Case Report
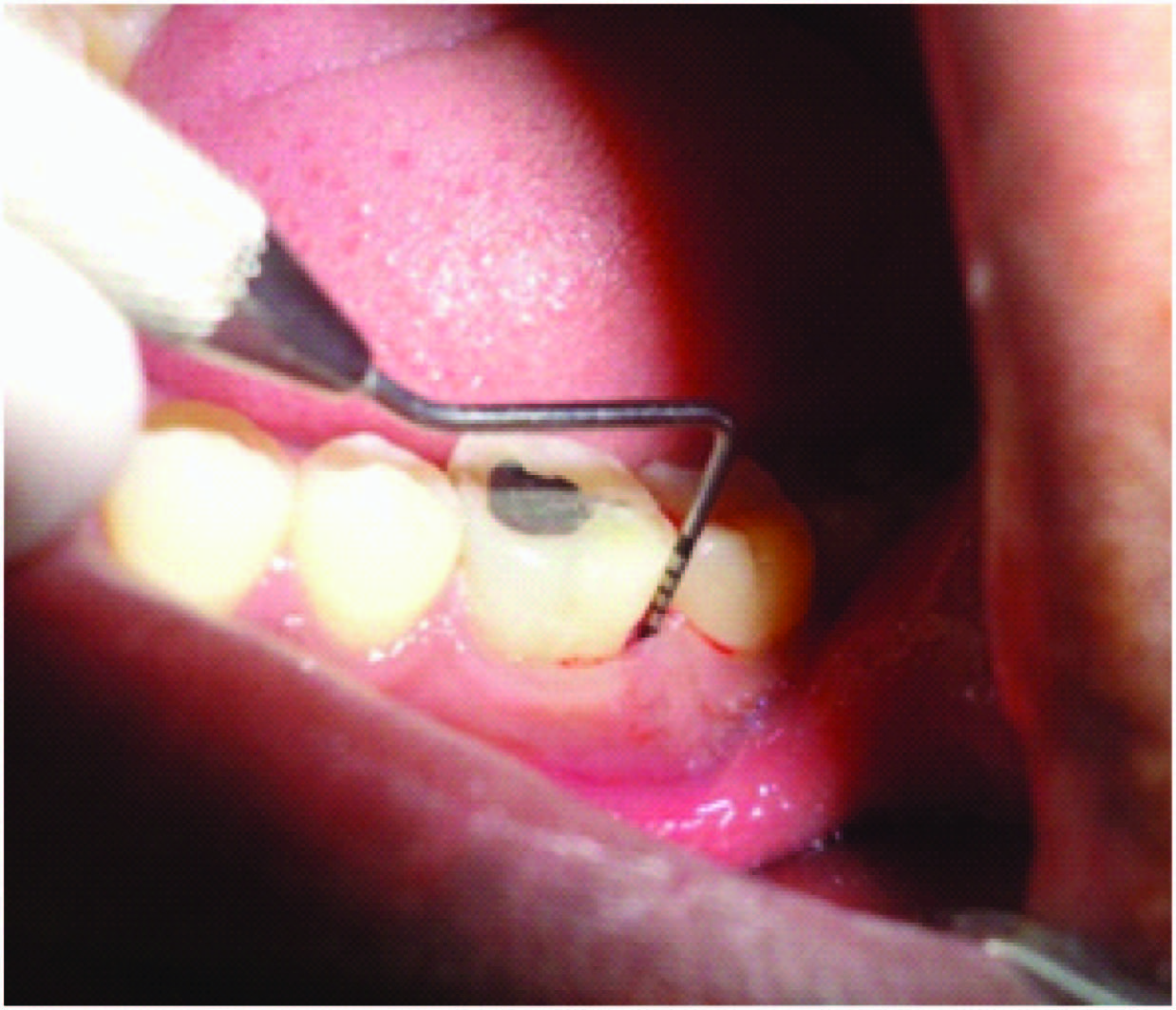
A 21-year-old male patient visited the Department of Periodontology at Government Dental College & Hospital, Vijayawada, Andhra Pradesh, India, complaining of mild soreness from mandibular left first molar tooth, especially when it was in function. His dental history revealed that root canal treatment had been performed five months previously. On clinical examination there was grade I mobility, clinical probing depth of 10mm on the disto labial aspect of mandibular left first molar measured using UNC-15 probe [Table/Fig-1]. An Intra Oral Periapical Radiograph (IOPA) of site was taken.
