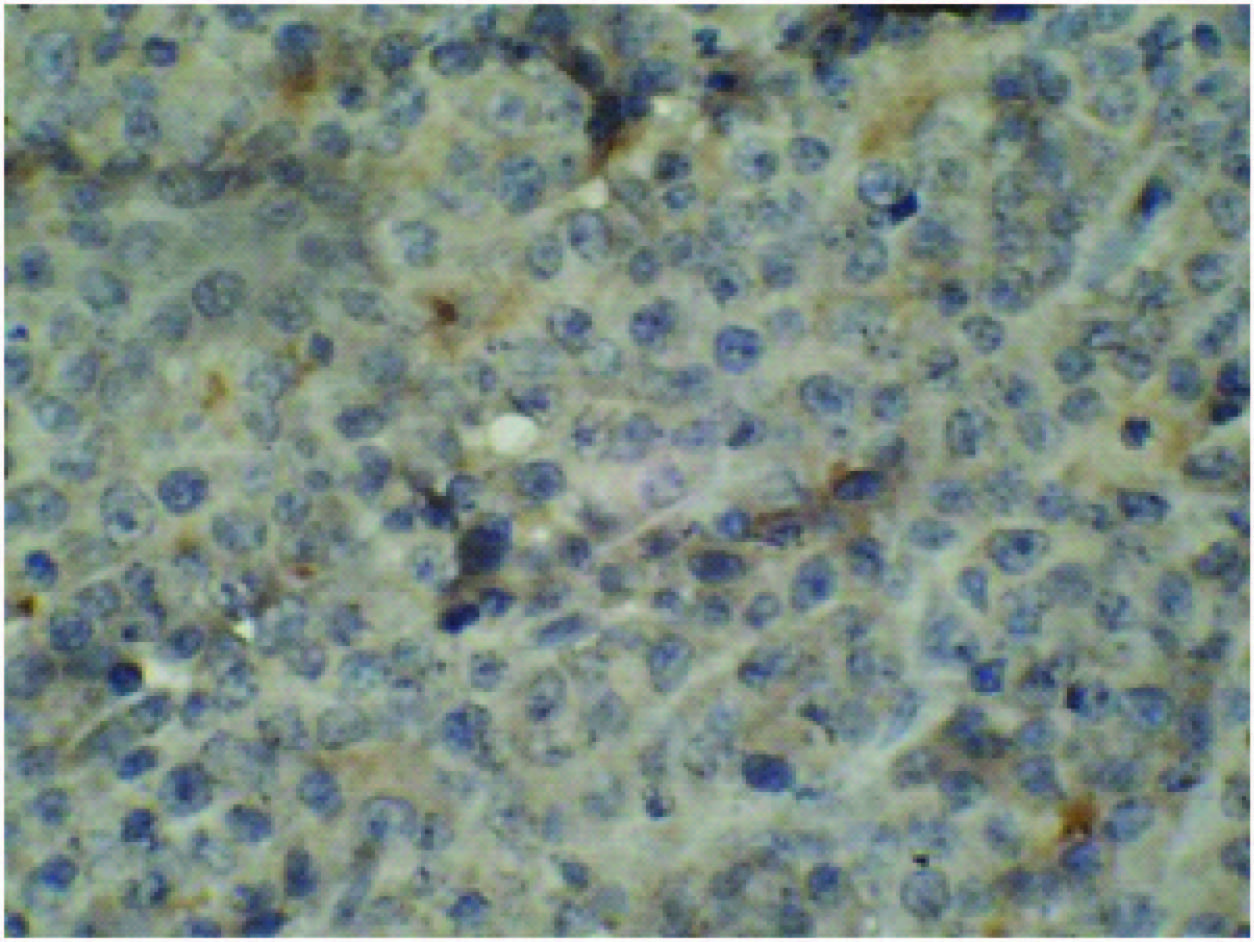
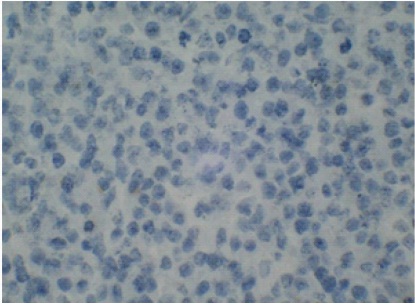
Intra oral radiograph did not prove to be helpful. Blood investigations revealed that all parameters were within normal limits.A provisional diagnosis of traumatic fibroma, lipoma, benign minor salivary gland tumour were considered. Incisional biopsy was carried out after which the biopsy specimen was processed and haematoxylin and eosin stained sections revealed sheets of abnormally large lymphoid cells with high Nucleus: Cytoplasmic ratio, coarse chromatin and inconspicuous nucleoli with abnormal mitotic figures. The features were suggestive of large cell lymphoma [Table/Fig-2a&b].