Clinical probing depth of 10mm,
The initial therapy, which included oral hygiene instruction, scaling, root planing, and occlusal adjustment, was completed.
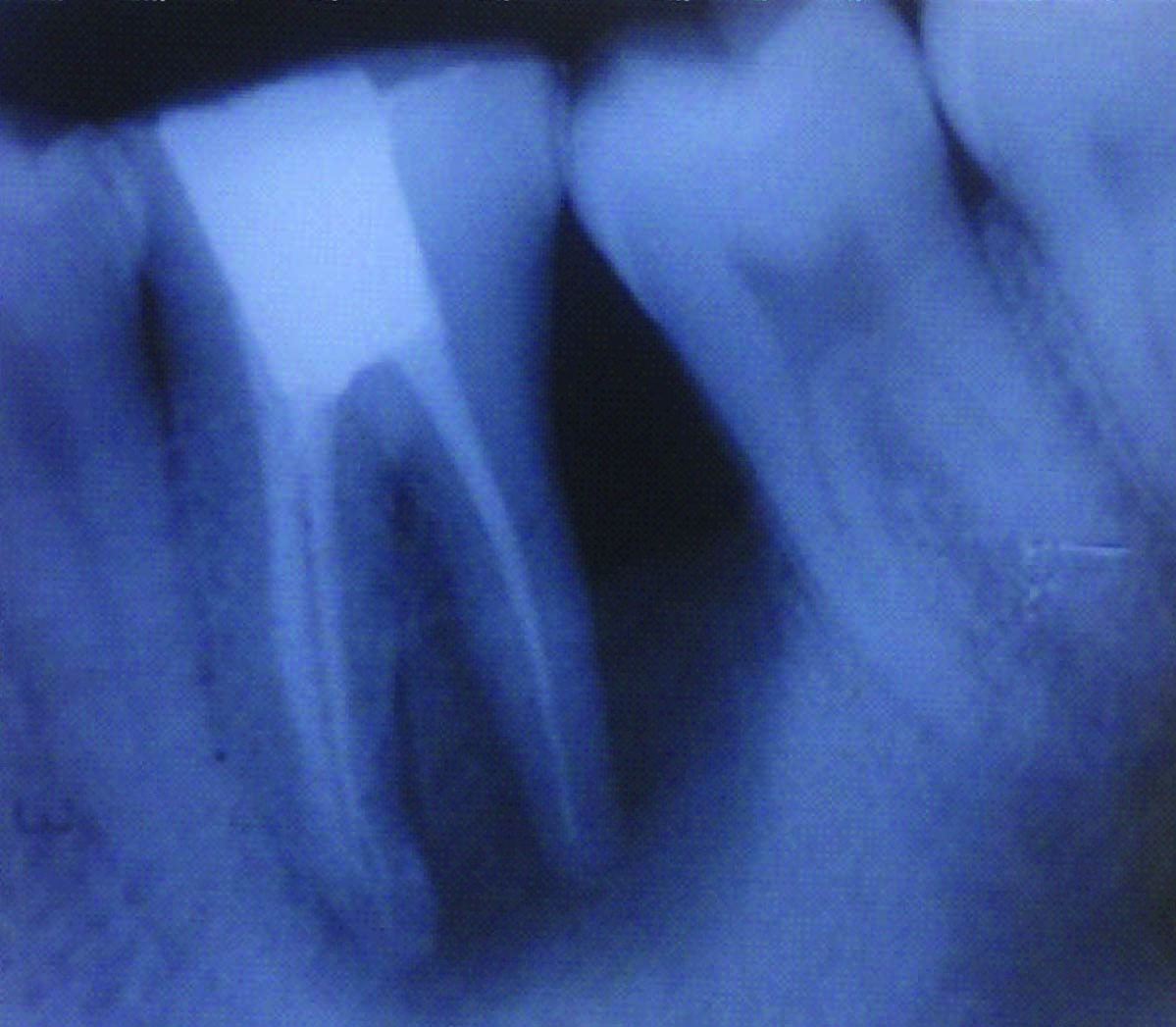
IOPA revealed root canal treated mandibular left first molar and more radiolucency around distal root when compared to mesial root [Table/Fig-2] indicating that some amount of bone destruction has been occurred around distal root and reduced interproximal bone height between left mandibular first and second molar. Although, IOPA produced acceptable details in the mesial-distal direction, the observation of details in the bucco-lingual dimension is inadequate as the size, morphology, and degree of furcation involvement and bone loss were not diagnosed precisely, the newly developed CBCT scan was decided to perform. The patient was given detailed explanation about the need for periodontal therapy and the fact that a CBCT system was to be used at the surgical site. It was performed and images were compared with that of IOPA.
Intraoral periapical Radiograph (IOPA) on the disto labial aspect of mandibular left first molar
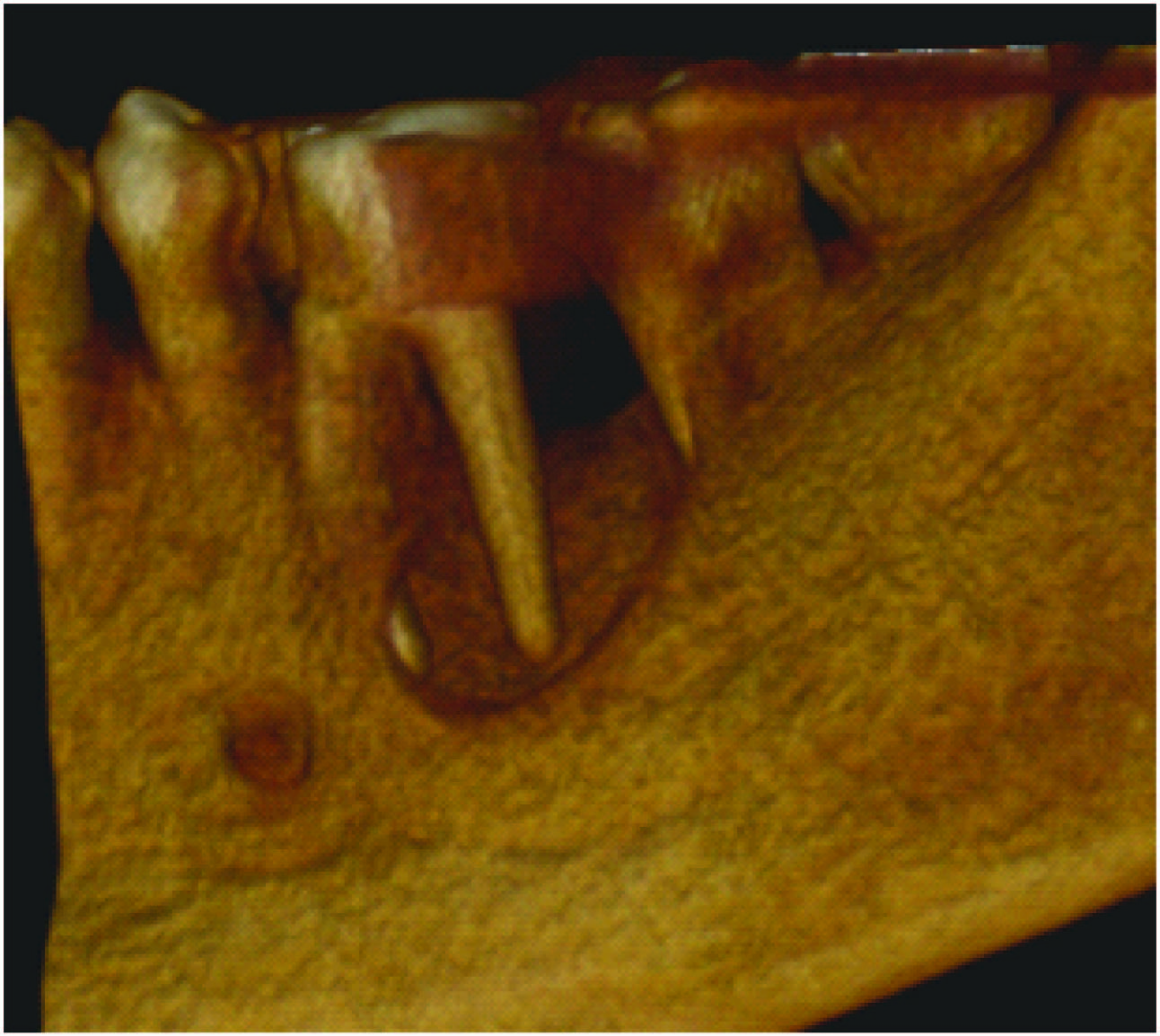
3D CBCT image [Table/Fig-3] showed loss of buccal cortical plate corresponding to the distal root of mandibular left first molar.