Hematoxylin and eosin stained sections showing sheets of abnormally large lymphoid cells with high nucleus cytoplasmic ratio, coarse chromatin and inconspicuous nucleoli with abnormal mitotic figures

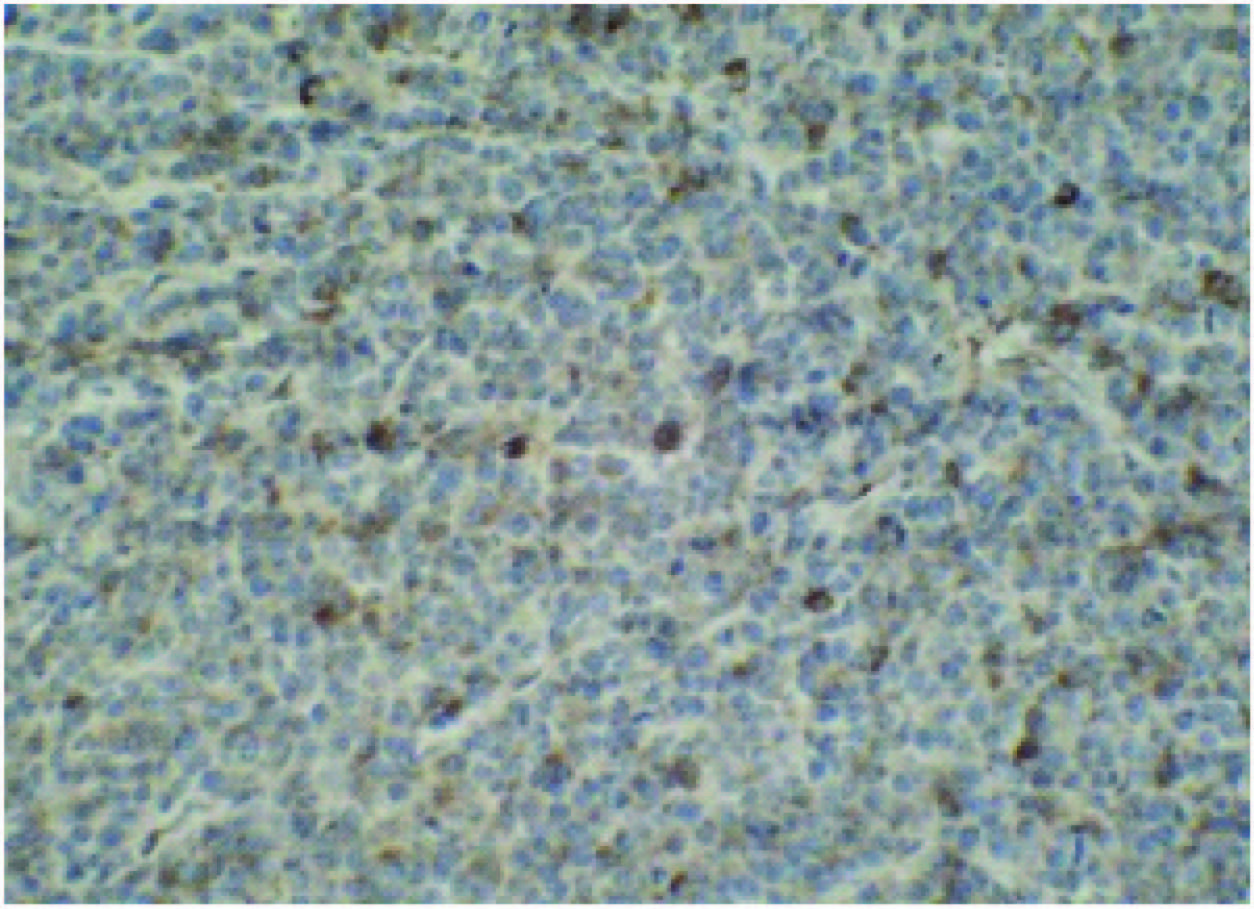