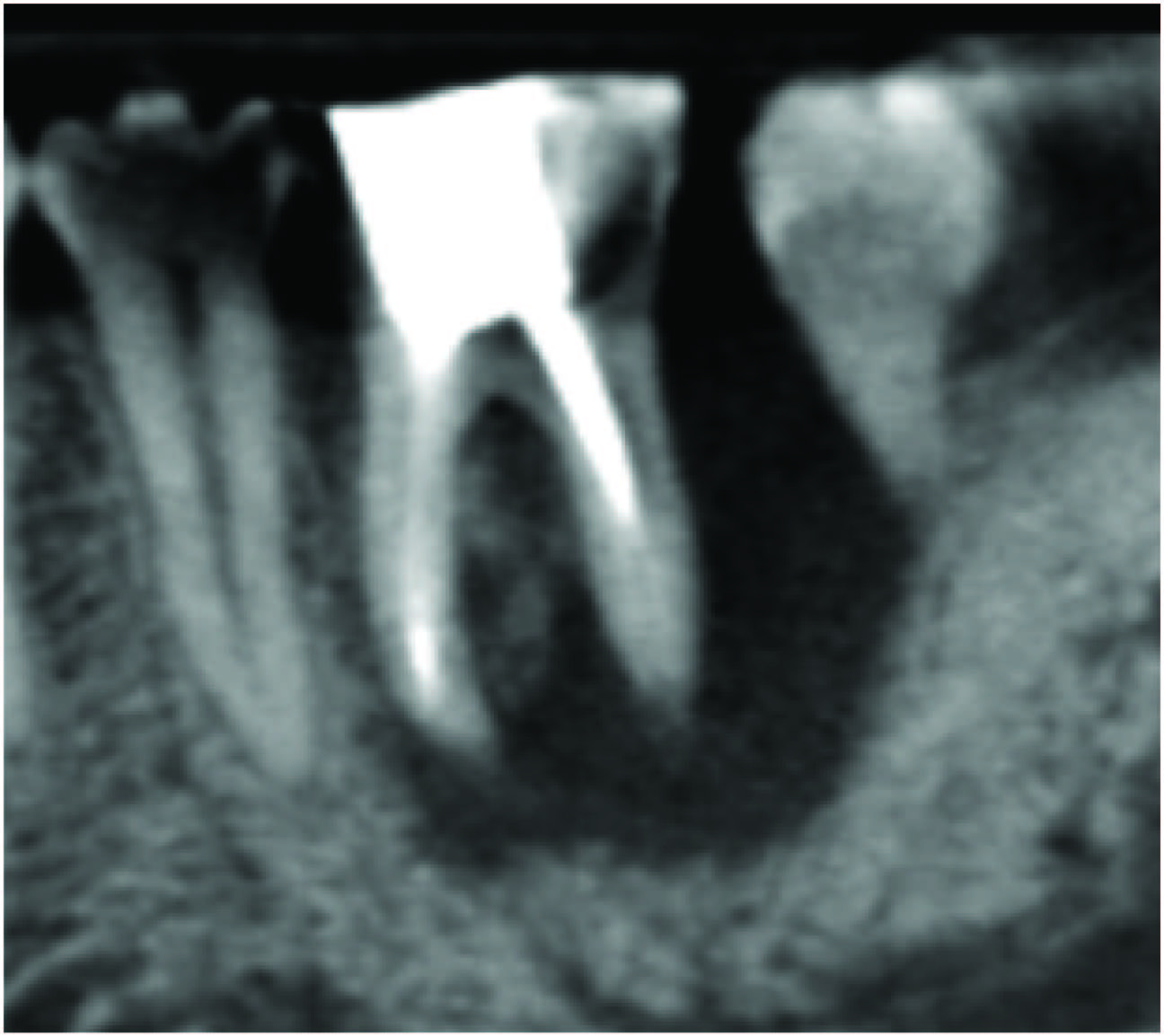
A sagittal CT image clearly shows location of the alveolar bone margins of mandibular left first molar. A vertical bone defect is found on the distal aspect on the distal root [Table/Fig-4].