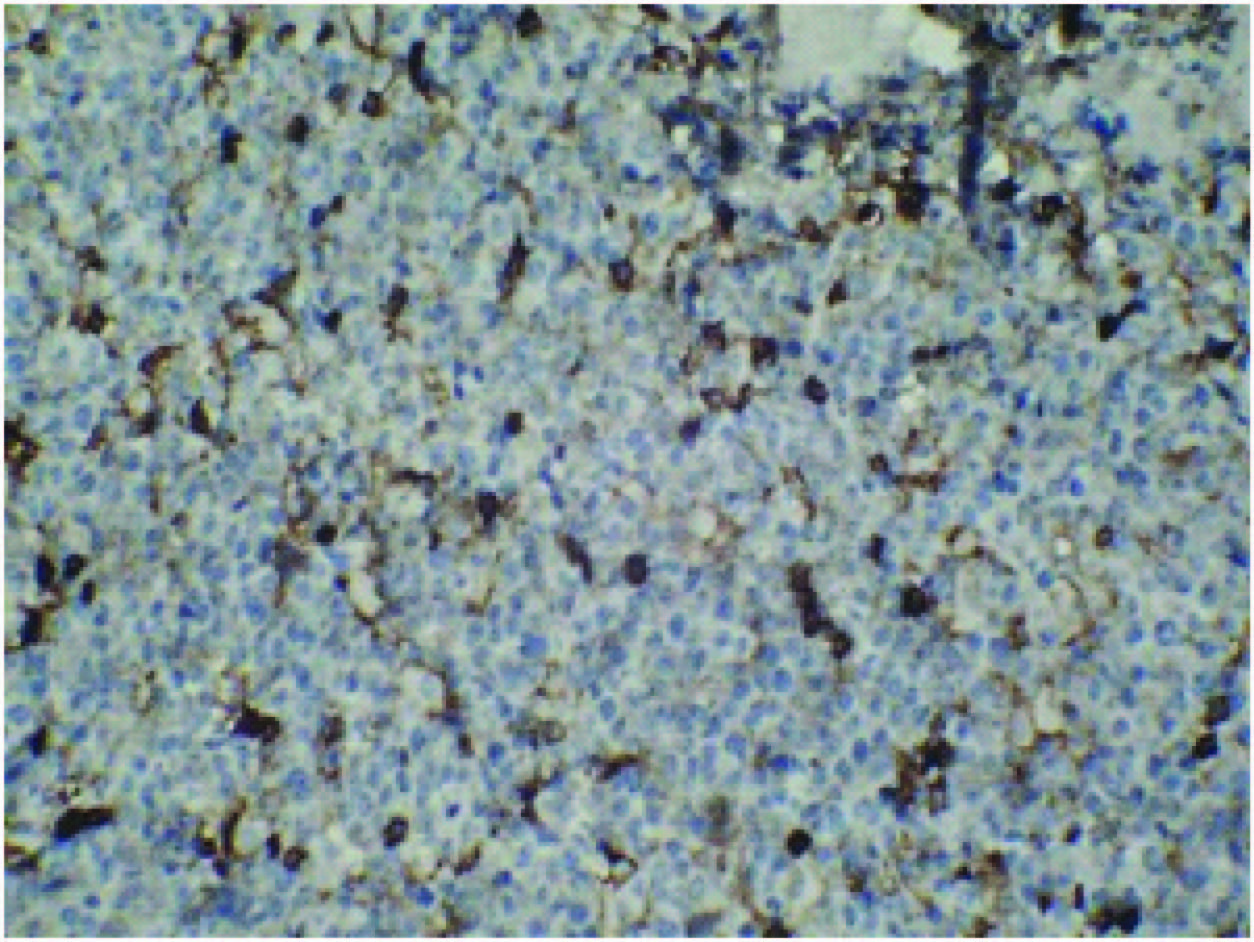
Then immunohistochemistry was undertaken which was positive for CD20, CD79a, LCA& CD45 [Table/Fig-3a,b,c] and negative for CK [Table/Fig-4] and CD3, which proved conclusively the lesion to be as a B-cell lymphoma.