A horizontal CT image (Axial plane) sharply depicts the morphology and distribution of each root. Radiolucency is noticeable around the distal root, and also furcation involvement between the roots [Table/Fig-5].

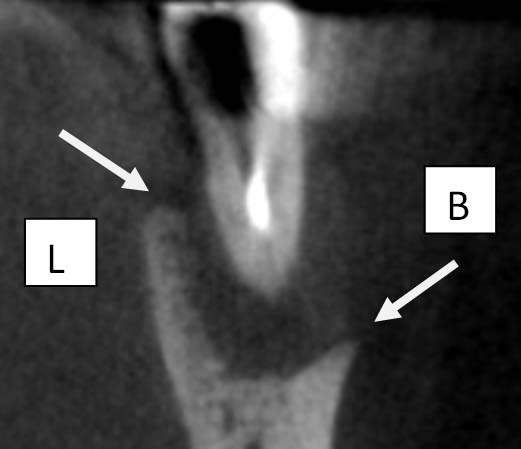
The size and morphology of furcation involvement are clearly evident in [Table/Fig-6]. The degree of furcation involvement in a buccal-to-lingual direction is well documented; the image provides evidence of definite involvement, but not through-and-through involvement [Table/Fig-6].
3D Image Coronal Plane( plane of the scan centered on middle of tooth mandibular left first molar)
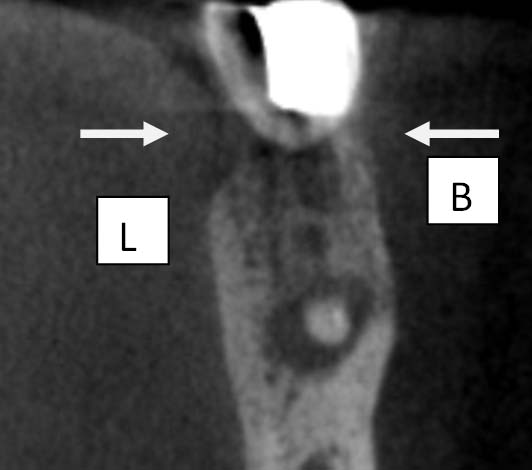
A buccolingual CT image(Coronal plane) obtained with the plane of the scan centered on distal root of mandibular left first molar tooth clearly showed reduced lingual cortical plate height and entire loss buccal cortical plate [Table/Fig-7].
3D Image coronal plane ( plane of the scan centered on distal root of tooth mandibular left first molar), B-Buccal, L-Lingual
From the CBCT findings, the defect on mandibular left first molar tooth was diagnosed as a Class II furcation involvement between the mesial and distal roots, and compromised bone support around its distal root with only lingual wall remaining supporting the apical third of distal root.
Based on the 3D images of CBCT findings, hemisection was the treatment of choice.
Discussion
Radiography plays an important role in periodontal diagnosis as they reveal the amount and type of damage caused to the alveolar bone. A number of intraoral and extra oral imaging modalities are available to assist in the management of the periodontal patient. Commonly used modalities include bitewing, periapical and panoramic radiography [1].
However, radiographs give a 2-D representation of 3-D structures, and their limitations have been well described [2,3]. There is ample research demonstrating that funnel-shaped or lingually located defects cannot be detected [4] and that destruction of the buccal plate can be undiagnosed or undistinguished from lingual defects [5].
In addition, the exact form of many periodontal defects including hemiseptum, intrabony defects, and furcation involvements cannot be determined from radiographs. Surgical entry is the best way in detecting the number of walls present or absent. These limitations reduce the sensitivity of IOPA and generally result in underestimating actual bone loss even when high quality images are produced.
To overcome the inherent difficulties of IOPA, 3-D image analysis by computed tomography (CT) has been introduced and is widely used for 3-D maxillofacial imaging in dentistry [6] but it is bulky and its use is expensive. However, recent advances have made it possible to design smaller machines that require lower doses. The cone-beam-type CT has a 2-D sensor and uses a cone-shaped x-ray beam in place of a fan-shape.
It gives the morphologic description of bone defects, measures intrabony defects in all the three planes (Sagittal, Axial, Coronal), pre-surgical implant planning for anatomic land marks, measures bone volume quality of hard tissue and in periodontal aspect to visualize interproximal defects, buccal and lingual defects, furcation defects, diagnosing dehiscence and fenestration defects, diagnostic and treatment-outcome evaluations of periodontitis, to evaluate postsurgical results of regenerative periodontal therapy, it can also be used as a new volumetric imaging method for measuring alveolar bone density, especially to assess healing after grafting [7]. Soft tissue CBCT is used for the measurement of gingival tissue and the dimensions of the dentogingival unit (to determine the relationships between gingival margin and the facial bone crest, gingival margin and the cemento-enamel junction (CEJ) and CEJ and facial bone crest) [8]. The width of the facial and palatal/lingual alveolar bone and the width of the facial and palatal/lingual gingival also could be measured [9].
CBCT and IOPA radiograph-comparision of advantages and disadvantages: CBCT provides 3D imaging which obtains cross-sectional and volumetric images with elimination of image deformity but of higher radiation dose, higher cost and occupies larger space compared to conventional radiography which provides 2D imaging with image superposition, distortion and magnification but of lower radiation dose, lower cost and smaller space requirement than CBCT [10].
Limitations of CBCT: When compared to IOPA or 2D imaging, CBCT has higher cost, effective radiation dose, lower resolution and lack of availability. Another important limitation of CBCT imaging is the presence of metal artifacts which are caused by metal and amalgam restorations and to a lesser extent, root-canal filling material and implants. Visualization of areas on the opposite side of an image is altered by streak artifacts which appear as linear hyperdensities [10].
Explanation and disclosure regarding radiation exposure risks, benefits and imaging modality alternatives to patients is required, as CBCT exposes them to ionizing radiation that may pose elevated risks to some patients (pregnant or younger patients) which has to be documented in the patient’s records [11].
Rees et al., [5] found that proximal osseous defects and furcation defects on the facial and lingual surfaces of multi-rooted teeth could be identified with a high degree of accuracy by their radiographic appearances. Conversely, lesions on the facial or lingual root surfaces are extremely difficult to recognize radiographically. In our patient, it was difficult to diagnose the furcation involvement of mandibular left first molar on IOPA.
It has been reported that destruction of the buccal plate cannot be distinguished from destruction of the lingual plate [4] when viewed in IOPA as in the present case.
The CT images of the furcation involvement combined with the intrabony defect of mandibular left first molar were clear and informative, indicating their potential clinical value. Digital images can be stored easily in computer memories. Patient data can be easily reconstructed for viewing from any direction at any time. This characteristic of computed tomography can reduce the radiation exposure of the patient. It also enables the patient’s images to be examined longitudinally.
Attempting to identify the most accurate method of evaluating hard tissue changes after periodontal therapy is an important task. To date, surgical reentry procedures appear to be the gold standard as it provides definitive information on morphology and dimensions of the intrabony defect before and after grafting. They are safe and have the advantage of being able to retreat the grafted area if complete defect resolution has not occurred. However, it has been suggested that the usual 6- to 12-month reentry procedure may be too early because osteoid may not be completely formed by eight months and that the maturation process of bone may take up to two years. Another disadvantage of using reentry procedures in clinical research is that the recruitment of study patients and approval from Institutional Review Boards may be more difficult than less invasive means of outcome assessment.
The image obtained with CBCT, combined with various techniques such as assessment of clinical probing depths, attachment levels, and alveolar bone levels, may increase our ability to determine the treatment outcome following periodontal treatment, without the use of a reentry procedure [12].