Chemotherapy was advised by the oncologist and a total of six cycles were suggested at the gap of every three weeks. The treatment regimen followed was that of classical CHOP therapy which comprised of using Cyclophosphamide, doxorubicin (Hydrodoxorubicin), vincristine (Oncovin) and Prendisolone. At the end of two cycles the swelling started decreasing in size and disappeared after four cycles. The patient was examined periodically once in two months. It’s been one and a half years now, he is disease free.
Discussion
Lymphoma is the second most common neoplasm of the head and neck. Non-Hodgkin’s lymphomas are a group of neoplasms that originate from the cells of the lymphoreticular system [1]. These malignancies initially arise within the lymphatic tissues and may progress to an extra nodular mass (non-Hodgkin’s lymphoma) or to a nontender mass or masses in a lymph node region (Hodgkin’s lymphoma) that later may spread to other lymph node groups and involve the bone marrow [2]. It has been known traditionally to divide lymphomas into Hodgkin’s disease (HD) and non-Hodgkin’s lymphomas (NHL) because of their difference in histology and patterns of behaviour [3].
Lymphoma in the oral soft tissues, usually presents as an extranodal, soft-to-firm asymptomatic lesion, although the mass may also be painful. These lesions may be clinically indistinguishable from squamous cancer of the head and neck. Oral involvement by lymphoma may represent a local disease process, but more frequently is part of a widespread disease that may also involve the head and neck regional lymph nodes [2]. Among the jaw lesions, maxilla is more frequently involved than mandible also it is the second most common neoplasm of the head and neck after squamous cell carcinoma. In the head and neck region, it can involve any area, including Waldeyer’s ring (i.e., the tonsils, pharynx, and base of the tongue), the orbit, the paranasal sinuses, the salivary glands, and the thyroid. Diffuse large B-cell lymphoma (DLBCL) is the most frequently diagnosed type of non-Hodgkin lymphoma (NHL) and is the fifth most frequent cancer, accounting for 30–40% of all cases reported in literature. It is frequently reported in the mediastinum, gastrointestinal tract, bone marrow, central nervous system, breast and testes. When compared to other cases in literature most cases occur in patients in the seventh decade of life. NHLs of the oral cavity are rare and account for only 3–5% of the lymphomas reported. They can be primary or secondary to extension from Waldeyer’s ring. Jaw involvement by NHL is rare, but among jaw lesions, maxilla is more frequently involved than mandible. The most frequent type of primary NHL lymphoma of the oral cavity is DLBCL. These lesions are symptomatic and typically present as a rapidly enlarging mass. Outside of the Waldeyer’s ring, in the oral cavity, the hard palate and the maxillary vestibule appears to be frequently involved. DLBCL is characterized by a diffuse proliferation of large neoplastic B cells with nuclear size equal to or exceeding normal macrophage nuclei, or more than twice the size of a normal lymphocyte. DLBCL is a heterogenous neoplasm with variable clinical, morphologic, immunophenotypic, cytogenetic, and genetic features. This is reflected in their marked biological heterogeneity and highly variable clinical course [4].
Our case when compared to other cases was suggestive of features like absence of characteristic clinical features when jaw bones are involved, they can present as swelling of the jaw, pain, numbness, tooth mobility or cervical lymphadenopathy [5,6]. Lymphomas show a male predominance with male to female ratio 3:2. Radiographic signs of bone involvement may be absent in 10-20% of cases and the radiographic findings may not be specific [5,7] which was the finding in our case also. NHL can be managed by chemotherapy, radiotherapy and surgery in various combinations. NHL arising in bone is best treated by chemotherapy and may not require radiotherapy. Survival is excellent in localized disease, whereas disseminated disease seems less favourable [8–10].
Though lymphoma of mandible is rare, it must be considered in the differential diagnosis of swellings arising in that region. Prognosis is excellent in localized disease, whereas in disseminated disease, it is less favourable. Lymphomas arising in bone may be effectively managed by chemotherapy alone. with the increase in the incidence of extra-nodal Lymphomas, the present age dentist must properly investigate the swellings of orofacial region and treat it judiciously.