Authors evaluated CBCT images of artificially created furcation involvement of the second molars in pig mandibles and accuracy for furcation lesion detection ranged between 78% and 88% [13]. Walter et al., [14] reported that cone beam computed tomography (CBCT) and intrasurgical assessments of maxillary molar furcation involvement were found to be in substantial agreement and that CBCT enables an exact estimation and classification of furcation involvement as well as a visualization of the root morphologies with root proximities or root fusions as in the present case.
Considering the several advantages, limitations and risks of both modalities, though CBCT has higher cost and effective radiation dose, it provides more accurate details than IOPA especially in furcation lesions. More research using a large sample-size for periodontal bone level assessment and clinical studies with perioperative check-up as a gold standard for the bone defects should be conducted. This could further expand the applicability of CBCT in periodontal diagnosis.
Conclusion
The perception of images of excellent quality acquired using CBCT in the evaluation of alveolar bone loss, periodontal bone defects and furcation involvement could lead to a new approach in the evaluation of patients with periodontal disease and prove to be an excellent resource when deciding on the most appropriate therapy.
[1]. Feijo CV, Lucena JG, Kurita LM, Pereira SL, Evaluation of cone beam computed tomography in the detection of horizontal periodontal bone defects: an in vivo studyInt J Periodontics Restorative Dent 2012 32(5):e162-68. [Google Scholar]
[2]. Theilade J, An evaluation of the reliability of radiographs in the measurement of bone loss in periodontal diseaseJ Periodontol 1960 31:143-53. [Google Scholar]
[3]. Prichard J, Interpretation of radiographs in periodonticsInt J Periodontics Restorative Dent 1983 3(1):8-39. [Google Scholar]
[4]. Ramadan AB, Mitchell DF, A roentgenographic study of experimental bone destructionOral Surg Oral Med Oral Pathol 1962 15:934-43. [Google Scholar]
[5]. Rees T, Biggs NL, Collins CK, Radiographic interpretation of periodontal osseous defectsOral Surg Oral Med Oral Pathol Oral Radiol Endod 1971 2:141-53. [Google Scholar]
[6]. Ramachandran GN, Lakshminarayanan AV, Three dimensional reconstruction from radiographs and electron micrographs: Application convolutions instead of Fourier TransformsProc Natl Acad Sci 1971 68:2236-40. [Google Scholar]
[7]. Shah Monali A, Shah Sneha S, Dave Deepak H, CBCT - A Positive Amelioration In PeriodonticsNational Journal of Integrated Research in Medicine 2013 4(3):144-48. [Google Scholar]
[8]. Mohan R, Singh A, Gundappa M, Threedimensional imaging in periodontal diagnosis - Utilization of cone beam computed tomographyJ Indian Soc Periodontol 2011 15:11-17. [Google Scholar]
[9]. Januario AL, Barriviera M, Duarte WR, Soft tissue cone-beam computed tomography: A novel method for the measurement of gingival tissue and the dimensions of the dentogingival unitJ Esthet Restor Dent 2008 20:366-73. [Google Scholar]
[10]. Acar B, Kamburoglu K, Use of cone beam computed tomography in PeriodontologyWorld J Radiol 2014 6(5):139-47. [Google Scholar]
[11]. Clinical recommendations regarding use of cone beam computed tomography in orthodontics. Position statement by the American Academy of Oral and Maxillofacial RadiologyOral Surg Oral Med Oral Pathol Oral Radiol 2013 116(2):238-57. [Google Scholar]
[12]. Grimard BA, Hoidal MJ, Mills MP, Mellonig JT, Nummikoski PV, Mealey BL, Comparison of clinical, periapical radiograph, and cone-beam volume tomography measurement techniques for assessing bone level changes following regenerative periodontal therapyJ Periodontol 2009 80(1):48-55. [Google Scholar]
[13]. Umetsubo OS, Gaia BF, Costa FF, Cavalcanti MG, Detection of simulated incipient furcation involvement by CBCT: an in vitro study using pig mandiblesBraz Oral Res 2012 26:341-47. [Google Scholar]
[14]. Walter C, Weiger R, Zitzmann NU, Accuracy of three dimensional imaging in assessing maxillary molar furcation involvementJ Clin Periodontol 2010 37:436-41. [Google Scholar]