Current treatment of DLBCL usually begins with multi agent chemotherapy, typically CHOP (cyclophosphamide, hydroxydoxorubicin, oncovin and prednisone). The chemotherapy usually involves three cycles of CHOP. Other drugs used in multiagent chemotherapy for advanced stage disease usually involve various combinations of methotrexate, bleomycin, doxorubicin, vincristin, dexamethasone and leukcovorin, etoposide, mechlorethamine, procarbazine, cytarabine. Early stage of disease response either to chemotherapy or a combination of chemotherapy and radiotherapy. Patients are considered for bone marrow tranplant if remission is not maintained. The role of surgery is severly limited in treatment of DLBCL [11].
Conclusion
In order to diagnose lymphoma the dentist should be aware of the clinical features of the tumour. Early diagnosis leads to treatment at an early stage of the tumour which results in better prognosis for the patient. Careful patient evaluation after treatment is essential to rule out recurrence.
[1]. Adwani DG, Arora Rajender Singh RS, Bhattacharya Anirudh A, Bhagat Bhushan B, Non-Hodgkin's lymphoma of maxillary sinus: An unusual presentationAnn Maxillofac Surg 2013 3(1):95-7. [Google Scholar]
[2]. Epstein JB, Epstein JD, Nhu D Le, Gorsky M, Characteristics of oral and paraoral malignant lymphoma: A population-based review of 361 casesOral Surg Oral Med Oral Pathol Oral Radil Endod 2001 92:519-25. [Google Scholar]
[3]. Abadi RZM, Sistani NS, Mohtasham N, Hesari KK, Vaezi T, Pazouki M, The prevalence of Epstein-Barr virus infection in head and neck non-Hodgkin's lymphomas in Khorasan, northeast of IranJ Pak Med Assoc 2013 63:882-87. [Google Scholar]
[4]. Bhattacharyya I, Chehal HK, Cohen DM, Al-Quran SZ, Primary diffuse large B-cell lymphoma of the oral cavity: germinal center classificationHead Neck Pathol 2010 4(3):181-91. [Google Scholar]
[5]. Reddy Indira, Sreenath G, Reddy Raghavendra Y, Prakash Ravi A, Swathi TR, Non- Hodgkins Lymphoma in Boccal Vestibule-Case ReportJournal of Clinical and Diagnostic Research 2014 8:QD01-2. [Google Scholar]
[6]. Rosado MF, Morgensztern D, Peleg M, Lossos IS, Primary diffuse large cell lymphoma of the mandibleLeuk Lymphoma 2004 45:1049-53. [Google Scholar]
[7]. Gusenbauer AW, Katsikeris NF, Brown A, Primary lymphoma of the mandible: report of a caseJ Oral Maxillofac Surg 1990 48:409-15. [Google Scholar]
[8]. Someya M, Sakata K, Nagakura H, Itou K, Nakata K, Oouchi A, Three cases of diffuse large B-cell lymphoma of the mandible treated with radiotherapy and chemotherapyRadiat Med 2005 23:296-302. [Google Scholar]
[9]. Kirita T, Ohgi K, Shimooka H, Okamoto M, Yamanaka Y, Sugimura M, Primary non-Hodgkin’s lymphoma of the mandible treated with radiotherapy, chemotherapy, and autologous peripheral blood stem cell transplantationOral Surg Oral Med Oral Pathol Oral RadiolEndod 2000 90:450-55. [Google Scholar]
[10]. Horning SJ, Weller E, Kim K, Earle JD, O’Connell MJ, Habermann TM, Chemotherapy with or without radiotherapy in limited-stage diffuse aggressive non-Hodgkin’s lymphoma: Eastern Cooperative Oncology Group study 1484J Clin Oncol 2004 22:3032-38. [Google Scholar]
[11]. Sahoo SR, Misra SR, Mishra L, Mishra S, Primary diffuse large B-cell lymphoma in the anterior hard palate: A rare case report with review of literatureJ Oral Maxillofac Pathol 2014 18(1):102-06. [Google Scholar]